Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.107 no.10 Pretoria Out. 2017
http://dx.doi.org/10.7196/samj.2017.v107i10.11371
RESEARCH
Male involvement in prevention of mother-to-child transmission of HIV in the context of partner testing in Goba town, Ethiopia: A facility-based cross-sectional study
M T AlemayehuI; J HaidarII
IBSc, MPH; Goba Hospital, Oromia Health Bureau, Goba, Ethiopia
IIMD, MSc, CRM, CME, HD; School of Public Health, Addis Ababa University, Ethiopia
ABSTRACT
BACKGROUND. Antenatal care (ANC) is an entry point for the prevention of mother-to-child transmission (PMTCT), particularly when a man accompanies his spouse for voluntary counselling and testing (VCT), even though this seldom happens in Ethiopia.
OBJECTIVE. To study the role of male partners in improving PMTCT/ANC, which is essential to prevent HIV/AIDS transmission in this country. Our study focused on identifying barriers for the low involvement in PMTCT/ANC among male partners whose spouses received ANC.
METHODS. A total of 422 male partners in Goba town, Oromia regional state, Ethiopia, were recruited in September - October 2014 and enrolled by a systematic sampling method. A facility-based cross-sectional study and two focus group discussions (FGDs) were conducted. Binary logistic regression and odds ratios were calculated to ascertain sociodemographic and other important information compared with the outcome variable and PMTCT/ANC, while the findings of the FGDs were grouped according to the emerging themes and analysed manually by means of a thematic approach.
RESULTS. The percentage of male partners (22.7%) accompanying their spouses for HIV testing and counselling at antenatal clinics improved three-fold when an invitation letter was introduced as a new initiative to increase male participation. Individuals in the age group 15 - 29 years (adjusted odds ratio (AOR) 5.4, 95% confidence interval (CI) 1.66 - 17.85), and whose duration of marriage was <5 years (AOR 5.6, 95% CI 1.83 -17.30), were more likely to be tested than their referent groups. Men without a higher education (AOR 0.1, 95% CI 0.02 - 0.50), who disagreed with legal enforcement (AOR 0.1, 95% CI 0.07 - 0.32), were less likely to be tested, while those who did not notify their partners (AOR 8.4, 95% CI 1.92 - 37.12) were more likely to use the service. Being busy, proxy testing, fears of testing HIV-positive, neglecting the importance of VCT, and inadequate knowledge about the PMTCT/ANC programme were other barriers that came to the fore in the FGDs.
CONCLUSION. Identified barriers have to be addressed, and helpful practices, such as using invitation letters to increase the uptake of the service by male partners, have to be instituted.
According to a Joint United Nations Programme on HIV/AIDS (UNAID) report,[1] it is estimated that by 2019, 33.3 million people worldwide will be living with HIV, of whom 2.5 million will be children. A total of 370 000 children are infected with HIV by means of mother-to-child transmission (MTCT). A total of 210 000 deaths related to AIDS were reported in 2009; most of these were in sub-Saharan countries, indicating that paediatric HIV infections are still prevalent in Africa.[1] Prevention of mother-to-child transmission (PMTCT) of HIV, particularly during antenatal care (ANC), is among the global strategies adopted to prevent paediatric HIV infection. In Ethiopia, PMTCT/ANC services have been implemented since 2001, but the programme faced some challenges, including low levels of utilisation, absence of compassionate respectful care and little involvement by men.[2]
The PMTCT/ANC programme is possibly an opportunity to improve the utilisation of the service, but demands the participation of male partners to comply with the programme.[3] Despite having been given the opportunity to participate, the compliance rate of male partners in most developing countries is low owing to socioeconomic, cultural and programmatic factors.[4] In Ethiopia, even though low male partner participation is mentioned as a major challenge to the success of this country's PMTCT/ANC programme, with new initiatives encouraging results are reported.[2] The success has been attributed to the various initiatives of the Ethiopian government at different levels, including a scale-up of the programme. These scale-up initiatives incorporated community mobilisation, awareness, creative efforts, demand creation and sending of an invitation letter to male partners to attend ANC.[5] Consequently, the number of health facilities providing a PMTCT service increased by 31% in 2010 - 2011 and the partner testing rate increased by 13% - from 7% in 2011 to 20% in 2012.[5] Similarly, a study done in Kayunga District, central Uganda, registered a 13% increase among male partners using the services, but more is required to increase male participation to contain the problem.[6] The extent of male involvement in some previous studies has not been examined in accordance with the existing voluntary counselling and testing (VCT) and provider initiative counselling and testing (PICT) endeavours. However, these might have underestimated the proportion of male PMTCT/ANC utilisation in addition to negligence and absence of legal backing regarding the use of available PMTCT/ANC services.[7] The objective of the current study was to examine the role of male partners and identify some of the barriers to improving the utilisation of PMTCT/ ANC in rural Ethiopia.
Methods
Study area and population
A cross-sectional study supplemented by two focus group discussions (FGDs) was conducted from 15 September to 9 October 2014 in the woreda (district) at Goba town among ANC attendants. This woreda is one of 18 in the Bale zone of the Oromia region, South-East Ethiopia, situated 444 km south-east of the capital, Addis Ababa. The woredas have 15 rural and 2 urban kebeles (villages). There is one government referral hospital and four health centres serving 89 859 people (projected from the Central Statistical Agency, 2011).[8] The hospital started providing a PMTCT service in 2002. ANC coverage for the woreda was 90% and the proportion of mothers counselled and tested in 2012 at Goba Hospital was 100%, whereas 10% of male partners were tested. The study site selected was convenient, as the hospital is one of the facilities in the Bale zone, which launched PMTCT services when Ethiopia adopted the programme; yet, the partner testing rate is below the expected national level. Therefore, the principal author, as a co-ordinator of the programme in the district, was interested in examining the factors contributing to the low male participation in the district despite the long-standing PMTCT/ANC service in the zone. In line with the new PMTCT/ANC scale-up initiatives, the zonal health office sends an invitation letter to all male partners to participate in the programme through the mother support programme or health development officials.
The participants recruited for the two FGDs were from mother support groups (MSGs) and female health extension workers (FHEWs) - all females aged between 25 and 40 years. In terms of their educational level, all FHEWs had studied further than grade 12, and four of them were married. Everyone in the MSGs was married and attended primary school only (discussed below under qualitative data collection section).
Sample size and sampling
The sample size was determined using single proportion formulas based on the estimation of the proportion of partner HIV testing at ANC in the study area, which was 10.0% for 2012 (Goba Hospital Health Management Information System prepared by the principal author and his team - unpublished data). An absolute precision of 3.0% and a 95% confidence interval (CI) with a non-response rate of 10.0% yielded a total of 422 subjects.
For the male participants, a sampling frame (SF) was constiuted and a man whose wife had attended ANC was registered (n=2 030). After obtaining the SF, it was divided by the sample size (n=422), which yielded a sampling interval of 5. Consequently, every fifth male participant with a random start from the prepared SF was selected until the required sample size was reached. The selected males were then traced by FHEWs, who have excellent knowledge of the programme, together with the field guides/community elders, to their place of residence. After a study participant's address was identified, an invitation letter was prepared by the zonal health office. FHEWs distributed the letter to the MSGs, to be handed to the participants by their wives. In this way, all male partners who volunteered were recruited and enrolled after written consent was obtained. The inclusion criteria were: male partner >18 years old, married, permanent resident, no major disability, and spouse visited the ANC clinic from July 2012 to June 2013. The entire private personal interview took place in the married couples' residence at their convenience.
Data collection instrument and procedure Quantitative data
Data were collected using a pre-tested, structured questionnaire adapted from previous similar studies conducted elsewhere.[8-10] The questionnaire consisted of components of sociodemographic information, knowledge about PMTCT, experience of counselling and testing for HIV at antenatal clinics, sociocultural beliefs about PMTCT/ANC, opinion about the need for confidentiality breaches between partners with regard to their HIV status, the need for legal enforcement of partners to use VCT services, and other sociocultural issues, e.g. do spouses consider pregnancy as belonging to the female domain only, and do they accompany their wives?
Five data collector FHEWs (selected from health posts to minimise bias, as FHEWs are not primary service providers), fluent in the local languages, and two supervisors (health officers) with relevant experience, were recruited and trained for 2 days regarding the method of data collection by the principal investigator. The training addressed issues such as the content of the questionnaire, basic interviewing skills, and filling out of the questionnaire. There were also five additional field guides/community elders who facilitated the tracing of male participants based on the information in the ANC registry.
Qualitative data
FGDs were used to supplement the quantitative study using an open-ended tool that included knowledge on the PMTCT programme, benefits of the programme, specific services rendered, importance of male partner HIV testing, perceived barriers to HIV testing at an ANC, opinion on partner notification, and legal enforcement of partner to use PMTCT/ANC. The FGDs included health workers (HWs) and MSGs. The first FGD was held among MSGs actively participating in similar programmes and recruited through the support of the FHEWs, while the HWs were recruited with the recommendation of the health office among those directly involved in the PMTCT/ANC programme of the hospital. Both FGDs were moderated by the principal investigator, assisted by someone who took notes, who was trained and who had relevant experience. The discussions were conducted in the local language, Amharic. The duration of the interviews was 45 - 90 minutes and the entire process was audio taped after participants granted permission.
Data quality management
The data quality was observed during questionnaire designing, which included widely used standard questions that had been pre-tested in PMTCT studies. The data collectors and supervisors were informed of the objective of the study, contents of the questionnaires and how to maintain confidentiality and privacy of the study subjects. The collected data were checked by the principal author on a daily basis for any incompleteness and/or consistency, and relevant action was taken immediately.
Statistical analysis
Data were checked for completeness, coded, entered using Epi-Info version 3.5.4 (Centers for Disease Control and Prevention, USA) and then exported to SPSS version 16 (SPSS Inc., USA) for analysis. Binary logistic regression and odds ratios (ORs) were calculated to ascertain the sociodemographic and other important information with the outcome variable, PMTCT/ANC. The findings of the FGDs were grouped according to the emerging themes and analysed manually. All sociodemographic characteristics and other covariates associated in a bivariate manner with p<0.20 were used and entered in the stepwise logistic regression calculations. In all analyses, p<0.05 was considered to be statistically significant.
In the qualitative data the entire audio-taped interview was transcribed and then translated into English. The content of the translated transcript of all the FGDs was read thoroughly and summarised under the themes. In this manner five major categories emerged.
Ethical considerations
Ethical approval was obtained from the School of Public Health Research Ethics Review Committee, College of Health Sciences, Addis Ababa University (ref. no. SPH/06). Permission was also secured from the woreda administration, woreda health office and Goba Hospital. Informed written consent was obtained from each subject for their participation, and the right to withdraw from the study at any time was also communicated to all of them. Anonymity and confidentiality of the information were assured and privacy of each respondent was maintained throughout the data collection process.
Definitions
Partner testing. This refers to women who are routinely offered HIV testing and counselling (HTC) and then encouraged to bring their partner for similar testing. In this study, partner testing with mutual disclosure is considered a form of couples' HIV testing and counselling (CHTC).[9]
Male involvement. This refers to engaging men to participate in health services together with their partners, or the male accompanying his spouse, especially in ANC settings for HTC.
Partner notification. This refers to an authorised individual in a health facility or health system sharing a person's HIV test result with that person's partner or partners to protect the health of that partner. This may occur with or without the expressed consent of the original partner.[9]
Opinion. This refers to a belief or judgment on a law that breaks confidentiality between a spouse and a law that enforces a partner to use the PMTCT service.
Composite level of PMTCT knowledge. This refers to the total number of correct answers to four questions on knowledge about MTCT of HIV, including questions on HIV transmission from an infected mother to her child during pregnancy, delivery and breastfeeding. Those who answered all four questions were considered to have adequate knowledge, while those answering between three and one as having inadequate knowledge.
Female health extension workers (FHEWs). This refers to female health workers in the health system, who are responsible for identifying pregnant women within their catchment area, delivering ANC, and connecting the women with the formal health system in the event of an increased risk or complications. FHEWs also have to follow up women during the postnatal period, when care is critical for both mother and newborn.
Mother support groups (MSGs). This refers to a peer support model that provides psychosocial support and adherence counselling, promotes facility delivery, encourages male involvement and family testing, provides group support, family planning and counselling, and promotes appropriate infant feeding options.
Health development army (HDA). This refers to volunteers who have been enlisted nationwide in the government's team, along with trained FHEWs, who are model families and foot soldiers in a massive social engineering project to redefine healthy behaviour.
Results
The quantitative data were collected from 409 respondents, with a 97.0% response rate, while the FGDs were conducted among eight MSGs and eight HWs.
Sociodemographic characteristics of respondents
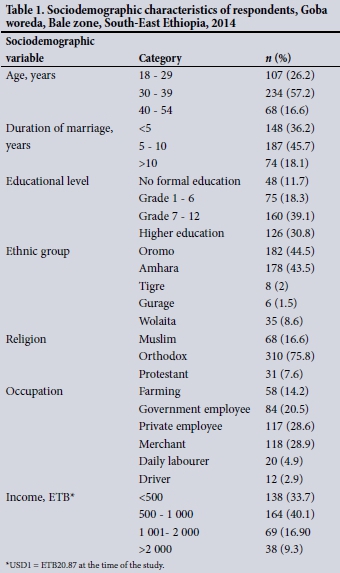
Over half (57.2 %) of the respondents were 30 - 39 years of age, most (63.8%) were married for >5 years, over two-thirds (69.9%) had secondary education and above, and the major ethnic groups were Oromos (44.5%) and Amharas (43.5%). Orthodox Christians constituted about three-quarters (75.8 %) of the respondents. Over half (57.5%) were either privately employed or were merchants, and about a third (33.7%) had a monthly income below USD24 (Table 1).
Knowledge and awareness about PMTCT
The proportion of male respondents who knew about MTCT during pregnancy, labour and delivery, and breastfeeding were 78.0%, 99.5% and 99.5%, respectively. Regarding awareness of the PMTCT/ANC programme, all respondents had heard about it and knew that the service existed in the hospital. Regarding HTC of women, nearly all knew that women were counselled and tested for HIV at PMTCT/ ANC clinics. The composite measure of respondents' knowledge, as determined by the total number of correct answers to four questions on knowledge of MTCT, indicated that over three-quarters (77.0%) had adequate knowledge (Table 2).
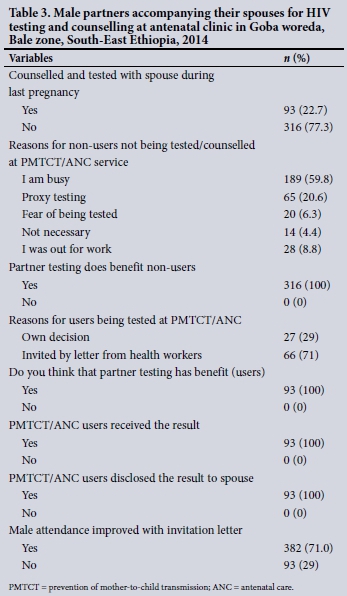
Male experience in PMTCT/ANC
The majority (77.3 %) were not counselled or tested for their HIV status with their pregnant wife during ANC. The major reasons for not using the services were: being busy (n=189 (59.8%)) and proxy testing (n=65 (20.6%)). Other reasons attributed were fear of being tested, negligence and abscence from work; these accounted for 6.3%, 4.4% and 8.8%, respectively.
Ninety-three respondents used the PMTCT/ANC service prior to the invitation letter. Nevertheless, after receiving the invitation letter from health workers through the MSGs, nearly three-quarters (10.0% v. 71.0%) of them complied. All 93 respondents who used the service believed that the PMTCT/ANC had benefits, underwent their HIV test on time, and shared (disclosed) their HIV results with their spouses. About three-quarters of the male participants (71.0%) complied and used the service after receiving invitation letters prepared by the zonal health office for their participation through the MSGs/HDA, emphasising the importance of letters for programme improvement (Table 3).
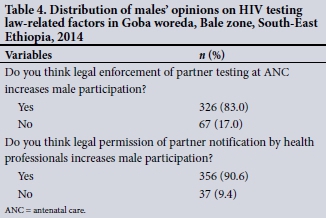
Opinion on HIV-testing laws
The majority (83%) of the respondents felt that endorsement (issuance) of a law that obliges male partners to participate (undergo HIV testing) in an PMTCT/ANC programme could increase their participation (Table 4). Likewise, the vast majority (90.6%) felt that legal permission of partner notification by health professionals increases male participation.
Factors associated with partner testing
Respondents who had been married for <5 years were significantly more likely to be tested than those who had been married for >10 years (crude odds ratio (COR) 3.3, 95% CI 1.46 - 3.90). Those partners who had adequate knowledge of the transmission of HIV/AIDS from mother to child during pregnancy, labour and delivery, and breastfeeding were more likely to be tested than those who had inadequate knowledge (COR 0.01, 95% CI 0.01 - 0.03). Similarly, partners who had no formal education and completed grade 7 - 12 were less likely to be tested than those who had completed higher education (COR 0.2, 95% CI 0.05 - 0.50; and COR 0.3, 95% CI 0.56 - 0.49), respectively. Partners who felt that legal enforcement is necessary to increase male participation in PMTCT/ANC were less likely to be tested than their counterparts (COR 0.3, 95% CI 0.17 - 0.51). Regarding endorsement of the law on partner notification by health professionals about the HIV status of individuals, those who responded affirmatively appeared more likely to be tested than their counterparts (COR 3.8, 95% CI 1.15 - 12.79, p=0.02).
Nevertheless, in the multiple logistic regression analyses, age, duration of marriage, educational status, legal enforcement and partner notification remained significant. Partners aged 18 - 29 years (adjusted odds ratio (AOR) 5.4, 95% CI 1.66 - 17.85) and married <5 years, were significantly more likely to be tested (AOR 5.6, 95% CI 1.83 - 17.30) than their counterparts. Those with no formal education were less likely to be tested than those who completed their higher education (AOR 0.1, 95% CI 0.02 - 0.05), and those whose partners studied up to grade 1 - 6 and 7 - 12 were also less likely to be tested than those who had completed higher education (AOR 0.3, 95% CI 0.10 - 0.99; AOR 0.09, 95% CI 0.032 - 0.24), respectively. Likewise, those who felt that legal enforcement is necessary were less likely to be tested than their counterparts (AOR 0.1, 95% CI 0.07 - 0.32). Nonetheless, partners who thought that partner notification by health professionals should be permitted were more likely to be tested than their counterparts (AOR 8.4, 95% CI 1.92 - 37.12) (Table 5).
According to the FGD participants, barriers that emerged during the discussions were aligned with the abovementioned findings and grouped into five major categories, summarised as follows:
- Lack of information/awareness by male partners of the PMTCT was mentioned by HWs and MSGs.
- Individual factors, such as fear of being tested, ignorance of the programme benefit, and work-related activities, were mentioned by both groups.
- Cultural factors, e.g. feeling that it is inappropriate for males to attend the programme because the issue is considered a woman's domain, were mentioned by both groups.
- The health system, e.g. inadequate resources, including room setup lacking privacy, as the room also delivers other maternal and child health services, was mentioned by HWs.
- Policy issues, e.g. lack of a mechanism to trace a male partner, neglecting MSG activities and problems related to working hours, were mentioned by both HWs and MSGs. Further, absence of an independent male ANC unit and male support groups, the need for partner notification (disclosure of one's HIV status to other partners), and legal enforcement of a male partner to use the VCT service, were among the barriers reflected in all the sessions by both HWs and MSGs. Other than these, it was underscored to maintain the new initiatives of writing invitation letters to male partners to participate in the programme to increase their participation and meet the desired programme objectives.
Discussion
The current study assessed the role of male PMTCT/ANC in the context of partner testing and associated factors in rural Ethiopia. In the study, 22.7% of male partners used the HTC service together with their spouses, with no-one influencing or inviting them to participate in the programme. This finding surpasses the national partner testing rate of 20.0% reported in 2012,[5] as well as some small-scale studies, which reported 17% and 15.7% in 2011.[10,11] Similarly, the current figure from Ethiopia is nearly four-fold that in a Ugandan study, which reported that only 5.0% of men had accompanied their spouses to the PMTCT/ANC.[12] It is also interesting to note that after the invitation letter for males to participate in the programme was distributed though the MSGs, male participation increased three-fold. This suggests that the implementation of an invitation letter is a viable approach to attract male partners to use the service and contributes to the success of the programme.
In this study, it was found that a number of factors could be associated with male participation in the PMTCT/ANC programme. These include age of male, duration of marriage and educational status. For instance, men aged 15 - 29 years were more likely to get tested than those 40 - 54 years of age. This suggests that the programme should focus on the latter age group for the betterment of the programme in Ethiopia. Contrary to our finding, the Zambian study documented that an increase in age has a positive influence on men's willingness to be involved in PMTCT[13] This assertion, however, needs careful interpretation and might require a further large-scale study.
Regarding the duration of marriage, those who were married for <5 years were more likely to be tested than those who were married for >10 years. This is concordant with the Zambian finding, which documented that a longer relationship between men and women may have a negative influence on the men's involvement in PMTCT/ ANC.[12] With regard to educational status, a male with no formal education was less likely to be tested than one who had completed a higher education. This finding is also consistent with that of the study conducted in Uganda, which stated that men with secondary education were more likely to be tested than those who had primary or no formal education.[11]
Although the majority of males in our study were not counselled or tested for HIV together with their wife at ANC during her last pregnancy, the figure is lower than that previously reported for Gojam (77.3% v. 84.7%), Ethiopia (10%) and Cameroon (77.3% v. 82.0%%).[14]
The low utilisation of PMTCT/ANC in this study was attributed to work load/being busy, which correlates with the findings of a Tanzanian study.[15] Another reason attributed to men not being tested was proxy testing (i.e. assuming to have the same HIV status as that of one's partner); the finding is congruent with that of the study done by Maryce[16] in Ethiopia. Other barriers identified were fear of being tested, negligence even though aware of the benefits of the service, and being away from work. Similar barriers and misconceptions have also been reported elsewhere in Africa,[16,17] underscoring the need for more focused behavioural change and counselling intervention.
One of the notable, interesting findings in our study is the three-fold improvement in the utilisation of the service as a result of the invitation letter that was sent to the males/partners, which increased the success of the programme. Similarly, the systematic review done on challenges and successes of males participating in PMTCT/ANC services in sub-Saharan Africa also showed an increase of 30% when a letter of invitation was sent to male partners,[4] substantiating further that sending such a letter could augment the utilisation of the service by male partners.
Regarding husband/wife communication, the vast majority of males reported that their wife had shared (disclosed) their HIV test results with them during their last pregnancy. The wife did not need the husband's permission to use the PMTCT/ANC or HIV testing service. In contrast to the current finding, the Zambian study underlined the need for a husband's permission for an HIV test,[12] probably because of cultural differences, and requires some remedial action.
Regarding the perception of the service among PMTCT/ANC users, almost all of them stated that the work ethic of the HWs was good, and that they treated the clients professionally and within a reasonable time. This shows some degree of client satisfaction with the service rendered. A similar client satisfaction level with the actual service provided was documented in Uganda.[18]
Nonetheless, the absence of an independent male ANC unit and of a male support group, the need for partner notification (disclosure of one's HIV status to others without permission) and legal enforcement of a male partner to use a VCT service were among other barriers reported by all participants, also during the FGDs and elsewhere.[12,18,19] Such reports need to be carefully interpreted in line with the standard ethical guideline, avoiding human rights violations. However, sometimes, from the child-rights point of view, an appropriate counselling service is necessary.
Although participants of both quantitative and qualitative groups supported an obligatory law to improve male partner participation, its practicality would be difficult because it appears to violate the principle of medical ethics. It is also apparent that some participants did not support the idea, suggesting the use of measures such as convincing males to participate in the programme through an invitation letter, which turned out to be effective, as evidenced in this study.
In terms of legal permission of partner notification by health professionals, there were different opinions, as most participants were in favour of the idea, while a few others were against it. The latter stated that it could lead to family separation, gender-based violence and stigmatisation, ultimately affecting service utilisation - based on FGDs. This, however, requires a further large exploratory study as the current study was limited to the zone.
Study limitations
Data collection was carried out by FHEWs, which might have maximised social desirability bias. In addition, measuring the temporal relationship was not easy, as both exposure and outcome variables were collected simultaneously. The study was limited to health facilities.
Conclusion
The majority of male partners did not accompany their spouses to the PMTCT/ANC clinic, implying that the level of partner testing is below the expectation of the perceived plan. Therefore, it is more important to strengthen and continue the previous activities, e.g. by using a letter of invitation and MSGs, while addressing the barriers impeding the programme, which were identifed in the quantitative and FGD findings.
Besides, a strategy must be designed that helps partner tracing. Intensified co-ordinated and targeted information, education and communication materials/programmes need to be developed to convince male partners to utilise the service. A strategy should also be developed for community mobilisation and supporting of the programme. Likewise, couple counselling must be promoted and awareness raised through behavioural change and communication among the community. A new approach should be developed for promoting male participation in the programme, e.g. introducing male support groups, creating male ANC clinics, offering couples counselling during weekends at ANC clinics, using peer educators for mobilising male participation and improving the structure of the healthcare system. Furthermore, it is necessary to encourage and incentivise men to use the PMTCT/ANC services to ensure an HIV-free generation.
Acknowledgements. This study was funded by the School of Public Health, Addis Ababa University. We express our gratitude to Goba Hospital staff, FHEWs who served as data collectors, and the male participants.
Author contributions. MT and JH conceptualised the study, wrote the manuscript, and approved the final version.
Funding. The study was supported by the College of Health Sciences, School of Public Health, Addis Ababa University.
Conflicts of interest. None.
References
1. Joint United Nations Programme on HIV/AIDS. Global AIDS Epidemic. UNAIDS Report on the Global AIDS Epidemic. Geneva: UNAIDS, 2013. [ Links ]
2. Federal Ministry of Health. Complementary Continuous Quality Improvement Guidance Note. National Accelerated Scale Up Plan for PMTCT Service 2012. Addis Ababa: FMoH, 2012. [ Links ]
3. United Nations Children's Fund. Programme Recommendations for the Prevention of Mother-to-child Transmission of HIV: A Practical Guide for Managers. New York: UNICEF, 2010. [ Links ]
4. Kalembo FW, Zgambo M, Mulaga AN, Yukai D, Ahmed NI. Male partner involvement in prevention of mother-to-child transmission of HIV in sub-Saharan Africa: Successes, challenges and way forward. Open J Prevent Med 2012;2(1):35-42. [ Links ]
5. Federal Ministry of Health. National Comprehensive PMTCT/MNCH Training Package Referral Manual 2012. Addis Ababa: FMoH, 2012. [ Links ]
6. Mary D. Male involvement in the prevention of mother-to-child transmission of HIV (PMTCT) programme in Kayunga District. 2010. https://www.musphcdc.ac.ug/files/pdf/Mary_Dutki.pdf (accessed 29 August 2017). [ Links ]
7. Federal Ministry of Health. Guideline for HIV Counselling and Testing in Ethiopia, 2007. Addis Ababa: FMoH, 2012. [ Links ]
8. Central Statistical Authority. Ethiopia Demographic and Health Survey, 2014. Addis Ababa, Ethiopia: CSA, 2014. [ Links ]
9. World Health Organization. Guidance on Couple HIV Testing and Counseling, including Antiretroviral Therapy for Treatment and Prevention in Serodiscordant Couples. Geneva: WHO, 2012. [ Links ]
10. Gebremedhin D, Gemechis H, Sibhatu B, Gebre M, Misrak M. PMTC programme using CQI approach in Southwest Shoa Zone, Oromia Region, Ethiopia. Addis Ababa: AIDSTAR, 2011. [ Links ]
11. Addisu B, Abebe G. Factors affecting acceptance of HIV counseling and testing among antenatal care attendants, with emphasis on role of male partner. Int J Sci Eng Res 2012;3(4):45-49. [ Links ]
12. Robert B, Jemes K, Nulu S, Thorkild T. Determinants of male involvement in the prevention of mother-to-child transmission of HIV programme in Eastern Uganda: A cross-sectional survey. Reprod Health 2010;7:12. https://doi.org/10.1186/1742-4755-7-12 [ Links ]
13. Tshibumbu DD. Factors influencing men's involvement in PMTCT programmes. MPH thesis. Pretoria: University of South Africa, 2006:6-7. https://www.k4health.org/sites/default/files/male_involvement_pmtct.pdf (accessed 29 August 2017). [ Links ]
14. Nkuoh GN, Meyer DJ, Nshom EM. Women's attitudes toward their partners' involvement in antenatal care and prevention of mother-to-child transmission of HIV in Cameroon, Africa. J Midwif Women's Health 2013;58(1):83-91. https://doi.org/10.1111/j.1542-2011.2012.00208 [ Links ]
15. Yohana B. Willingness and participation toward prevention of mother to child transmission among males of reproductive age. A study from Kilimanjaro, Tanzania. Tanzania Medical Students' Association 2008/2009:1-4. [ Links ]
16. Maryce R Ethiopia gender assessment. Intra Health 2012:39-52. www.intrahealth.org (accessed 29 August 2017). [ Links ]
17. Morfaw F, Mbuagbaw L, Thabane L, et al. Male involvement in prevention programmes of mother- to-child transmission of HIV: A systematic review to identify barriers and facilitators. Syst Rev 2013;2:5. https://doi.org/10.1186/2046-4053-2-5 [ Links ]
18. Drasiku A. Acceptability and satisfaction of male partners with antenatal clinic based HIV testing for PMTCT at Mulago Hospital, Uganda. MSc thesis. Kampala, Uganda: Makerere University, 2010:1-15. https://news.mak.ac.ug/2011/06/mak-theses (accessed 29 August 2017). [ Links ]
19. Kayembe KN. Role of men in programme to prevent mother-to-child transmission of HIV in Jwaneng, Botswana. MPH thesis. Johannesburg: University of the Witwatersrand, 2005. [ Links ]
 Correspondence:
Correspondence:
J Haidar
hjemal@gmail.com
Accepted 11 May 2017














