Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.107 n.10 Pretoria Oct. 2017
http://dx.doi.org/10.7196/samj.2017.v107i10.12392
IN PRACTICE
HEALTHCARE DELIVERY
Evaluating 5 years' NIMART mentoring in South Africa's HIV treatment programme: Successes, challenges and future needs
M JonesI; D CameronII
IRN, MSc; East Sussex Healthcare NHS Trust, UK; and Evaluation Unit, Foundation for Professional Development, Pretoria, South Africa
IIMB ChB, M Prax Med, MPhil, FCFP (SA); Department of Family Medicine, School of Medicine, Faculty of Health Sciences, University of Pretoria, South Africa; and Evaluation Unit, Foundation for Professional Development, Pretoria, South Africa
ABSTRACT
Task shifting has enabled South Africa (SA) to rapidly expand its HIV treatment programme. This has been achieved by training and mentoring primary-care nurses in nurse initiation and management of antiretroviral therapy (NIMART). Five years into its clinical mentoring programme, the Foundation for Professional Development conducted an evaluation that identified improved knowledge, attitudes and confidence perceived by nurses who received NIMART mentoring. Low completion rates for the Department of Health (DoH) NIMART training process were identified and therefore targeted mentoring was introduced; this increased the percentage of primary nurses eligible for DoH certificates of clinical competence in NIMART from 12%, adding a further 30%. There remain a large number of primary nurses who require mentoring in order to complete the NIMART process. For those who have completed the process, there remains a need for ongoing mentoring as SA's HIV programme evolves, complex cases emerge and primary care undergoes change.
The Foundation for Professional Development (FPD) has contributed to the rapid expansion of South Africa (SA)'s HIV treatment programme. We wanted to evaluate FPD's clinical mentoring programme, in order to identify its achievements and shortcomings, with a view to planning for the future.
Over the past 10 years, research has shown that shifting the initiation and management of antiretroviral therapy (ART) from specialised, hospital-based clinics to primary-care nurses is complex and challenging.[1-6] Such task shifting has been shown to improve access to and early initiation of ART, reduce mortality and improve retention in care,[7] and has resulted in a reduced burden on referral hospitals.[8] Further benefits that have been demonstrated include reduced patient waiting times, less costly healthcare provision[9,10] and improved health-related quality of life in patients living with HIV.[11] The clinical mentorship of primary-care nurses by mentors with experience and expertise in HIV management has been shown to increase confidence and enhance professional development, and should be considered essential to ensure universal ART access in resource-limited settings.[12,13]
We undertook a multifaceted review of the clinical mentoring of professional nurses initiating and maintaining HIV-positive patients on ART in primary-care clinics in 4 districts of SA, over a period of 5 years. These districts cover an area of 62.7 km2 (5% of SA's landmass), and contain a population of 6.5 million people (12% of its total population).
We reviewed the mentoring process that is set out in the Department of Health (DoH)'s Clinical Mentoring Manual for Integrated Services ('the manual'),[14] and assessed the effectiveness of clinical mentoring by roving teams of mentors in equipping nurses with the knowledge, attitudes and skills required for nurse initiation and management of ART (NIMART).
Training and competency of the clinical mentors
To equip its professional staff to mentor NIMART-trained nurses, FPD orientated its doctors to become clinical mentors and to provide 6 months' clinical-skills training and work-based supervision to its professional nurses, who had been working in ART clinics for several years. All these nurses had attended a 5-day NIMART training course as a prerequisite to becoming a clinical mentor. During the 6 months of supervision, the nurses attended 36 days of training in: HIV counselling and testing, prevention of mother-to-child transmission (PMTCT), adherence counselling, diagnosis and management of tuberculosis (TB), management of sexually transmitted infections, isoniazid prophylactic therapy, integrated management of childhood illnesses, Practical Approach to Lung Health and HIV/AIDS in SA (PALSA PLUS), paediatric HIV management, maintaining ART registers and SA's electronic medical record system (TIER.net).
The mentoring process
These nurses kept a logbook of 80 patients who they had managed, as set out in the manual. The competence of these nurses as clinical mentors was tested in a series of three 12-station objective structured clinical examinations, moderated by experienced external examiners. Between 2010 and 2012, 39 professional nurses were assessed as competent, and deployed to provide clinical mentoring to professional nurses working in primary-care clinics supported by FPD. From 2012, the doctors, nurses and data management mentors - a health information system mentor and a data capturer - were grouped into roving mentor teams of four, who travelled together and visited clinics according to a set schedule. Specialist mentors in maternal and infant care, TB and community liaison provided additional support in accordance with the districts' priorities.
The teams each travel in a double-cab pick-up truck, from a convenient central starting point, and visit between one and four clinics a day. The total average daily distance covered is 94 km per team. The shortest distance may be only 3 km, while the farthest clinics in the rural districts of Nkangala and Vhembe are respectively 125 and 190 km from the central starting point. As a result, a significant period of time is spent travelling. Some clinics are visited weekly, while the more distant clinics only receive a monthly visit.
The DoH requires all professional nurses working in primary care to undertake NIMART training. Clinical mentoring was introduced to ensure the continuing professional development of nurses following the theoretical part of NIMART training, and to support progress towards the 54 clinical competencies that are set out in the manual. The mentor encourages the mentee to follow the relevant DoH clinical guidelines, and if necessary, to phone for advice between visits. The mentee records in a logbook brief details of all the cases seen, and these are reviewed by the mentor at the next visit. Each NIMART nurse is required to see a minimum of 80 patients of various age groups (including infants), both men and women (including women who are pregnant) and those co-infected with HIV and TB. When the logbook is complete and the mentor satisfied with the clinical competence of the mentee, a portfolio of evidence (POE) is submitted to the DoH Regional Training Centre. The DoH then acknowledges the competency of the NIMART nurse by issuing a certificate of clinical competence.
The evaluation
The aim of our evaluation was to describe and analyse the achievements and evolution of clinical mentoring for NIMART-trained professional nurses by roving mentor teams in primary-healthcare facilities in the health districts of Tshwane (Gauteng Province), Nkangala (Mpumalanga Province), and Capricorn and Vhembe (Limpopo Province) over a period of 5 years. These are the four health districts that were supported by FPD at the time of the evaluation.
In order to evaluate the roving mentorship programme, the following questions were considered:
- What are the strengths and weaknesses of the mentoring process set out in the manual?
- How many nurses completed the mentorship process and received certificates of clinical competence from the DoH, and how long did this take?
- What was the coverage of mentorship provided by the roving mentor teams?
- Is the model of roving mentor teams cost-effective and sustainable?
- How should the process of clinical mentoring adapt as the HIV epidemic evolves and changes in donor funding occur?
Semi-structured interviews were conducted with a convenience sample of NIMART nurses, facility managers, roving mentors and their operational managers. Data were also obtained from routine monitoring and evaluation reports, and from the DoH District Health Information System. Signed consent was obtained from all participants; interviewee responses and comments were recorded anonymously. The data analysis included statistical calculation and thematic analysis of the qualitative data.
Ethical approval was obtained from the Research Ethics Committee of FPD on 10 December 2013 (ref. no. 2013/12/10).
During the first quarter of 2014, a clinical nurse specialist from the UK with 25 years' experience in HIV care, including 3 months establishing NIMART mentoring in the Eastern Cape Province,[15] visited 66 primary-care facilities in the four districts. He accompanied the roving mentor teams on their routine visits, and interviewed 92 professional nurses who had completed classroom training in NIMART, 20 facility managers, 4 subdistrict programme managers, 45 roving mentors and 12 FPD operational managers.
Results
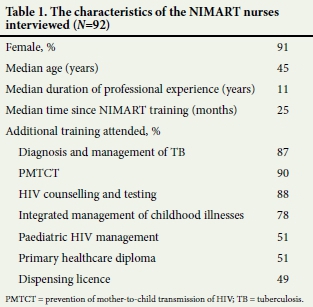
The NIMART-trained nurses who were interviewed were experienced professional nurses, many of whom had attended a number of related courses (Table 1).
Strengths and weaknesses of the mentoring process
Eighty-seven percent of the NIMART nurses interviewed said that mentoring had met their expectations, and 78% felt that the frequency of mentoring visits had been 'just right'. Factors leading to this positive response included maintaining scheduled visits, the easy availability of the mentor for telephonic advice and the mentors' supportive attitude, which made the nurses feel that they were not being 'policed':
The mentor corrects us very nicely.' (Nurse)
Effective mentoring requires a commitment to a long-term relationship of support and guidance, and nurses appreciated this:
'One of the reasons it has worked is that it is the same team over a long period of time that can start to build real relationships.' (Nurse)
There was a great deal of initial apprehension on the part of professional nurses that the down referral of patients from centralised ART clinics would overwhelm them. However, despite the increased workload, 94% agreed that mentoring had helped to bring about a positive change in their attitude towards taking on the responsibility for initiating and managing patients on ART:
'I feared down referral but now it's an easy job to me; ART works.' (Nurse)
'There has been no increase in staffing in facilities, but HIV has increased the number of attendances, and on top of this the community's awareness of health issues has improved.' (Nurse)
As a result of personal experience of HIV, some nurses were highly motivated to treat HIV-positive patients:
'Many relatives and friends have died. I am trying to help those that are left.' (Nurse)
Despite their NIMART training, prior to mentoring, some nurses were anxious about providing HIV care:
'I previously feared even touching patients with HIV until the mentor explained things, motivated listening skills and empathy.' (Nurse)
While some knowledge is gained during classroom instruction, most learning occurs in the workplace. It is during this initial phase of translating theory into practice, and using the guidelines in practice, that mentoring plays such a vital role:
'I did not feel clear after the NIMART course, but my mentor used the guidelines to help me to choose regimens, refer appropriately and deal with side effects.' (Nurse)
Completion of the mentoring process
Nurses exhibited high levels of knowledge, confidence and competence in NIMART, but reported limited motivation to provide written evidence: by March 2014, only 13% (12) had completed the POE, and 8% (7) had received the certificate of clinical competency:
'The requirement for 80 cases is too many - it is discouraging. Get rid of the annual presentation of certificates of clinical competency - it causes delay'. (Nurse)
While the manual provided a valuable template to guide mentoring, many factors interfered with the completion of the process and the issuing of certificates of clinical competence. The following reasons were given by the NIMART nurses for not completing the process:
- Not seeing enough HIV-positive children - this was seen as resulting from the success of the PMTCT programme.
- Not being involved in the management of complex cases such as pregnant women co-infected with HIV and TB.
- Being unaware that there was a logbook, or too busy to maintain or complete it.
Mentors were praised for their accessibility, and their support in managing complex cases such as advanced HIV disease, treatment failure, initiation of ART in children and interpreting abnormal biochemistry results. However, the mentoring process was undermined by high patient numbers, reported absenteeism of part-time clinic doctors, nurse rotation to other aspects of primary-care provision, inadequate consultation space and the non-availability of essential medicines.
Coverage and sustainability
FPD's 32 roving teams mentored 2 010 (60%) of 3 359 professional nurses in 409 health facilities in the 5 years reviewed. During this time, the 32 teams travelled a total of 3 700 560 km, at a cost of R6 216 941 (R1.68/km). The salaries for the 32 teams amounted to R267 200 million (R1.67 million/team/year). The total cost of this work-based mentoring programme was R268 million. The average cost per nurse mentored was R133 391 (Table 2).

Evolution
The evaluation found that 94% of nurses felt confident in initiating ART, and many had a growing sense of independence from their mentor. They felt that their skills in listening to their patients, performing physical examinations, making comprehensive assessments, interpreting laboratory results, providing adherence counselling and solving clinical problems had improved significantly:
'Nurses are more knowledgeable and I get fewer phone calls.' (Mentor)
'We have a weekly meeting to discuss cases and ring FPD if we cannot resolve challenges together.' (Nurse)
While the initial phase of gaining confidence and competence in ART initiation is easily achieved, the skills required to recognise and manage the complications that may occur in patients taking ART take time to develop:
'I think now we are moving away from [ART] initiation because most of the nurses are comfortable with that. We have stepped into reviewing side-effects and everything they are picking up. But we are getting patients that are having resistance and treatment failures so we need to build their confidence there.' (Mentor)
It was encouraging to see the professional maturity and competence that continues to grow in the NIMART nurses. Being a competent primary-care clinician requires life-long learning. The following comment is thus realistic and understandable:
' Don't stop coming - we need 2 years' mentoring in order to be stable, independent.' (Nurse)
The temptation to 'cut corners' can be a danger with a complex process such as NIMART. However,
'Mentoring visits prevent the clinic from complacency.' (Nurse)
' Having outside scrutiny helps to maintain sound minds on HIV.' (Nurse)
There is a need for a balance between encouraging independent practice and maintaining mentoring, as HIV care and patient needs evolve:
' HIV is always changing so mentoring will always be needed.' (Nurse)
'Without the roving team we would be experiencing big problems.' (Nurse)
Professional isolation in a community primary clinic is a reality. The objectivity of a mentor provides encouragement and invaluable support. With ART guidelines subject to frequent revision, mentoring provides necessary updating of these.
Discussion
Our evaluation considered the evolution of a large PEPFAR (the US President's Emergency Plan for AIDS Relief)-funded clinical mentoring programme supporting primary-care nurses to deliver the NIMART programme over a 5-year period. We demonstrated the effectiveness of mentoring NIMART-trained professional nurses using teams of roving mentors, which has improved their knowledge, attitudes and skills. This was true in both urban and remote rural primary clinics. Mentoring also encouraged nurses to complete the POE: prior to this evaluation, 241 (12%) of 2 010 professional nurses in the four health districts had completed the POE. When mentors focused on encouraging its completion, a further 600 (30%) completed the DoH process.
Participants agreed that NIMART mentoring has enabled nurses to successfully take on the role of initiating and maintaining HIVpositive patients in primary-care clinics. The DoH process of submitting POEs and being awarded certificates of competence was found to be dysfunctional, although rates of completion were improved through intensive, focused mentoring. Both processes require the investment of significant resources and amounts of time. In order to sustain the NIMART programme, professional nurses identified the need for ongoing mentoring to maintain standards of care and for support when managing complex cases. Multidisciplinary team case discussions were cited as a useful approach.
Conclusion
The key findings of the evaluation are summarised as follows:
- Clinical mentoring by roving mentor teams has enabled primary-care nurses to become competent in initiating and maintaining ART.
- While clinical mentoring is costly, it has improved access to ART.
- Nurses delivering the NIMART programme require ongoing mentoring in order to increase the numbers who have completed the DoH mentoring process, and to deal with complex HIV-related problems.
- With the integration of clinical services at primary-care clinics, work-based mentoring will need to be broadened to include the full spectrum of programmes delivered in primary care.
Recommendations
HIV is an evolving epidemic; as guidelines and patient needs change, clinical mentoring will similarly need to adapt in a climate where cost is an unavoidable consideration. Participants suggested a number of ways that mentoring could adapt, including: fewer and less-frequent mentoring visits, more telephonic mentoring and multidisciplinary complex-case discussions.
Mentoring should focus on the DoH process in order to achieve higher rates of POE submission and increase the number of certificates of competence awarded.
With the integration of clinical services at primary care clinics, work-based mentoring will need to be broadened to include the full spectrum of programmes delivered in primary care.
Acknowledgements. None.
Author contributions. MJ: design, data gathering, analysis, writing; DC: design, analysis, writing.
Funding. Foundation for Professional Development.
Conflicts of interest. None.
References
1. Chan AK, Ford D, Namata H, et al. The Lablite project: A cross-sectional mapping survey of decentralized HIV service provision in Malawi, Uganda and Zimbabwe. BMC Health Serv Res 2014;14:352. https://doi.org/10.1186/1472-6963-14-352 [ Links ]
2. Uebel K, Guise A, Georgeu D, Colvin C, Lewin S. Integrating HIV care into nurse-led primary health care services in South Africa: A synthesis of three linked qualitative studies. BMC Health Serv Res 2013;13:171. https://doi.org/10.1186/1472-6963-13-171 [ Links ]
3. Emdin CA, Millson P. A systematic review evaluating the impact of task shifting on access to antiretroviral therapy in sub-Saharan Africa. Afr Health Sci 2012;12(3):318-324. https://doi.org.org/10.4314/ahs.v12i3.11 [ Links ]
4. Fairall L, Bachmann MO, Lombard C, et al. Task shifting of antiretroviral treatment from doctors to primary-care nurses in South Africa (STRETCH): A pragmatic, parallel, cluster-randomised trial. Lancet 2012;380(9845):889-898. https://doi.org/0.1016/S0140-6736(12)60730-2 [ Links ]
5. Davies NE, Homfray M, Venables EC. Nurse and manager perceptions of nurse initiated and managed antiretroviral therapy (NIMART) implementation in South Africa: A qualitative study. BMJ Open 2013;3(11):e003840. https://doi.org/10.1136/bmjopen-2013-003840 [ Links ]
6. Grimsrud A, Kaplan R, Bekker LG, Myer L. Outcomes of a nurse-managed service for stable HIV-positive patients in a large South African public sector antiretroviral therapy programme. Trop Med Int Health 2014;19(9):1029-1039. https://doi.org/10.1111/tmi.12346 [ Links ]
7. Fox MP, Rosen S. Patient retention in antiretroviral therapy programs up to three years on treatment in sub-Saharan Africa, 2007 - 2009: Systematic review. Trop Med Int Health. 2010; 15(s1): 1-15. https://doi.org/10.1111/j.1365-3156.2010.02508.x [ Links ]
8. Nyazulu JC, Muchiri E, Mazwi SL, Ratshefola M. NIMART rollout to primary healthcare facilities increases access to antiretrovirals in Johannesburg: An interrupted time series analysis. S Afr Med J 2012; 103(4): 232-236. https://doi.org/10.7196/samj.6380 [ Links ]
9. Boullé C, Kouanfack C, Laborde-Balen G, et al. Task shifting HIV care in rural district hospitals in Cameroon: Evidence of comparable antiretroviral treatment-related outcomes between nurses and physicians in the Stratall ANRS/ESTHER trial. J Acquir Immune Defic Syndr 2013;62(5):569-576. https://doi.org/10.1097/QAI.0b013e318285f7b6 [ Links ]
10. Long L, Brennan A, Fox MP, et al. Treatment outcomes and cost-effectiveness of shifting management of stable ART patients to nurses in South Africa: An observational cohort. PLoS Med 2011;8(7):e1001055. https://doi.org/10.1371/journal.pmed.1001055 [ Links ]
11. Suzan-Monti M, Blanche J, Boyer S, et al. Benefits of task-shifting HIV care to nurses in terms of health-related quality of life in patients initiating antiretroviral therapy in rural district hospitals in Cameroon [Stratall Agence Nationale de Recherche sur le SIDA (ANRS) 12110/Ensemble pour une Solidarité Thérapeutique Hospitalière en Réseau (ESTHER) substudy]. HIV Med 2015;16(5):307-318. https://doi.org/10.1111/hiv.12213 [ Links ]
12. Green A, de Azevedo V, Patten G, Davies MA, Ibeto M, Cox V. Clinical mentorship of nurse initiated antiretroviral therapy in Khayelitsha, South Africa: A quality of care assessment. PLoS One 2014;9(6):e98389. https://doi.org/10.1371/journal.pone.0098389 [ Links ]
13. Cameron D, Gerber A, Mbatha M, Mutyabule J, Swart H. Nurse initiation and maintenance of patients on antiretroviral therapy: Are nurses in primary care clinics initiating ART after attending NIMART training? S Afr Med J 2012;102:98-100. https://doi.org/10.7196/samj.5195 [ Links ]
14. National Department of Health, South Africa. Clinical Mentorship Guide for Integrated Services. Pretoria: DoH, 2011. [ Links ]
15. Jones M, Stander M, van Zyl M, Cameron DA. The recall of lost to follow-up pre-antiretroviral therapy patients in the Eastern Cape and the impact of mentoring on patient care. S Afr Med J 2012; 102(9):768-769. https://doi.org/10.7196/samj.5957 [ Links ]
16. Swart AM, Chisholm BS, Cohen K, Workman LJ, Cameron D, Blockman M. Analysis of queries from nurses to the South African National HIV & TB Health Care Worker Hotline. S Afr J HIV Med 2013;14(4):179-182. https://doi.org/10.7196/sajhivmed.948 [ Links ]
 Correspondence:
Correspondence:
M Jones
martinjones6@nhs.net
Accepted 17 July 2017














