Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.107 no.8 Pretoria Ago. 2017
http://dx.doi.org/10.7196/samj.2017.v107i8.12710
CME
Heat-related illness in the African wilderness
R HofmeyrI; C D'AltonII
IMB ChB, DipPEC, DA, MMed (Anaes), FCA (SA), FAWM; Department of Anaesthesia and Perioperative Medicine, Faculty of Health Sciences, University of Cape Town; and WildMedix, Cape Town, South Africa
IIMB ChB, MSc (Sport Exercise Med); Sports and Exercise Medicine, Faculty of Human Biology, University of Cape Town, South Africa
ABSTRACT
Wilderness heat-related illnesses span a variety of conditions caused by excessive or prolonged heat exposure, and/or the inability to compensate adequately for increased endogenous production during strenuous outdoor activities. Despite management of well-known risk factors, such as lack of fitness or acclimatisation, dehydration, underlying illness and certain medications, even highly trained individuals may exceed their physiological capability to dissipate increased core temperature. Heat illnesses range from benign cramps to the more concerning heat syncope and exercise-associated collapse (with or without hyperthermia), and culminate in life-threatening heat stroke. The differential diagnosis in the wilderness is broad and should include exercise-associated hyponatraemia with or without encephalopathy. Clinical guidelines for wilderness and hospital management of these conditions are available. Field management and evacuation are based on severity, and include cooling, rehydration and assessment of core temperature and serum sodium, if possible. Hyponatraemia should be corrected with the use of oral or intravenous hypertonic saline, depending on whether the patient can safely take oral fluids. Hospital management may include aggressive and potentially invasive cooling, careful assessment for organ dysfunction, and intensive multi-organ support, if required. Paracetamol, non-steroidal anti-inflammatory drugs and dantrolene should not be used.
Scenario
A fit-looking 23-year-old male participant in a summer mountain trail run collapses 3 km from the end of the 25 km race. Despite the altitude, ambient temperatures are warm, and the participants have been exposed to the full sun for several hours. On your first assessment, he is very confused, with a weak, rapid pulse (160 beats per minute). His skin is wet and cool. A passing member of the same running club alleges that he is not known to have any medical conditions. You notice that his water bottles are both empty. As fellow runners help you carry him to the nearby medical-aid station, a rapidly expanding differential diagnosis fills your thoughts.
Background
Wilderness heat-related illnesses span a continuum of medical problems caused by the generation of, and/or exposure to, excessive heat in the wilderness environment. They can range from minor annoyances to life-threatening conditions. Endogenous heat production is directly dependent on the sum of that from inescapable sources, such as basal cellular metabolism and cardiorespiratory work, and heat generated by physical exertion. All heat exchange (gain or loss) occurs through four mechanisms: conduction, convection, radiation and evaporation. Conduction refers to the direct transfer of heat from one object to another through contact. Convection is heat gain or loss due to movement of a fluid (such as air); a convection oven or wind chill from an Antarctic breeze are similar examples. Radiation describes transfer of heat through electromagnetic waves, epitomised by the heat of the sun on skin. Evaporation is the loss of heat induced by the phase change from liquid to gas, which is dramatically affected by ambient vapour pressure or relative humidity.
Many animals have developed ingenious strategies to adapt their physiology to control heat gain or loss. Indeed, it is hypothesised that particular human traits - our upright stance, complex bony structure of the foot, nuchal ligament, relatively hairless skin and copious capacity for perspiration - evolved to give us an advantage in chasing down prey in the prehistorical African heat.[1] Today, however, humans are unique in their ability to adapt the environment to control their physiology through behaviour and material means: use of clothing, shelter, and devices such as heaters and air conditioners. Despite this, we cannot alter the laws of thermodynamics, and people in the wilderness are subject to the same exposure and thermal exchange mechanisms as our primitive ancestors. Fortunately, the development of modern science, clothing technology, and an understanding of physiology allow us to function successfully in environments of extreme heat under many adverse circumstances (Fig. 1).
Risk factors traditionally considered to increase our susceptibility to the deleterious effects of heat stress include obesity, lack of acclimatisation to hot environments, poor physical fitness, extremes of age, underlying illness (e.g. cardiac conditions, hyperthyroidism), dehydration, certain medications (e.g. beta blockers, anticholinergics, and diuretics) and illicit drugs (e.g. amphetamines, cocaine, and Ecstasy).
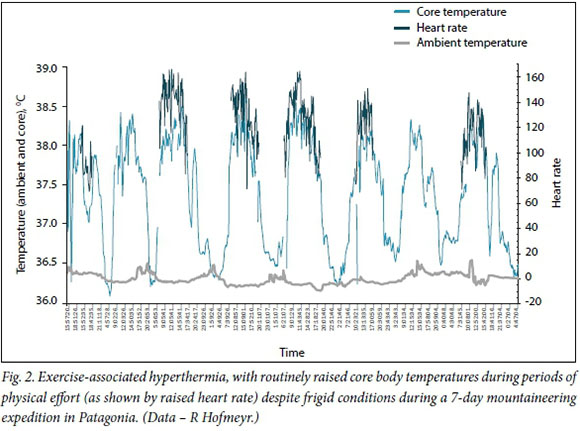
Heat-related illnesses are usually preventable. Mitigating factors include improved physical fitness, heat acclimatisation, selection of appropriate clothing, maintaining adequate hydration, sufficient rest periods, and enhancing evaporative cooling. These may be recalled using the CHAFER mnemonic (Table 1). However, it is important to appreciate that exertional heatstroke and other forms of heat illness can occur in spite of the optimal control of these factors.[2] Similarly, it is normal for well-adapted individuals to experience an increase in core temperature above 'normal' values during exercise, even in the setting of low environmental temperatures (Fig. 2). Therefore, core temperature alone is not a reliable indicator of heat illness or injury in the absence of other signs, and illness only occurs when physiological compensation to balance heat gain/production with heat loss fails.
Definition and spectrum of heat-related illnesses
Heat-related illnesses are not neatly delineated conditions, but rather occur as a spectrum - from benign to catastrophic. To better understand the pathophysiology of heat illness, it is essential to clarify the definitions thought to encompass these entities.
Classifying the manifestations into discrete categories, however, is useful to ascribe the correct urgency of management and level of severity.
Heat cramps
Heat cramps are muscle spasms that typically occur in the large muscle groups of the leg, and may be debilitatingly severe. The precise aetiology is still being debated, but is thought to be a combination of calcium and other electrolyte derangements at tissue level, plasma volume depletion, tissue acidosis in the light of respiratory alkalosis from hyperventilation, and altered neuro-muscular control related to exertion.[3-5] As these cramps can occur without exposure to a warm environment and typically resolve rapidly, they are often considered not to be true heat illness.
Heat rash and sunburn
Prickly heat or miliaria rubra is infrequently seen in the South African (SA) context, but occurs in humid or tropical climates owing to exocrine sweat duct blockage during copious or prolonged sweating. It presents as an erythematous pruritic rash with papules, usually on the neck, trunk and limbs, but sparing hands and feet. While heat rash alone is more of an irritation than a serious illness, the reduction in sweat production by duct obstruction can greatly reduce efficiency of evaporative heat loss and predispose the sufferer to more severe injuries. Sunburn - epidermal and dermal damage due to exposure to ultraviolet radiation - also limits sweat production. In its severe form, it can result in a systemic inflammatory response manifesting with headache, nausea, fever or rigors, and delirium.
Heat syncope and exercise-associated collapse
This condition is traditionally defined as a transient collapse or brief loss of consciousness occurring immediately after strenuous exercise in a warm environment. The patient usually rapidly regains clear consciousness shortly after becoming supine, or with raising of the legs. It is often seen in athletes, where it is possibly a manifestation of exercise-associated syncope. It commonly occurs immediately after completion of intense exercise. There are sudden decreases in venous return when skeletal muscle contraction is halted and blood pools in the lower extremities, in the context of exercise-induced peripheral vasodilation and decreased systemic vascular resistance. This may be compounded by an abnormal baroreflex response, Bezold-Jarisch or Barcroft-Edholm reflex. As this condition can occur during intense exercise in the absence of hot conditions, it is frequently termed exercise-induced postural hypotension.
Heat exhaustion
While heat exhaustion is understood to be a manifestation of intra-vascular volume depletion and dehydration caused by prolonged effort in a thermally stressful environment, many in the sports medicine community believe that heat exhaustion is a more severe form of exercise-associated collapse or exercise-induced postural hypotension, and not a separate entity. In the wilderness environment, it is typified by symptoms of fatigue, effort intolerance, weakness, headache, nausea, tachycardia and sometimes dyspnoea. The patient may have a warm or cool skin, with profuse sweating. Core temperature is either normal or mildly elevated (<39°C). Critically, there is no persistent change in mental state. If altered mentation remains for more than a few minutes after the patient is supine, with legs raised, it should be treated as heat stroke.
Exercise-associated hyperthermia
Raised core body temperature (<40°C) that results from strenuous exertion or exercise may be a normal consequence of increased endogenous heat production, and can occur in cold environments, particularly in athletes exercising at or close to maximum capacity (Fig. 1). Where exercise-associated hypothermia leads to collapse or altered level of consciousness, it indicates the development of heat exhaustion or heat stroke. In athletes, this typically occurs over medium distances (5 - 21 km). Previous occurrence is a risk factor.
Heat stroke
Heat stroke is a true medical emergency. The defining characteristics are a core temperature of >40°C and encephalopathy, manifested by altered mental status. While often distinguished as occurring as a result of prolonged exposure to high ambient temperatures (classic heat stroke) or pathological hyperthermia during exercise (exertional heat stroke), it is most commonly a combination of the two in the context of wilderness medicine. The patient may be sweating, but often has a dry skin. Clinical signs include confusion, disorientation, decreased level of consciousness, inappropriate behaviour, ataxia or collapse, tachypnoea, and tachycardia, or the patient may be in cardiovascular shock on presentation. Dysrhythmias can occur. Risk of brain, renal, hepatic and other organ damage depends on duration of hyperthermia, with systemic protein denaturation beginning at >42°C. The patient may develop a systemic inflammatory response syndrome (SIRS) owing to cytokine and heat-shock protein release, which mimics sepsis.[6] Hypoperfusion of the gastrointestinal tract is exacerbated by inflammatory-mediated increase in mucosal and vascular permeability, leading to endotoxin migration from the gut to the circulation.[7] This is thought to lead to the multi-organ failure that causes death in severe or untreated cases.[8]
Exercise-associated hyponatraemia
While not specifically a heat-related illness, exercise-associated hyponatraemia (EAH) often occurs in the setting of prolonged effort in hot conditions. It is therefore important to understand the condition, and to consider it as a differential diagnosis. Defined as a serum sodium concentration <135 mmol/L within 24 hours of prolonged physical activity, it is believed to be caused by an interplay between excessive fluid intake (especially hypotonic fluids such as clear water) and reduced water excretion under the influence of antidiuretic hormone due to the physical stress imposed by exercise.[9] Of these factors, overhydration (>1 500 mL/h) is considered the most prominent cause. While most cases are asymptomatic and go undetected, EAH can cause fatigue, nausea/vomiting, headache, dizziness, blurred vision and tachycardia. Severe cases can result in cerebral oedema (even non-cardiogenic pulmonary oedema) and confusion, decreased level of consciousness, and seizures. In these cases, it is termed exercise-associated hyponatraemic encephalopathy (EAHE).
Exercise-associated hyponatraemic encephalopathy
As described above, EAHE is defined as the presence of altered mental status, seizures or coma in the presence of EAH. As a biochemically proved reduction in serum sodium is required to confirm the diagnosis, it should be considered in all patients presenting with appropriate risk factors (prolonged effort, particularly in a warm environment, combined with significant hypotonic fluid intake and oliguria).
Wilderness medicine guidelines for heat-related illnesses
The Wilderness Medical Society (WMS) has published practice guidelines for wilderness emergency care, heat-related illnesses, and EAH, most recently updated in 2014.[2,9,10] These peer-reviewed, expert-consensus guidelines form an excellent foundation upon which local recommendations can be made for the African context, drawing from local experts in fields such as wilderness, emergency and sports medicine.
Clinical diagnosis and temperature measurement
The practitioner is usually alerted to the initial presence of heat-related illness by patient symptoms. In the wilderness, a presumptive diagnosis is made on the clinical signs described above, in the presence of heat exposure and/or excessive endogenous production. However, as hyperthermia and heat stroke can exist in the absence of excessive ambient temperatures - even in patients with cool extremities and skin - contemporaneous measurement of core body temperature is very valuable in excluding or confirming the diagnosis, assessing severity, and monitoring response to treatment. Unfortunately, accurate core temperature measurement in the field is challenging. Invasive gold-standard measurements (pulmonary artery catheter or oesophageal thermistor) are infrequently available, and skin, oral or infrared tympanic measurements lack accuracy.[11] A pragmatic approach is to treat lucid patients according to their perceived temperature (as they do not have heat stroke if fully conscious and orientated), use a rectal thermometer for patients with altered consciousness, and insert an oesophageal thermistor, when available, in unconscious patients who have an advanced airway in place.[12]
Field management
Severity of outcome of heat-related illness is directly proportionally related to duration of exposure. Treatment should therefore be initiated in the field, both to limit the progression of severity and to limit duration. Fortunately, there are many interventions that can be commenced in resource-constrained settings that will improve patient outcome (Table 2).
Field testing of serum sodium is available using compact, battery-powered point-of-care devices, such as the i-STAT analyser (Abbott Point of Care, USA).[13] However, in very hot environments, these devices often have a limited operation temperature range (e.g. 16 -30°C for the i-STAT[14]), and the device may have to be kept cool in the field to guarantee function when required.[15]
Hospital management
Cases of suspected heat-related illness should always be managed urgently on admission to hospital. In addition to swift primary assessment and any related advanced life-support interventions, a reliable (rectal or oesophageal) core temperature and serum sodium measurement should be obtained as a matter of priority. Intravenous access should be established. It is valuable to obtain haematological, electrolyte, creatinine kinase, renal and liver function tests at the same time. Patients with altered mental status and a core temperature of >39°C must be urgently cooled, using methods described below. Invasive cooling using bladder, gastric, pleural or peritoneal lavage can be considered if the patient does not respond rapidly. Seizures should be controlled with a benzodiazepine or propofol, which may necessitate intubation and ventilation. Treat hypotension or shock with fluid resuscitation, but avoid hypotonic fluids, especially if the serum sodium level is unknown. If EAHE is diagnosed, up to three 100 mL boluses of 3% hypertonic saline at 10-minute intervals are advocated. There is no risk of central pontine myelinolysis with this therapy in the context of EAHE.[9]
Serum potassium and calcium should be assessed and corrected if abnormal. If there is biochemical evidence of rhabdomyolysis, promoting positive fluid balance, diuresis with furosemide, and alka-linisation of urine with sodium bicarbonate can be considered.[7,8] In contrast to fever, there is no role for paracetamol and non-steroidal anti-inflammatory drug use in heat stroke, which may cause further harm.[10] Dantrolene has also not been shown to contribute to man-agement.[16] Admission to an intensive care unit (ICU) with renal dialysis and management for multi-organ failure may be required. The treating clinicians should be alert for acute respiratory distress syndrome, liver or kidney injury, coagulopathy and gastrointestinal ischaemia.
Scenario resolution
You consider the potentially differential diagnosis, including presentation of underlying febrile illnesses such as malaria, hypoglycaemia, drug toxicity or intoxication, cardiac ischaemic events, epilepsy, an occult head injury or EAH. However, the hot conditions and strenuous exertion make heat exhaustion or heat stroke very likely.
At the medical station, you elevate the athlete's legs, rapidly commence cooling by soaking his clothing in cool water and encouraging evaporation by fanning, and obtain a rectal temperature of 41.2°C. Recognising the medical emergency, you establish IV access, and recognising the risk of hyponatraemia, start isotonic fluid resuscitation. You request an urgent evacuation, even though the patient is gradually becoming more lucid. On arrival at the emergency unit, he is found to have significant rhabdomyolysis and dehydration in addition to heat stroke, but despite spending a night in the ICU, he avoids more serious consequences because of your swift interventions.
References
1. Bramble DM, Lieberman DE. Endurance running and the evolution ofHomo. Nature 2004;432(7015):345-352. https://doi.org/10.1038/nature03052 [ Links ]
2. Wilderness Medical Society Expert Panel. Heat-related illnesses. In: Forgey WW, ed. Wilderness Medical Society Practice Guidelines for Wilderness Emergency Care. Connecticut, USA: FalconGuides, 2006:62-63. [ Links ]
3. Schwellnus MP. Cause of exercise associated muscle cramps (EAMC) - altered neuromuscular control, dehydration or electrolyte depletion? Br J Sports Med 2009;43(6):401-408. https://doi.org/10.1136/bjsm.2008.050401 [ Links ]
4. Schwellnus MP, Derman EW, Noakes TD. Aetiology of skeletal muscle 'cramps' during exercise: A novel hypothesis. J Sports Sci 1997;15(3):277-285. https://doi.org/10.1080/026404197367281 [ Links ]
5. Schwellnus MP, Drew N, Collins M. Muscle cramping in athletes - risk factors, clinical assessment, and management. Clin Sports Med 2008;27(1):183-194, ix-x. https://doi.org/10.1016/j.csm.2007.09.006 [ Links ]
6. Dallimore J, Dhillon S, Winser S. Hot, dry environments: Deserts. In: Johnson C, ed. Oxford Handbook of Expedition and Wilderness Medicine. Oxford: Oxford University Press, 2015:745-767. [ Links ]
7. Bouchama A, Knochel JP. Heat stroke. N Engl J Med 2002;346(25):1978-1988. https://doi.org/10.1056/NEJMra011089 [ Links ]
8. Leon LR, Bouchama A. Heat stroke. Compr Physiol 2015;5(2):611-647. https://doi.org/10.1002/cphy.c140017 [ Links ]
9. Bennett BL, Hew-Butler T, Hoffman MD, et al Wilderness Medical Society practice guidelines for treatment of exercise-associated hyponatremia: 2014 update. Wilderness Environ Med 2014;25(4 Suppl):S30-S42.https://doi.org/10.1016/j.wem.2014.08.009 [ Links ]
10. Lipman GS, Eifling KP, Ellis MA, et al Wilderness Medical Society practice guidelines for the prevention and treatment of heat-related illness: 2014 update. Wilderness Environ Med 2014;25(4 Suppl):S55-S65. https://doi.org/10.1016/j.wem.2014.07.017 [ Links ]
11. Strapazzon G, Procter E, Paal P, et al. Pre-hospital core temperature measurement in accidental and therapeutic hypothermia. High Alt Med Biol 2014;15(2):104-111. https://doi.org/10.1089/ham.2014.1008 [ Links ]
12. Hofmeyr R. Wilderness cold-exposure injuries: An African perspective. S Afr Med J 2017;107(7):566-570. https://doi.org/10.7196/SAMJ.2017.v107i7.12610 [ Links ]
13. Backer HD, Collins S. Use of a handheld, battery-operated chemistry analyzer for evaluation of heat- related symptoms in the backcountry of Grand Canyon National Park: A brief report. Ann Emerg Med. 1999;33(4):418-422. [ Links ]
14. Herr DM, Newton NC, Santrach PJ, et al Airborne and rescue point-of-care testing. Am J Clin Pathol 1995;104(4 Suppl 1):S54-S58. [ Links ]
15. Joslin J, Mularella J, Schreffler S, et al. Novel method for reducing temperature of i-STAT1 analyzer in extreme environments. Wilderness Environ Med 2014;25(3):357-358. https://doi.org/10.1016/j.wem.2014.01.002 [ Links ]
16. Bouchama A, Cafege A, Devol EB, et al Ineffectiveness of dantrolene sodium in the treatment of heatstroke. Crit Care Med 1991;19(2):176-180. https://doi.org/10.1097/00003246-199102000-00011 [ Links ]
 Correspondence:
Correspondence:
R Hofmeyr
ross.hofmeyr@uct.ac.za














