Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.107 no.8 Pretoria Ago. 2017
http://dx.doi.org/10.7196/samj.2017.v107i8.12352
IN PRACTICE
CASE REPORT
Ocular metastasis as initial presentation in breast cancer
M MaliepaardI; M MeshamII; Z AleksicIII; R ScholtzIV; J EdgeV
IMB BS; Department of Surgery, Charlotte Maxeke Johannesburg Academic Hospital, Johannesburg, South Africa
IIMB ChB, FCS (SA); Department of Ophthalmology, Life Peninsula Eye Hospital, Cape Town, South Africa
IIIMD, FCS (SA); Department of Ophthalmology, Cape Town Mediclinic, Cape Town, South Africa
IVMB ChB, DCH, FCS (SA); Department of Ophthalmology, Life Eye and Laser Centre, Life Peninsula Eye Hospital, Cape Town, South Africa
VMMed (Surg); Netcare Christiaan Barnard Memorial Hospital, Cape Town, South Africa
ABSTRACT
Two patients presented to their ophthalmologists with vision disturbances. On ocular examination, retinopathic lesions were observed. On subsequent examination, these lesions were diagnosed as metastases of breast cancer. Neither patient had a history of breast cancer. In patients with breast cancer and multiple metastases, ocular metastases are well described. However, the latter is uncommon as a presenting complaint.
Metastatic disease involving the eye is rare. In women, the primary cancer most commonly occurs in the breast. Ocular metastases from breast cancer are generally a feature of widespread disseminated disease. It is rare for ophthalmological symptoms to be the presenting symptoms of a breast primary carcinoma. We present two patients who were not known to have breast cancer and who were diagnosed with ocular metastases, which were subsequently shown to be from a breast primary lesion.
Case 1
A 74-year-old woman presented to her ophthalmologist with a 4-week history of deteriorating vision in her right eye. She noticed flashing lights for the first 2 weeks, followed by 2 weeks of decreased visual acuity.
On examination, the visual acuity on the right was 0.4 best corrected (left: 1.0) and the anterior segment was normal.
The dilated pupil fundus examination revealed exudative retinal detachment (retinal detachment with no visible retinal tears, holes or breaks) with subretinal haemorrhage and a choroidal mass ~2 disc diameters superior from her optic disc (Fig. 1).

The mass was provisionally diagnosed as a choroidal secondary lesion, as it did not appear to be a choroidal melanoma. The patient initially reported to be well, but on further questioning with regard to comorbidities she mentioned noticing a breast lump.
On examination of her breasts, she had locally advanced breast cancer of the left breast with overlying skin nodules and ipsilateral lymphadenopathy. Core biopsy showed the lesion to be grade 3 ductal carcinoma - oestrogen receptor (ER)-positive, progesterone receptor (PR)-positive, HER2-negative. A computed tomography (CT) scan showed an intraocular lesion with widespread pulmonary and bony metastases. She was treated with endocrine therapy.
Case 2
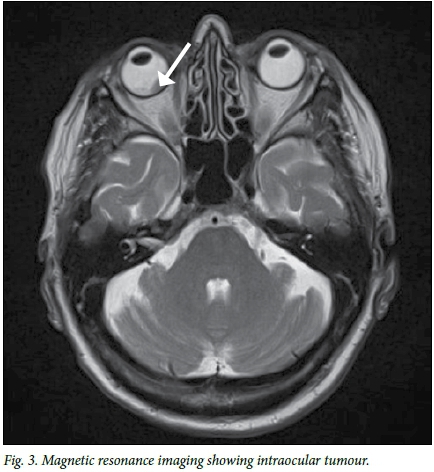
An 80-year-old woman presented to her ophthalmologist with a 1-month history of blurred vision in her right eye. The vision was reduced to 6/18 and she had a large pale subretinal lesion nasal to the disc. She was otherwise well. An ultrasound scan of the eye showed a single, 14 mm choroidal mass (Fig. 2). Magnetic resonance imaging (MRI) confirmed an intraocular mass (Fig. 3), in keeping with a metastatic lesion. She was unaware of any other problems. On examination, her breasts were normal. Her mammogram showed a 6 mm lesion in the left breast. Biopsy revealed a grade 1 ER-positive, PR-positive, HER2-negative ductal carcinoma. A CT scan showed multiple pulmonary metastases and an adrenal mass. These were interpreted in keeping with metastatic breast cancer rather than melanoma. She was treated with an aromatase inhibitor and her vision has improved.

Background
The presenting symptoms of ocular tumours are blurred vision, loss of peripheral vision or floaters.
The differential diagnosis includes:
• choroidal melanoma
• choroidal metastases (commonly breast and lung)
• choroidal haemorrhage
• inflammatory lesions of the choroid (granulomatous diseases)
• retinoblastoma (in children).
Orbital tumours tend to present differently. The common presenting symptoms are proptosis, pain, diplopia and blurred vision. The differential diagnosis includes:
• orbital pseudotumour
• thyroid eye disease
• haemangioma
• meningioma
• lymphoma
• rhabdomyosarcoma
• metastases.
Discussion
The eye is an uncommon site for metastatic lesions, as it does not have a well-developed lymphatic system. Therefore, metastatic spread to the eye is haematogenous. The uveal tract, which is the most vascular part of the eye, is the most likely to be affected.[1]
Ninety percent of metastatic lesions deposit in the choroid, causing painless loss of vision. The most common presentations are blurred vision, visual field defects and floaters.[2-4] In ~10% of cases the iris and ciliary body are involved.[1,3] In such cases, patients present with chronic anterior uveitis or raised intraocular pressure owing to iris neovascularisation or trabecular meshwork block from metastatic deposits.[1] The inflammation and raised pressure are resistant to treatment. Less commonly, breast adenocarcinoma will deposit in the orbital lymphatic tissue behind the eye and present with exophthalmos and pain.[2,4]
On examination, choroidal metastases appear as pale subretinal lesions. The lesions exude serous fluid into the subretinal space and frequently cause retinal detachment. Choroidal metastases are associated with a disproportionately large amount of subretinal fluid compared with primary choroidal melanomas.[1,3,5] Both of our patients had retinal detachment at presentation, which is not uncommon in women with metastatic breast cancer. In contrast, with melanomas, the deposit is usually of a significant size before an exudative retinal detachment can be seen.
Many choroidal metastases are asymptomatic, unless the macula is directly involved by tumour or the associated retinal detachment. They tend to be pale and often have a characteristic leopard-spot appearance from retinal pigment epithelial change on the surface. Lipofuscin from poorly functioning retinal pigment epithelium can be observed on the surface of metastatic deposits, which can also be seen in choroidal melanoma.[1] Fluorescein angiography of a meta-static deposit reveals hypofluoresence in the arterial phase followed by late hyperfluorescence, with no pooling of dye. Indocyanine green angiography of the deeper choroidal vasculature is useful to differentiate choroidal haemangioma from a metastatic deposit. However, the most helpful investigation is an ocular ultrasound scan. Metastases are typically placoid shaped with an undulating surface and show medium to high blood flow velocity.
Most ocular metastases are indistinguishable in terms of the original primary tumour; however, certain primary tumours are associated with a particular metastatic appearance. Carcinoid metastases in the choroid appear orange, as do thyroid metastases. Renal metastases are more likely to produce intraocular haemorrhage. A solitary ocular metastasis from a cutaneous melanoma is pigmented and difficult to distinguish from a primary choroidal melanoma, although retinal and vitreous pigmented seeding is an indication that the pigmented choroidal tumour may be a secondary lesion.
When investigating ocular tumours, a breast examination and chest radiograph should be performed to determine the possible presence of a primary lesion. A liver ultrasound scan and liver function tests should be done to investigate the presence of potential liver metastases. An MRI of the brain is an important investigation, as cerebral and intraocular cancers often coexist. If the primary source of the metastatic lesion is unknown, a positron emission tomography (PET) scan or CT scan should be considered. These are very helpful investigations for lymphoma and melanoma, which are metabolically active and therefore show good uptake of fludeoxyglucose F18 (FDG).[1]
The proportion of ocular tumours caused by metastases depends on when the tumours are diagnosed. A survey of 716 patients with ocular disease leading to their death showed that 9.3% had metastatic disease to the eye. However, this is more commonly seen at postmortem examination than in routine practice.[1] Common primary sites include breast (47%) and lung (21%). Other primary sites are prostate, gastrointestinal tract, kidney and skin (melanoma).[6] The metastases usually present as unilateral disease.[2] However, bilateral disease does occur, with an incidence of 20%.[7]
In women with widespread metastatic breast cancer, 28 - 58% may have orbital metastases[1,6] that may be asymptomatic. The metastases generally present 4.5 - 6.5 years after the initial diagnosis.[7]
However, ocular metastasis is seldom the initial presentation of a previously undetected cancer.
Conclusion
Although ocular metastases as primary presentation of breast cancer are rare, it is an important diagnosis to consider. When examining a patient with ophthalmological complaints suggesting an infiltrative process, a thorough history must be taken and, in women, a full clinical examination must include a breast examination.
Acknowledgements. We would like to thank both of the patients for sharing their history with us.
Author contributions. All authors contributed to the article.
Funding. None.
Conflicts of interest. None.
References
1. Cohen VML. Ocular metastases. Eye 2013;27(2):137-141. https://doi.org/10.1038/eye.2012.252 [ Links ]
2. Vlachostergios PJ, Voutsadakis IA, Papandreou CN. Orbital metastasis of breast carcinoma. Breast Cancer 2009;3:91-97. [ Links ]
3. Wickremasinghe S, Dansingani KK, Tranos P, Liyanage S, Jones A, Davey C. Ocular presentations of breast cancer. Acta Ophthalmologica 2007;85(2):133-142. https://doi.org/10.1111/j.1600-0420.2006.00737.x [ Links ]
4. Ahmada MS, Esmaeli B. Metastatic tumors of the orbit and ocular adnexa. Curr Opin Ophthalmol 2007;18(5):405-413. https://doi.org/10.1097/ICU.0b013e3282c5077c [ Links ]
5. Georgalas I, Paraskevopoulos T, Koutsandrea C, et al. Ophthalmic metastasis of breast cancer and ocular side effects from breast cancer treatment and management: Mini review. BioMed Res Int 2015. https://doi.org/10.1155/2015/574086 [ Links ]
6. Arepalli S, Kaliki S, Shields CL. Choroidal metastases: Origin, features, and therapy. Ind J Ophthalmol 2015;63(2):122-127. https://doi.org/10.4103/0301-4738.154380 [ Links ]
7. Francone E, Murelli F, Paroldi A, Margarino C, Friedman D. Orbital swelling as a first symptom in breast carcinoma diagnosis: A case report. J Med Case Rep 2010;4:211. https://doi.org/10.1186/1752-1947-4-211 [ Links ]
 Correspondence:
Correspondence:
J Edge
dr@jennyedge.co.za
Accepted 29 March 2017














