Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.108 no.1 Pretoria Jan. 2018
http://dx.doi.org/10.7196/samj.2018.v108i1.12686
RESEARCH
Anaemia, renal dysfunction and in-hospital outcomes in patients with heart failure in Botswana
J C MwitaI, II; M G M D MagafuIII; B OmechIV, V; M J DewhurstVI; Y MashallaVII
IMD, MMed, MSc; Department of Internal Medicine, Faculty of Medicine, University of Botswana, Gaborone, Botswana
IIMD, MMed, MSc; Department of Internal Medicine, Princess Marina Hospital, Gaborone, Botswana
IIIMD, MPHM, MPH, MSc, PhD; Department of Family Medicine and Public Health, Faculty of Medicine, University of Botswana, Gaborone, Botswana
IVMB ChB, MMed; Department of Internal Medicine, Faculty of Medicine, University of Botswana, Gaborone, Botswana
VMB ChB, MMed; Department of Internal Medicine, Princess Marina Hospital, Gaborone, Botswana
VIMD, FRCP; Department of Cardiology, University Hospital Hartlepool, UK
VIIMD, PhD; Department of Biomedical Sciences, Faculty of Medicine, University of Botswana, Gaborone, Botswana
ABSTRACT
BACKGROUND: Anaemia and renal dysfunction are associated with an increased morbidity and mortality in heart failure (HF) patients.
OBJECTIVE: To estimate the frequency and impact of anaemia and renal dysfunction on in-hospital outcomes in patients with HF.
METHODS: A total of 193 consecutive patients with HF admitted to Princess Marina Hospital, Gaborone, Botswana, from February 2014 to February 2015, were studied. Anaemia was defined as haemoglobin <13 g/dL for men and <12 g/dL for women. Renal dysfunction was defined by an estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m2, calculated by the simplified Modification of Diet in Renal Disease formula. The in-hospital outcomes included length of hospital stay and mortality.
RESULTS: The mean (standard deviation (SD)) age was 54.2 (17.1) years and 53.9% of the patients were men. The overall median eGFR was 75.9 mL/min/1.73 m2 and renal dysfunction was detected in 60 (31.1%) patients. Renal dysfunction was associated with hypertension (p=0.01), diabetes mellitus (p=0.01) and a lower haemoglobin level (p=0.008). The mean (SD) haemoglobin was 12.0 (3.0) g/dL and 54.9% of the patients were anaemic. Microcytic, normocytic and macrocytic anaemia were found in 32.1%, 57.5% and 10.4% of patients, respectively. The mean (SD) haemoglobin level for males was significantly higher than for females (12.4 (3.3) g/dL v. 11.5 (2.5) g/dL; p=0.038). Anaemia was more common in patients with diabetes (p=0.028) and in those with increased left ventricular ejection fraction (p=0.005). Neither renal dysfunction nor anaemia was significantly associated with the length of hospital stay or in-hospital mortality.
CONCLUSION: Anaemia and renal dysfunction are prevalent in HF patients, but neither was an independent predictor of length of stay or in-hospital mortality in this population. These findings indicate that HF data in developed countries may not apply to countries in sub-Saharan Africa, and call for more studies to be done in this region.
Anaemia and renal dysfunction are common comorbidities that are associated with morbidity and mortality in heart failure (HF) patients.[1,2] Depending on the definition used and population studied, the prevalence of anaemia in patients with HF ranges from 4% to 70%.[3-5] The presence of anaemia has been associated with increased length of hospital stay and in-hospital mortality in HF patients.[3] Some studies have reported that the impact of anaemia on mortality tends to occur a few months after discharge.[6] Causes of anaemia in HF include iron deficiency, renal insufficiency, haemodilution due to activation of renin-angiotensin-aldosterone and vasopressin systems, infections such as HIV, and drugs that interfere with the synthesis of endogenous erythropoietin, e.g. angiotensin-converting enzyme inhibitors.[7,8] Both renal dysfunction and HF-associated inflammatory activation are known to inhibit renal erythropoietin production, resulting in anaemia.[9]
Renal dysfunction, therefore, is associated with an increase in the prevalence of anaemia, and the two conditions are independent predictors of all-cause mortality in patients with HF.[2,4] Mortality risk is increased when both renal dysfunction and anaemia are present.[3] Both these conditions often coexist in HF patients.[4] Most of the studies on HF, however, have been from high-income countries (HICs), where older patients with multiple comorbid conditions are involved.[1,5] There is a paucity of information regarding the frequency of anaemia and renal dysfunction and their impact on in-hospital morbidity and mortality among patients with HF in sub-Saharan Africa (SSA). HF patients in SSA are usually younger (4th - 5th decade of life) than those in HICs (7th - 8th decade of life).[7,10] Our study aimed to estimate the frequency and impact of anaemia and renal dysfunction on in-hospital outcomes among HF patients admitted to Princess Marina Hospital (PMH), Gaborone, Botswana.
Methods
The study formed part of a larger observational study that characterised the HF population at PMH, the largest referral hospital in Botswana.[7] Included in the study were adult patients (>18 years) admitted between February 2014 and February 2015, whose serum creatinine and haemoglobin results were available. No formal sample size calculations were done. HF was defined according to the criteria of the European Society of Cardiology, and decompensated HF in patients with a previous HF diagnosis and in those with new-onset HF was included. [11]
Demographic and clinical characteristics documented at admission include gender, age, hypertension, HIV serostatus, diabetes mellitus, and functional class according to the New York Heart Association (NYHA) criteria. Complete blood count, serum electrolyte, urea, creatinine and uric acid tests were performed on all enrolled patients. Left ventricular ejection fraction (LVEF) was calculated from the left ventricular volumes obtained at end-diastole and end-systole using the modified biplane Simpson's rule in the apical four-chamber and two-chamber views.[12] LVEF <45% was used to define significant left ventricular (LV) systolic dysfunction, whereas patients with LVEF >45% were classified as having HF with preserved ejection fraction.
Renal dysfunction was diagnosed using an estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m2 body surface area on admission, calculated by the simplified Modification of Diet in Renal Disease formula.[13] Anaemia was defined as a haemoglobin level <13 g/dL for men and <12 g/dL for women.[14] Hospital length of stay (LOS) and in-hospital mortality were assessed for each participant. LOS was defined as the number of days from hospital admission to discharge.
Statistical analysis
Data were analysed using SPSS version 23.0 (IBM Corp., USA). Continuous variables were presented as means (standard deviations (SDs)) or medians and interquartile ranges (IQRs). For non-continuous variables, absolute and relative frequencies (%) were used. Comparisons between continuous variables were performed using Student's f-test or the Kruskal-Wallis test. Associations between categorical variables were tested with the use of contingency tables and calculations of Pearson's χ2, and p<0.05 was considered statistically significant. Multivariate analysis was performed using binary logistic regression. Covariate selection was based on plausibility and p<0.05 on univariate analyses.
Ethical considerations
The study was granted ethical clearance by the University of Botswana, the Ministry of Health and PMH Institutional Review Boards (ref. no. PPME 13/18/1 VIII (264)). All patients provided informed consent before participation.
Results
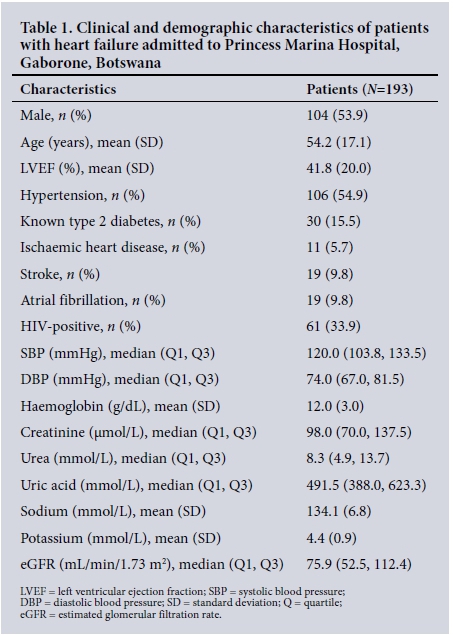
The study included 193 patients, mostly (98.4%) black Africans (Table 1). The patients' ages ranged between 20 and 89 years, with a mean (SD) of 54.2 (17.1) years. All patients were symptomatic and the majority (77.5%) presented in NYHA III or IV functional classes. Overall, the median (IQR) systolic and diastolic blood pressures were 120 (104 - 133) mmHg and 74 (67 - 82) mmHg, respectively. More than half (54.9%) of patients were hypertensive. A prior diagnosis of diabetes mellitus was present in 30 (15.5%) and often coexisted with hypertension. The mean LVEF was 41.7%, and about two-thirds (64.8%) of patients had HF with systolic dysfunction (LVEF <45%).
Renal dysfunction
The median serum creatinine was 98.0 μmol/L - significantly higher in males than in females (105.0 μmol/L v. 87.7 μmol/L; p=0.031). The overall median (quartile) eGFR was 75.9 (Q1 52.5, Q3 112.4) mL/min/1.73 m2, with no significant gender differences. Renal dysfunction was detected in 60 (31.1%) patients (Table 2). In bivariate analysis, patients with renal dysfunction were more likely to be diabetic, hypertensive, and older, and had significantly greater serum creatinine, potassium, urea and uric acid concentrations than those with an eGFR >60 mL/min/1.73 m2. In multiple logistic regression analysis, patients with renal dysfunction were likely to have hypertension (odds ratio (OR) 2.80; 95% confidence interval (CI) 1.28 - 6.12; p=0.01), diabetes (OR 3.09; 95% CI 1.23 - 7.76; p=0.01), and lower haemoglobin levels (OR 0.85 g/dL; 95% CI 0.76 -0.96; p=0.008). Renal dysfunction was not associated with length of hospital stay (p=0.292) or in-hospital all-cause mortality (p=0.217).
Anaemia
Overall, the mean (SD) haemoglobin was 12.0 (3.0) g/dL and about half (54.9%) of the patients were anaemic (Table 3). Microcytic, normocytic and macrocytic anaemia were found in 32.1%, 57.5% and 10.4% of patients, respectively. Of the 11 patients with macrocytic anaemia, 10 (90.1%) were HIV-positive and receiving antiretroviral medications. The mean haemoglobin level for males was significantly higher than for females (12.4 (3.3) g/dL v. 11.5 (2.5) g/dL; p=0.038). Nonetheless, the proportion of anaemic patients did not differ by gender (p=0.53).
Bivariate analysis showed that patients with anaemia were more likely to have a higher LVEF or type 2 diabetes mellitus. Moderate to severe anaemia (haemoglobin <10 g/dL) was more common among those with renal dysfunction than in those without the condition (57.8% v. 23.0%; p<0.001).
The multiple logistic regression analysis indicated that patients with anaemia were likely to have diabetes (OR 2.68; 95% CI 1.12 - 6.45; p=0.028) and a higher LVEF (OR 1.02; 95% CI 1.01 - 1.04; p=0.005). Anaemia was not associated with LOS (p=0.101) or in-hospital all-cause mortality (p=0.496).
Anaemia and an eGFR <60 mL/min/1.73 m2 coexisted in 38 (19.6%) patients and was not associated with an increased in-hospital all-cause mortality (p=0.61) or duration of hospital stay (p=0.153).
Discussion
To the best of our knowledge, this is the first observational study of anaemia and renal failure among patients with HF admitted to a hospital in Botswana. We found a high proportion of anaemia and renal dysfunction among patients with HF in this setting (54.9% and 31.1%, respectively). Neither anaemia nor renal dysfunction was significantly associated with hospital LOS (p=0.101) or in-hospital all-cause mortality (p=0.496). There was no effect on either LOS or in-hospital mortality. Remarkably, our cohort comprised younger patients (mean 54 years) compared with patients presenting in their 7th and 8th decades of life in the developed world.[10] This finding may in part explain why anaemia and renal dysfunction had a neutral effect on hospital outcomes, unlike in HICs. As our patients were young, they were likely to have fewer comorbidities and could possibly compensate better for anaemia and renal dysfunction than the older HF cohorts in HICs.
The prevalence of anaemia among patients with HF varies between studies. Using the World Health Organization definition of anaemia in patients with HF, prevalence rates of 50 - 70% have been reported.[4-6,15] Most of these studies were performed in HICs and involved patients who are not only older than those in our setting, but also predominantly white.[15] We observed a prevalence rate >13.5% previously reported among patients with idiopathic cardiomyopathy in South Africa.[16] It was also higher than the 42% reported in a study in Brazzaville, Congo, even though the difference may be attributed to the use of a lower cut-off value for anaemia (haemoglobin level <12 g/dL for men and <11 g/dL for women).[17] The proportion of patients with anaemia in this study is lower than the 63.3% reported in Uganda.[18] Direct comparison of different studies is nevertheless difficult owing to the variation of both anaemia cut-off values and the populations studied. In HIC populations, anaemia is caused by age-related chronic diseases and renal dysfunction.[4,15,19] Our population was young and included a higher proportion of females of reproductive age. The prevalence of anaemia among non-pregnant women in Africa is about 41%, the highest in the world.[20] Even though the prevalence of anaemia was high among HF patients in our study, its significance for public health screening remains doubtful owing to lack of effect in hospital outcomes. It is therefore imperative that each HF patient with anaemia is recognised by healthcare workers in the hospital setting and managed accordingly.
Low haemoglobin levels have been reported to be an independent predictor of mortality.[2,21] While in-hospital mortality and LOS were not associated with anaemia in our study, we have previously reported an increase in 6-month mortality when these patients were followed up.[7] A similar finding, where in-hospital mortality was similar for anaemic and non-anaemic patients but with a higher mortality 1 year after discharge, has previously been reported by De Amicis et al.'61 The median hospital LOS in our study was not significantly longer in anaemic patients than in non-anaemic participants (8.0 days v. 9.5 days; p=0.292). Our observation is in agreement with the findings of De Amicis et al[6]that anaemia is not associated with an increase in hospital LOS. Our result, however, differs from that of Caughey et al.,[5] who found an increase in hospital mortality and LOS among patients with acute decompensated HF. The discrepancy in these findings is possibly owing to differences in the characteristics of HF cohorts studied. The young age of our patients may partially protect them from increased mortality or prolonged LOS.
Type 2 diabetes mellitus, a high LVEF or HF with preserved ejection fraction has been reported to be associated with anaemia in HF.[6,21] Our study demonstrated a significant association between anaemia with type 2 diabetes and LVEF after adjusting for other factors. Diabetes mellitus has been associated with anaemia of chronic disease, a common presentation among patients with HF.[22] Other known causes of anaemia in HF include iron deficiency, renal insufficiency, haemodilution due to activation of renin-angiotensin-aldosterone and vasopressin systems, infections such as HIV, and drugs that interfere with the synthesis of endogenous erythropoietin, e.g. angiotensin-converting enzyme inhibitors.'7,81 As our study included patients with new-onset HF, who enrolled before the initiation of HF medications, haemodilution is a possible cause of anaemia in this group. Although about a third of the study participants were HIV-infected, the infection was not significantly associated with anaemia. Macrocytic anaemia was, however, more common among HIV-infected patients, most likely due to the use of azidothymidine.[23]
We found that a third of participants had renal dysfunction, comparable to the findings of the sub-Saharan Africa Survey of Heart Failure (THESUS-HF), in which 30.6% of HF patients had renal dysfunction when admitted to hospital.[24] Similarly, in a meta-analysis of 65 324 HF patients, moderate to severe renal impairment was found in up to 29% of all patients, the prevalence being lower in outpatients than hospitalised patients.[1] In addition to structural renal abnormalities related to hypertension, diabetes or atherosclerosis, renal dysfunction in HF patients may result from renal hypoperfusion caused by haemodynamic, neurohumoral and inflammatory factors.[9,25] We also found that systolic and diastolic blood pressures were significantly high among patients with reduced renal function, possibly explained by the underlying hypertension. Hypertension and diabetes mellitus (both risk factors for kidney
disease) were common in patients with renal dysfunction.[26] This is consistent with findings in previous studies that suggested a progressive increase in the prevalence of hypertension and diabetes, with reduction in kidney function.[26] Our study also confirmed the findings that a decline in renal function is associated with an increase in the prevalence of anaemia in HF patients.[4] Both renal dysfunction and HF-associated inflammatory activation inhibit renal erythropoietin production.[9] Moderate to severe anaemia (haemoglobin <10 g/dL) was more commonly seen among patients with renal dysfunction than in those without.
Renal dysfunction has been associated with longer hospital stay and increased hospital mortality in patients with HF.[1,24,27] We found an insignificant increase in mortality and length of hospital stay in patients with renal dysfunction, possibly owing to our sample size. Furthermore, estimation of renal function was done at enrolment, using a single (baseline) serum creatinine value. In the setting of acute or decompensated HF, it is possible to misclassify patients with unstable renal dysfunction who recover with improvement in HF. As our participants were young, they were more likely to have unstable renal dysfunction, and potentially recovered without any effect on mortality or length of hospital stay.
Conclusion
The current study has demonstrated a high frequency of anaemia and renal dysfunction among HF patients admitted to a tertiary hospital in Botswana. Both anaemia and renal dysfunction were, however, not predictors of LOS or in-hospital mortality. There is a need for large studies in SSA to confirm findings from HICs, as data from western cohorts may not necessarily apply to SSA because of the differences in HF populations.
Study limitations
This study was undertaken in a small city (Gaborone) and therefore limited by the relatively small number of patients. As this was part of previous research, there was no sample size calculation. However, the study provides useful insights that open new avenues for future studies of HF. All deaths were assumed to be attributable to HF, which is likely to be an overestimation because of other significant medical comorbidities that were highly prevalent in our patients.
Acknowledgements. We would like to thank the patients and their relatives for their co-operation. Special thanks to the nursing staff of the medical wards for their assistance with the study.
Author contributions. JCM conceived and supervised the study, recruited patients, performed the echocardiographic studies, interpreted the data and wrote the manuscript. YM, BO, MJD and MGMDM participated in the design of the study and critically reviewed the manuscript. All authors read and approved the final article.
Funding. This study was supported by a grant from the University of Botswana Office of Research and Development (ORD), Round 25.
Conflicts of interest. None.
References
1. Smith GL, Lichtman JH, Bracken MB, et al. Renal impairment and outcomes in heart failure: Systematic review and meta-analysis. J Am Coll Cardiol 2006;47(10):1987-1996. https://doi.org/10.1016/j.jacc.2005.11.084 [ Links ]
2. Horwich TB, Fonarow GC, Hamilton MA, MacLellan WR, Borenstein J. Anemia is associated with worse symptoms, greater impairment in functional capacity and a significant increase in mortality in patients with advanced heart failure. J Am Coll Cardiol 2002;39(11):1780-1786. https://doi.org/10.1016/S0735-1097(02)01854-5 [ Links ]
3. Al-Ahmad A, Rand WM, Manjunath G, et al. Reduced kidney function and anemia as risk factors for mortality in patients with left ventricular dysfunction. J Am Coll Cardiol 2001;38(4):955-962. https://doi.org/10.1016/S0735-1097(01)01470-X [ Links ]
4. Lindenfeld J. Prevalence of anemia and effects on mortality in patients with heart failure. Am Heart J 2005;149(3):391-401. https://doi.org/10.1016/j.ahj.2004.08.039 [ Links ]
5. Caughey MC, Avery CL, Ni H, et al. Outcomes of patients with anemia and acute decompensated heart failure with preserved versus reduced ejection fraction (from the ARIC study community surveillance). J Am Coll Cardiol 2014;114(12):850-1854. https://doi.org/10.1016/j.amjcard.2014.09.024 [ Links ]
6. De Amicis MM, Chivite D, Corbella X, Cappellini MD, Formiga F. Anemia is a mortality prognostic factor in patients initially hospitalized for acute heart failure. Intern Emerg Med 2017;6:749-756. https://doi.org/10.1007/s11739-017-1637-5 [ Links ]
7. Mwita J, Dewhurst M, Magafu M, et al. Presentation and mortality of patients hospitalised with acute heart failure in Botswana. Cardiovasc J Afr 2017;28(2):112-117. https://doi.org/10.5830/CVJA-2016-067 [ Links ]
8. Chatterjee B, Nydegger UE, Mohacsi P. Serum erythropoietin in heart failure patients treated with ACE-inhibitors or AT1 antagonists. Eur J Heart Fail 2000;2(4):393-398. https://doi.org/10.1016/S1388-9842(00)00110-0 [ Links ]
9. Metra M, Cotter G, Gheorghiade M, Dei Cas L, Voors AA. The role of the kidney in heart failure. Eur Heart J 2012;33(17):2135-2142. https://doi.org/10.1093/eurheartj/ehs205 [ Links ]
10. Nieminen MS, Brutsaert D, Dickstein K, et al. EuroHeart Failure Survey II (EHFS II): A survey on hospitalized acute heart failure patients: Description of population. Eur Heart J 2006;27(22):2725-2736. https://doi.org/10.1093/eurheartj/ehl193 [ Links ]
11. McMurray JJ, Adamopoulos S, Anker SD, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012. Eur J Heart Fail 2012;14(8):803-869. https://doi.org/10.1093/eurjhf/hfs105 [ Links ]
12. Picard MH, Adams D, Bierig SM, et al American Society of Echocardiography recommendations for quality echocardiography laboratory operations. J Am Soc Echocardio 2011;24(1):1-10. https://doi.org/10.1016/j.echo.2010.11.006 [ Links ]
13. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Ann Intern Med 1999;130(6):461-470. https://doi.org/10.7326/0003-4819-130-6-199903160-00002 [ Links ]
14. World Health Organization. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and mineral nutrition information system. Geneva: WHO, 2011. [ Links ]
15. Opasich C, Cazzola M, Scelsi L, et al. Blunted erythropoietin production and defective iron supply for erythropoiesis as major causes of anaemia in patients with chronic heart failure. Eur Heart J 2005;26(21):2232-2237. https://doi.org/10.1093/eurheartj/ehi388 [ Links ]
16. Inglis SC, Stewart S, Papachan A, et al. Anaemia and renal function in heart failure due to idiopathic dilated cardiomyopathy. Eur J Heart Fail 2007;9(4):384-390. https://doi.org/10.1016/j.ejheart.2006.10.013 [ Links ]
17. Ikama MS, Nsitou BM, Kocko I, Mongo NS, Kimbally-Kaky G, Nkoua JL. Prevalence of anaemia among patients with heart failure at the Brazzaville University Hospital: Cardiovascular topics. Cardiovasc J Afr 2015;26(3):140-142. https://doi.org/10.5830/CVJA-2015-021 [ Links ]
18. Kuule JK, Seremba E, Freers J. Anaemia among patients with congestive cardiac failure in Uganda: Its impact on treatment outcomes. S Afr Med J 2009;99(12):876-880. [ Links ]
19. Villacorta H, Saenz-Tello BF, Santos EBD, et al. Renal dysfunction and anemia in patients with heart failure with reduced versus normal ejection fraction. Arquivos Brasileiros de Cardiologia 2010;94(3):378-384. https://doi.org/10.1590/S0066-782X2010000300016 [ Links ]
20. Stevens GA, Finucane MM, de-Regil LM, et al. Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995 - 2011: A systematic analysis of population-representative data. Lancet Glob Health 2013;1(1):e16-e25. https://doi.org/10.1016/S2214-109X(13)70001-9 [ Links ]
21. Felker GM, Gattis WA, Leimberger JD, et al. Usefulness of anemia as a predictor of death and rehospitalization in patients with decompensated heart failure. Am J Cardiol 2003;92(5):625-628. https://doi.org/10.1016/S0002-9149(03)00740-9 [ Links ]
22. Ezekowitz JA, McAlister FA, Armstrong PW. Anemia is common in heart failure and is associated with poor outcomes. Circulation 2003;107(2):223-225. https://doi.org/10.1161/01.CIR.0000052622.51963.FC [ Links ]
23. Richman DD, Fischl MA, Grieco MH, et al. The toxicity of azidothymidine (AZT) in the treatment of patients with AIDS and AIDS-related complex. N Engl J Med 1987;317(4):192-197. https://doi.org/10.1056/NEJM198707233170402 [ Links ]
24. Sani MU, Davison BA, Cotter G, et al. Renal dysfunction in African patients with acute heart failure. Eur J Heart Fail 2014;16(7):718-728. https://doi.org/10.1002/ejhf.103 [ Links ]
25. Stevenson LW, Nohria A, Mielniczuk L. Torrent or torment from the tubules? J Am Coll Cardiol 2005;45(12):2004-2007. [ Links ]
26. Ahmed A, Campbell RC. Epidemiology of chronic kidney disease in heart failure. Heart Fail Clin 2008;4(4):387-399. https://doi.org/10.1016/j.hfc.2008.03.008 [ Links ]
27. Heywood JT, Fonarow GC, Costanzo MR, et al. High prevalence of renal dysfunction and its impact on outcome in 118 465 patients hospitalized with acute decompensated heart failure: A report from the ADHERE database. J Cardiac Fail 2007;13(6):422-430. https://doi.org/10.1016/j.cardfail.2007.03.011 [ Links ]
 Correspondence:
Correspondence:
J C Mwita
mwitajc@ub.ac.bw
Accepted 31 July 2017














