Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.107 n.11 Pretoria Nov. 2017
http://dx.doi.org/10.7196/samj.2017.v107i11.12484
RESEARCH
Endoscopy services in KwaZulu-Natal Province, South Africa, are insufficient for the burden of disease: Is patient care compromised?
E LootsI, II; D L ClarkeIII, IV, V; K NewtonVI; C J MulderVII
IMB ChB, FCS (SA), Cert Gastroenterology (SA) Surg; Department of Surgery, Inkosi Albert Luthuli Central Hospital, Durban, South Africa
IIMB ChB, FCS (SA), Cert Gastroenterology (SA) Surg; Department of Surgery, School of Clinical Medicine, College of Health Sciences, Nelson R Mandela School of Medicine, Durban, South Africa
IIIMB ChB, MPhil, MBA, MSc, PhD; Department of Surgery, School of Clinical Medicine, College of Health Sciences, Nelson R Mandela School of Medicine, Durban, South Africa
IVMB ChB, MPhil, MBA, MSc, PhD; Department of General Surgery, Grey's Hospital, Pietermaritzburg, South Africa
VMB ChB, MPhil, MBA, MSc, PhD; Department of Surgery, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
VIMB ChB, FCP (SA); Department of Gastroenterology, Inkosi Albert Luthuli Central Hospital and School of Clinical Medicine, College of Health Sciences, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
VIIPhD; Department of Hepatogastroenterology, VU University Medical Centre Amsterdam, Netherlands
ABSTRACT
BACKGROUND. Endoscopy services are central to the diagnosis and management of many gastrointestinal (GI) diseases.
OBJECTIVE. To evaluate the adequacy of endoscopy services in the public sector hospitals of KwaZulu-Natal (KZN) Province, South Africa, in 2016.
METHODS. A cross-sectional study was performed using a questionnaire completed by the clinical heads of endoscopy units in the public hospitals in KZN.
RESULTS. The heads of 11 of the 12 endoscopy units responded. Two units were in tertiary-level hospitals and nine in regional hospitals. A total of 22 353 endoscopic procedures were performed annually, averaging 2 032 cases per annum per centre; they were performed by 89 endoscopists, of whom 72 (80.1%) were general surgeons. There were 0.06 registered gastroenterologists (GEs) per 100 000 population. Each endoscopist performed an average of 263 endoscopies per annum. There were 1.18 endoscopy rooms available per unit, and two units had on-site fluoroscopy available. The average waiting period for an upper endoscopy was 27 (range 7 - 60) days, for colonoscopy 29 (range 7 - 90) days and for duodenoscopy/endoscopic retrograde cholangiopancreatography 13 (range 4 - 20) days. This included patients with alarm symptoms for GI cancers. Equipment breakages interrupted most services, except for one hospital that had a service contract. Unit heads cited lack of equipment, trained staff and maintenance contracts as major shortcomings.
CONCLUSIONS. Endoscopy units in KZN are not adequately equipped to deal with the endoscopy workload and services are plagued by frequent disruptions, which impact negatively on service delivery. There is a need to train more GEs. Patient care is compromised in these public hospitals.
Gastrointestinal (GI) symptoms have varied presentations in common diseases encountered in both general and specialist practice. The spectrum of GI disease varies around the world. Traditionally low- and middle-income countries (LMICs) are most commonly burdened by infectious diseases of the GI system. Diarrhoeal diseases, hepatitis B virus (HBV) and Helicobacter pylori are major contributors to morbidity and mortality.[1] Non-infectious diseases, especially GI cancers such as oesophageal cancer and hepatocellular carcinoma, are highly prevalent on the east coast of South Africa (SA), and cancers often present at an advanced stage.[2,3]
Clinical guidelines for the diagnosis and treatment of GI disease are usually developed in high-income settings and then applied in clinical practice in low- and middle-income settings.[4] These guidelines often depend on advanced endoscopic and ultrasonic techniques, utilising computer software for managing basic data and documentation.[5] However, the applicability of these innovative modalities and advances to practice in LMICs is unclear. Attempts to translate these guidelines into practice in LMICs are often hampered by infrastructural and human resource constraints.[6,7] Endoscopy services and computerised data collections form the backbone of gastroenterology services and are often poorly developed in LMICs.
Context remains important, and recognising the different working conditions in which guidelines are implemented is an important step towards narrowing the gap between gastroenterology in rich and poor countries. SA has a dual healthcare system consisting of a privately funded and a publicly funded health system. The system is based on the values and principles of primary healthcare, but major discrepancies prohibit equal access for the majority of the population. In KZN the publicly funded healthcare system provides access to healthcare to an estimated 8.5 million people (~85% of the KZN population).[8] Estimations suggest that the local need for oesophagogastroduodenoscopy (OGD) is 1 per 100 population per year and for colonoscopy 1 per 250 population per year.[9] There should therefore be capacity for 80 000 endoscopies a year in the public sector in this region.[9]
The number of gastroenterologists (GEs) per 100 000 is 3.9 in the USA, 2.1 in Australia and 1.41 in the UK, all high-income countries (HICs).[10.11] In SA there are 0.12 per 100 000,[12] which is well below the recommended minimum of 0.22 per 100 000.[10] The World Gastroenterology Organisation recommends one GE for every 50 000 population.[13] Based on this number, at least 1 000 GEs are required in SA, which translates to ~100 in the KZN public sector.
A functional endoscopy unit requires at least three endoscopy suites (otherwise a minimum of two rooms) for units carrying out >3 000 endoscopies per year with three dedicated endoscopists.[4] The National Health Service (NHS) in the UK has set the benchmark of a maximum 2-week delay from the onset of alarm symptoms to endoscopy, referred to as the two-week rule (TWR). Their average waiting times are 1.2 weeks for urgent cases and 3.4 weeks for non-urgent cases, with a range of 1 - 6 weeks.[14] This endpoint is heavily influenced by the number of trained endoscopists and facilities available.
Objective
To audit the GI endoscopy services in KZN and compare these with the current guidelines for infrastructure, number of endoscopists and number of GEs and the effect the available resources and manpower have on achieving a TWR.
Methods
A cross-sectional study of the KZN hospitals providing an endoscopy service was performed using a questionnaire addressed to the head of each endoscopy unit (HOU). The questionnaire was sent via email in August 2016 to the head of endoscopy services in each hospital in the province that was eligible for inclusion. The HOUs were required to consent to and complete the questionnaire based on historical facility data over the past year. The questionnaire was devised to gather information on endoscopy services in KZN by using a combination of quantitative and qualitative questions.
The format of the questionnaire was designed to gather information on the number of endoscopists and the registered qualification (e.g. general surgeon, medical or surgical GE, etc.) of each endoscopist in that particular unit. Information on the institutional facilities focused on the endoscopic equipment and the instruments available to perform specific procedures, e.g. endoscopic injection and endoscopic banding. The final part consisted of qualitative questions on facilities or equipment that the HOU perceived would potentially improve the service in their specific endoscopic unit. Descriptive data were analysed and processed using Microsoft Excel, 2011 version (Microsoft, USA).
Ethics approval
Ethics approval was obtained from the University of KwaZulu-Natal Biomedical Research Ethics Committee (ref. no. BE051/16) and the KZN Department of Health (DoH) (ref. no. KZ 2016 RP37 97).
Results
Facilities, staff and waiting lists
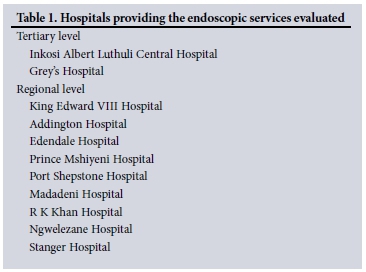
The questionnaire was sent to the 12 KZN hospitals that perform endoscopy, and 11 HOUs responded. Two hospitals were tertiary level and nine were regional (Table 1). The non-responding hospital was a district-level institution. The main central referral hospital was the only hospital with both equipment and facility maintenance contracts, which impacted favourably on equipment repair times. The number of endoscopies performed at this hospital was limited by contract stipulations based on agreed terms and conditions stipulated between the DoH and the private partner. The implication is that only a limited number of endoscopic procedures may be performed annually, as negotiated in advance. For instance, at the time of data collection 13 endoscopic retrograde cholangiopancreatographies (ERCPs) could be booked per week.
An estimated 22 353 endoscopic procedures were performed across all the hospitals annually, averaging 2 032 cases per annum per centre. There was a total of 89 active endoscopists, which equates to about 1 per 100 000 population. Of these, 43 were general surgeons, 29 surgery medical officers, 8 medical GEs, 8 surgical GEs and 1 a general physician. General surgeons and surgery medical officers represented 89.9% of all active endoscopists. There were 0.06 trained medical and surgical GEs per 100 000 population. An average of 263 endoscopies were performed per endoscopist per year, and 1 597 endoscopies were performed per endoscopy room per year. The total number of operational endoscopes available for the 11 units was as follows: 30 upper endoscopes, 19 colonoscopes, 10 duodenoscopes, 3 endoscopic ultrasounds, 1 balloon-assisted enteroscope and 1 capsule endoscopy facility. Each unit had an average of 1.18 endoscopy rooms. The average waiting time for all booked cases, including those with alarm symptoms, was as follows: upper endoscopy 27 (range 7 - 60) days, colonoscopy 29 (range 7 - 90) days and duodenoscopy/ERCP 13 (range 4 -20) days. If the main teaching hospital endoscopic facilities are excluded, an average of 616 endoscopies per year were performed. Two units performed >3 000 endoscopies per annum. All the units were involved in training for OGD and colonoscopy, with the two tertiary units offering additional training in ERCP.
Shortages and breakages
All the hospitals except the main teaching hospital experienced endoscopy breakages that disrupted services. There was an average of three upper endoscopic repairs of upper endoscopes per hospital per year (range 0 - 8), and 1.25 repairs of colonoscopes (range 0 -2). In the four units performing ERCP there were eight repairs to duodenoscopes, with one unit requiring four repairs. Two of these units stopped performing ERCP, one owing to lack of funding for ERCP accessories and another owing to prolonged disruption of fluoroscopy services. Fluoroscopy was available in only two units, but six others had fluoroscopy available in a theatre complex. Ten units had oesophageal dilators available; four units had both balloon dilators and Savary-Gilliard dilators and six had only Savary-Gilliard dilators. Three hundred and seventy oesophageal self-expandable metal stents were placed in four hospitals, with the two tertiary-level hospitals placing 295 of these. There were 409 biliary sphincterotomies performed, 327 (80.0%) of them in the two tertiary-level hospitals. Three hospitals lacked on-site endoscopic banding devices. One regional and one tertiary-level hospital had on-site access to H. pylori testing. One other hospital was equipped to perform endomucosal resection and submucosal dissection.
Open-ended questions
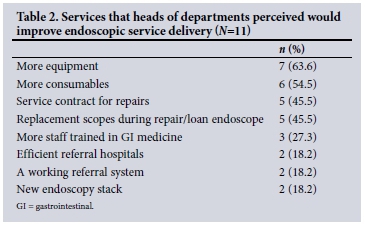
Respondents indicated that more equipment, availability of procedure accessories and trained endoscopy staff would improve service delivery. Furthermore, respondents felt that there was a need for service contracts to expedite the repair of broken equipment to avert disruptions in service delivery. Table 2 details the responses to the open-ended questions.
Discussion
This study investigated for the first time the current status of endoscopy services in KZN, SA. It demonstrated that endoscopy services lack facilities and trained specialist endoscopists and experience frequent breakages, which result in delays. Unlike the situation in HICs, general surgery consultants and surgery medical officers usually perform endoscopies.
The World Endoscopy Society has posted guidelines regarding the design and construction of endoscopy units and suggested minimum requirements. A minimum number of three rooms are recommended when >3 000 endoscopies are performed per year, with the third room catering for X-ray facilities.[4] Our study demonstrated the lack of infrastructure to deal with this workload based on the number of endoscopies performed in relation to available endoscopic suites (average 1.18), which is below the recommendation of three.[4] Having only a single room is problematic, as longer procedures requiring conscious sedation and endoscopy interventions such as ERCP and colonoscopy may overly occupy the often single endoscopy room available in a unit, limiting the number of routine endoscopies that can be performed on a normal working day. It is important to consider these factors when new hospitals or facility upgrades are planned.
An estimated 8.5 million people in KZN are burdened by diarrhoeal disease, HBV and H. pylori.[1] There are still major economic disparities between communities, reflected by the number of GEs in the system. There are 0.06 GEs per 100 000 population, which is well below the recommended minimum of 0.22/100 000. It is also lower than the national average of 0.12/100 000 cited previously,[12] and compares poorly with an expected 1.4 - 3/100 000 in HICs.[12] This trend has also been noted in other African countries.[6] It is concerning that GE training numbers are low, with only six GEs trained per year in SA, and unlikely to make an impact in the foreseeable future unless new impetus is found.
Performing >300 colonoscopies per year has been shown to improve adenoma detection rates dramatically.[15] It is therefore suggested that a full-time GE (performing at least 300 colonoscopies or 1 000 endoscopies a year) should perform the bulk of endoscopic procedures in an endoscopy unit. Although the number of endoscopists appears to be appropriate, the average number of 263 endoscopies performed per year is lower than the benchmark of 1 000.[4] Availability of general surgeons in endoscopy units is generally limited because of the competing interest of running an operating theatre, interfering with a dedicated endoscopy service. The lower average number of endoscopies performed may also reflect the frequent downtime of endoscopy services due to prolonged endoscopy repair periods. Most general surgery departments are responsible for training in OGD and colonoscopy, whereas internal medicine tends to focus on the non-interventional aspects of managing these diseases. The low number of GEs in training is a cause for concern and unlikely to change in the near future.
The average waiting times for endoscopy and colonoscopy were 27 and 29 days, respectively, including patients with alarm symptoms for malignancy. Waiting times were as long as 3 months in certain centres and exceeded the recommended TWR as used in the NHS.[14] Repair times for damaged equipment were frequently long, and are a major factor contributing to the delays and disruptions encountered by all endoscopic facilities in the province. These delays almost certainly contribute to both morbidity and mortality. The only facility that was not subject to these delays and disruptions had a service contract in place for replacement and maintenance of endoscopes. Fluoroscopy was not freely available, necessitating movement of unwieldy equipment from a GI unit to a radiology department and increasing the risk of mechanical breakage. A move towards dedicated mobile endoscopic units provides an alternative solution; this has been successfully employed in India, and less so in SA. It may provide an alternative means of reducing long waiting times.[4,16]
Recommendations
The study highlights the need to strengthen the endoscopic services by upgrading facilities and training GEs. The role of endoscopy is well established and is expanding as screening and endoscopic interventions become more common. The demand for endoscopic services will increase, requiring planning for adequate endoscopy facilities, staffing and equipment.
A number of strategies must be put in place if we hope to meet the demand for endoscopic services. An educational strategic plan to increase trainee numbers and service contracts is needed. Reducing the number of training years for GEs and staff retention strategies in the public sector may impact considerably on GE numbers in the underserviced component of the public sector.[10,17,18] Alternative training pathways have been proposed to increase the number of GEs trained by reducing the number of years required to produce a GE. A 2-year common internal medicine trunk followed by 2 - 3 years' training in gastroenterology can potentially fast-track GE training, but has not gained traction. It is unlikely that internal medicine will be able to provide sufficient manpower to meet this massive demand. Surgeons will continue to play a major role in delivering endoscopic services in SA for the foreseeable future.
The above educational approach is a long-term tactic that may only bear fruit over the next two decades. For this reason, a broader strategic approach should involve up-skilling of secondary hospitals by ensuring the employment of appropriately skilled doctors at these institutions, and improving equipment maintenance and availability. Focus should also be placed on ensuring that clinicians performing endoscopy undergo appropriate training.
Study limitations
A limitation of the study was that data retrieval, by and large, relied on manual extraction of facility data at most of the institutions. Electronic data systems improve data retrieval and analysis of bookings, delays and actual interventions performed. The need for the implementation of electronic data capturing in endoscopic units is well described. It ensures standardised reporting on procedures and allows retrieval of statistical data.[5]
This study was not intended to compare with existing models such as the Endoscopy Global Rating Scale (GRS), which focuses on both patient satisfaction and facility standards.[19] Our evaluation focused on whether minimum staff and facilities were available. However, the need for a GRS-based quality improvement programme with modifications applied to an LMIC is apparent. Another area we did not address was washing and disinfection facilities for endoscopes, which impact on cost, safety and staff.[4,20]
Conclusion
Endoscopy services in KZN are not adequately equipped and are plagued by frequent disruptions in services. Waiting times exceed the recommended TWR. There is a need to improve physical infrastructure and endoscopic equipment. Appropriate endoscopic training is important. It is also essential to ensure that those performing endoscopy do an appropriate number of endoscopies to maintain their expertise.
Acknowledgements. None.
Author contributions. EL: conceptual idea, study design, data collection, manuscript preparation; DLC: study design, data collection, manuscript preparation: KN: data interpretation; CJM: manuscript preparation.
Funding. None.
Conflicts of interest. None.
References
1. Mandeville KL, Krabshuis J, Ladep NG, Mulder CJ, Quigley EM, Khan SA. Gastroenterology in developing countries: Issues and advances. World J Gastroenterol 2009;15(23):2839-2854. https://doi.org/10.3748/wjg.15.2839 [ Links ]
2. Govender M, Aldous C, Ferndale L, Thomson SR, Clarke DL. Self-expanding metal stent placement for oesophageal cancer without fluoroscopy is safe and effective. S Afr Med J 2015;105(10):858-861. https://doi.org/10.7196/SAMJnew.8329 [ Links ]
3. Kew MC. Epidemiology of hepatocellular carcinoma in sub-Saharan Africa. Ann Hepatol 2013;12(2):173-182. [ Links ]
4. Mulder CJ, Jacobs MA, Leicester RJ, et al. Guidelines for designing a digestive disease endoscopy unit: Report of the World Endoscopy Organization. Dig Endosc 2013;25(4):365-375. https://doi.org/10.1111/den.12126 [ Links ]
5. Möschler O. Software tools in endoscopy - nice to have or essential? Visc Med 2016;32(1):37-41. https://doi.org/10.1159/000443628 [ Links ]
6. Perl D, Leddin D, Bizos D, et al. Endoscopic capacity in West Africa. Afr Health Sci 2016;16(1):329-338. https://doi.org/10.4314/ahs.v16i1.44 [ Links ]
7. Watermeyer G, van Wyk ME, Goldberg PA. Audit of provincial gastroenterology services in the Western Cape. S Afr J Surg 2008;46(3):68-72. [ Links ]
8. Ataguba JE, McIntyre D. Paying for and receiving benefits from health services in South Africa: Is the health system equitable? Health Policy Plan 2012;27(Suppl 1):i35-i45. https://doi.org/10.1093/heapol/czs005 [ Links ]
9. Thorne K, Hutchings HA, Elwyn G. Unmeasured improvement work: The lack of routinely collected, service-related data in NHS endoscopy units in England involved in 'modernisation. BMC Health Serv Res 2008;8(1):20. https://doi.org/10.1186/1472-6963-8-20 [ Links ]
10. Mulder CJ, Terhaar Sive Droste JS, Barrow PH. Endoscopic manpower in Romania seems deficient: Appropriate training is mandatory. Rom J Gastroenterol 2005;14(1):5-7. [ Links ]
11. Terhaar Sive Droste JS, Craanen ME, Kolkman JJ, Mulder CJ. Dutch endoscopic capacity in the era of colorectal cancer screening. Neth J Med 2006;64(10):371-373. [ Links ]
12. Mulder CJ Puri A, Reddy DN. Food for thought, a perspective of future GI training in SA: A review. S Afr Gastroenterol Rev 2009;7(2):6-9. [ Links ]
13. Telleman H, Burger TF, Mulder CJ. Evolution of gastroenterology training. World J Gastroenterol 2009;15(15):1793-1798. https://doi.org/10.3748/wjg.15.1793 [ Links ]
14. Galloway JM, Gibson J, Dalrymple J. Endoscopy in primary care - a survey of current practice. Br J Gen Pract 2002;52(480):536-538. [ Links ]
15. Wieten E, Spaander MC, Kuipers EJ. Accrediting for screening-related colonoscopy services: What is required of the endoscopist and of the endoscopy service? Best Pract Res Clin Gastroenterol 2016;30(3):487-495. https://doi.org/10.1016/j.bpg.2016.04.008 [ Links ]
16. Anderson DW, Goldberg PA, Algar U, Felix R, Ramesar RS. Mobile colonoscopic surveillance provides quality care for hereditary nonpolyposis colorectal carcinoma families in South Africa. Colorectal Dis 2007;9(6):509-514. https://doi.org/10.1111/j.1463-1318.2006.01172.x [ Links ]
17. Mills EJ, Kanters S, Hagopian A, et al. The financial cost of doctors emigrating from sub-Saharan Africa: Human capital analysis. BMJ 2011;343:d7031. https://doi.org/10.1136/bmj.d7031 [ Links ]
18. Ziady C, Bond R, Nwokolo C, Mulder CJ. Who will do an ERCP on me when I'm retired? S Afr Med J 2013;103(7):435. https://doi.org/10.7196/SAMJ.6928 [ Links ]
19. Stebbing JF. Quality assurance of endoscopy units. Best Pract Res Clin Gastroenterol 2011;25(3):361-370. https://doi.org/10.1016/j.bpg.2011.05.004 [ Links ]
20. Murdani A, Kumar A, Chiu HM, et al. WEO position statement on hygiene in digestive endoscopy: Focus on endoscopy units in Asia and the Middle East. Dig Endosc 2017;29(1):3-15. https://doi.org/10.1111/den.12745 [ Links ]
 Correspondence:
Correspondence:
E Loots
emilloots@hotmail.com
Accepted 30 May 2017














