Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.107 n.7 Pretoria Jul. 2017
http://dx.doi.org/10.7196/samj.2017.v107i7.12355
RESEARCH
Interprofessional communication in organ transplantation in Gauteng Province, South Africa
H R EtheredgeI; C PennII; J WatermeyerII
IPhD. Wits Donald Gordon Medical Centre, Johannesburg, South Africa
IIPhD. Health Communication Research Unit, School of Human and Community Development, Faculty of Humanities, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
BACKGROUND. Communication is essential to the transplant process, but it is challenging in South Africa (SA) because of the complexity of the country and the health system, the nature of transplantation as a technical procedure with inherent psychological considerations, and the large number of professionals involved. Transplant communication has not been explored in SA, and this study was the first to use health communication methods to generate empirical evidence relating to it.
OBJECTIVE. To explore communication in transplant settings in Gauteng Province, SA.
METHODS. Qualitative methods were used to collect data across six hospitals and transplant centres in Gauteng. State and private institutions were equally represented. Health professionals and transplant co-ordinators participated. Thematic analysis of data was undertaken.
RESULTS. Facilitators of interprofessional transplant communication included appreciation of its importance to good practice and cohesive individual transplant teams. Barriers to interprofessional communication were observed when individual teams had to come together in a multi-team, interdisciplinary environment, when interchange became aggressive, and when information was not passed on to other health professionals timeously. These barriers had implications for continuity of care and ethics, which could lead to moral distress.
CONCLUSION. Transplantation in Gauteng is characterised by aspects of good teamwork, and the importance of effective communication is acknowledged. Transplantation also faces some challenges in terms of interprofessional communication. Recommendations for mitigating some of the gaps include integrating a health communication specialist into the transplant process, 'knotworking', the use of apology, and an advance warning text-message system for transplant professionals.
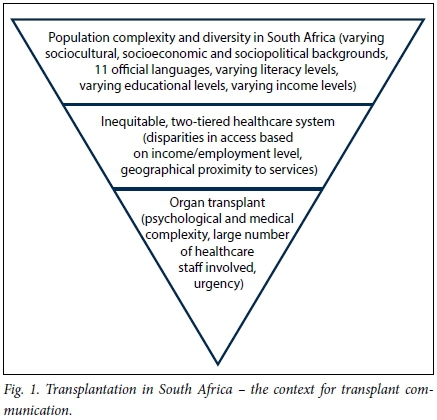
Solid-organ transplantation is the gold standard for treating patients with end-stage organ failure, and South Africa (SA) has a small but active transplant community. In the SA context, this community strives to provide transplant services to an unusually complex and diverse population, where people from different sociocultural, sociopolitical and socioeconomic backgrounds interact in any of 11 official languages. These interactions are framed by the two-tiered SA health sector, which has been criticised for inequality.[1]
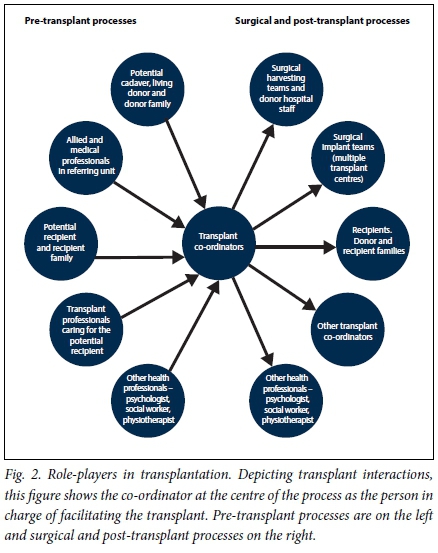
Within the complexities of context and health sector, transplantation itself is one of the most complicated and personnel-intensive interventions in medicine[2] (Fig. 1), and the number of health professionals involved speaks to its complexity (Fig. 2). This figure, based on a number of sources which, when collated, illustrate the complexities of transplantation in SA,[3-6] depicts transplant interactions. It shows the co-ordinator at the centre of the process as the person in charge of facilitating the transplant. The left-hand side of the figure shows pre-transplant processes, while the right-hand side shows the surgical and post-transplant processes.
Each of these individuals has a specific role to play, and a transplant cannot be successful unless they come together as a team with the same objective. However, these role-players are often based at different hospitals, and they are required to facilitate the transplant across a geographical divide. Moreover, a transplant needs to happen quickly. There is a finite window during which organs need to be removed from donors and implanted in order to ensure best outcomes for recipients. Because a transplant involves life, death, hope, expectation, urgency and uncertainty, the stakes are high when it comes to communication, which needs to be extensive and without which the transplant could not happen.
Communication
Communication is a cornerstone of medical care that facilitates ethical practice through conveying information, expressing emotion and clarification of instruction that accompanies the healthcare process.[7] At its most basic, healthcare involves a patient seeking medical expertise. The patient explains his or her ailment, the health professional responds, and acceptable management is determined. As health interventions become more complex, health communication extends beyond the practitioner-patient relationship into the institutional realm. Communication is a foundation of teamwork and continuity of care, and through communication patient autonomy can be enhanced and patient best interests appreciated.[8]
Teamwork
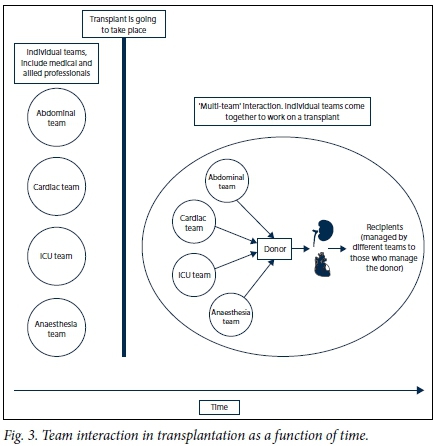
The objective of multidisciplinary, patient-centred care[9] (which is epitomised in transplantation and promotes patient autonomy) is that all of the 'individual teams' who lend their specialist skills to transplantation need to come together in a 'multi-team', interdisciplinary environment (Fig. 3). This figure is based on a comprehensive project on communication and transplantation in Gauteng Province, SA. It depicts cohesive individual teams on the left, and the thick vertical line indicates that a transplant is going to take place. At this point, all these teams must come together (portrayed on the right of the figure) and work towards the objective of transplanting chosen recipients. They are often required to work in a confined space, to travel and to be present at unusual hours, such as in the middle of the night.
Generally, the effectiveness of teams can be considered by looking at four criteria,[10] which are detailed in Fig. 4.
Continuity of care
Continuity of care involves sharing details about patient management among relevant health professionals,[11] and it requires thorough and careful communication. Continuity of care promotes beneficence and non-maleficence because it obliges health professionals to keep one another informed about patient management over a period of time, so that gaps that may affect patient care are minimised.
Study rationale
Although transplantation has been widely researched in SA,[12-15] it has not been studied through the lens of health communication, or utilising methods that lend themselves to exploring the process and impact of communication. Because communication is essential to the transplant process, the rationale for this study was to explore transplant communication in Gauteng. This is the first study of its kind in SA.
Objective
To explore communication in solid-organ transplant settings in Gauteng. Specific objectives were to: (i) explore communication aspects of solid-organ transplantation in Gauteng from a transplant professional perspective; and (ii) ascertain likely barriers to, as well as facilitators of, solid-organ transplantation in Gauteng. We aimed to present a snapshot of findings relating to interprofessional communication in transplantation, and to make some practical recommendations for its improvement.
Methods
The Human Research Ethics Committee (Medical) of the University of the Witwatersrand approved the study (ref. nos M120751 and M131041). Written informed consent was obtained from all participants. Because the transplant community in Gauteng is highly identifiable, great care was taken to anonymise data.
The study used qualitative methods and was conducted across six health institutions in Gauteng (three state and three private), which hosts the largest number of transplant centres in SA.[16] Purposeful sampling was used[17] to recruit transplant professionals and transplant co-ordinators (both procurement and recipient). The aim in sampling for each group was to reflect all transplant programmes in Gauteng, and all types of organs that were being transplanted at the time. The data presented form part of a much larger research project,[18] and only relevant methodological points are made here.
The first author (HRE) collected the data. Participants were asked about their perceptions of communication in transplantation. Data were analysed utilising Braun and Clarke's thematic analysis.[18] Codes and themes were identified, refined, defined and named by the research team.
Data analysis produced 38 codes, which fitted into three themes. Only those relevant to this article are reported here. Rigour of the study was ensured through triangulation of several data sets, reflective journaling, peer debrief, member checking and ensuring accuracy of transcriptions.[19,20]
A number of terms are used in this article, which are defined as follows:
• Transplant communication. Communication among health professionals and with patients that is related specifically to the transplant process.
• Interprofessional communication. Interactions that take place between health and/ or transplant professionals.
• Health professional. An individual who has obtained a degree in health sciences, or one that feeds into health sciences (such as social work or psychology).
• Transplant professional. A doctor or allied health professional who is involved in transplantation.
• Allied professional. Health and transplant professionals, including nurses, physical and psychological support professionals and technical assistants, who do not hold medical degrees.
Results
Study results are illustrated by verbatim quotes from participants as per qualitative research conventions, and the most important aspects of the quotes are emphasised in italics. Each quote is identified as being from a doctor or allied participant, and the original participant number is indicated. The data have been organised according to four relevant sub-themes derived during the analysis process, all of which fitted into the theme of 'interprofessional communication'.
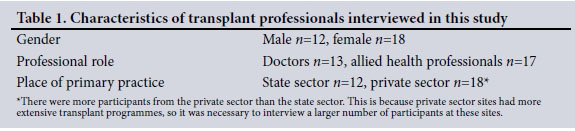
The study sample
Thirty interviews were undertaken with transplant professionals (Table 1) and two focus groups with both donor and procurement transplant co-ordinators (N=10). A table detailing transplant co-ordinator information and demographics has not been included in this article, as they are highly identifiable by these characteristics.
The transplant hierarchy
A hierarchy seems predominant among transplant professionals in Gauteng. It appears to frame interprofessional interactions and to influence the nature of transplant communication in the province. Doctors were placed at the top of the hierarchy, with allied professionals at the bottom:
'You see you have a hierarchy, and a hierarchy usually culminates with the surgeon at the top of the pinnacle'. (Doctor, 001) 'You make sure that even though [the doctor] is throwing his instruments, whatever, at the end of the day he will get his results'. (Allied professional, 008)
The notion of doctors being at the top of the hierarchy seemed rather endemic:
'„. a kind of sub-culture that gets taught to [doctors] when they go to med school about being on a pedestal or being the "knower" compared with the "auxiliary services". So you're often taught that you are the head and the nurses and everyone else are a kind of "sub class".' (Allied professional, 021)
It is worth noting that among allied professionals there were also micro-hierarchies, but these were not analysed in detail for this research because of the implications for confidentiality if participants were stratified by profession. Transplant co-ordinators appeared to be in the middle of the hierarchy, and seemed more assertive than allied professionals, expressing a sense that they would take control of difficult situations and stand up to doctors if necessary:
'And also the ability to take authority of the situation and not to be pushed by others. And as nurses who are co-ordinators, we're used to doctors telling us what to do. In this field, the co-ordinator is in charge of when to do things and needs to accept that responsibility. Because if you just do it on the demand of an outside person you are not going to get your consent.' (Transplant co-ordinator, FG1P1)
The notion of transplant co-ordinators asserting themselves more actively than other allied professionals may explain a perception of co-ordinators as:
'...HOLY NURSES. They're too too good to be nurses anymore. That's what ...' (Allied professional, 009)
Teamwork in transplantation
Across the board, transplant professionals emphasised the imperative of good team interaction as an integral aspect of their work: '... transplantation is a team sport, there's just no two ways about it' (Doctor, 002), and there was an acknowledgement of how important communication and sharing discipline-specific information is to the transplant process: we are constantly keeping each other updated with regard to our specialties' (Allied professional, 021).
Individual teams (i.e. the units of a team as an entity) were considered particularly effective by transplant professional participants, suggesting good cohesion and collective mood. This perception of well-functioning individual teams appeared to be based on a familiarity with other team members:
' I mean it's, and we have, I think evolved over the last few years and brought up a fairly constant team of people whose predominant interest is transplantation ... So we become very familiar with them and we know that and that's the advantage of having a team all the way through.' (Doctor, 005)
Newly employed or occasional team members were sometimes seen as impeding individual team cohesion:
and particularly if you're with newer people that are not asexperienced with the team, there's lots of stress involved.' (Alliedprofessional, 015)
Teamwork was less effective when cohesive individual transplant teams were required to collaborate in a multi-team environment (Fig. 3), and interaction between teams was sometimes challenging: 'The problem is not the team. The problem is the interaction between the teams. So there are various teams. And each team, I think, will, among itself, have its own view, and work very well by itself. It's the problem between the teams. So if you have a cardiac team and an abdominal team, that's the problem.' (Doctor, 002) 'There is a lot of tension, there is a lot of unhappiness a lot of the time. But between the medical "professionals" as such and the [allied] professionals there is very little communication, very very little'. (Allied professional, 009)
Continuity of care
Allied professionals expressed frustration with doctors, citing communication gaps that negatively influenced continuity of care and the quality of care provided. For instance, allied professionals sometimes felt that doctors failed to transmit important information trans-professionally:
'. .. the communication - sometimes you'll find that the doctor has just written a prescription but he didn't tell [the nursing staff], [they] find out very late that the patient was supposed to get this [medication].' (Allied professional, 006)
Doctors were critical of their medical colleagues from other institutions, who referred patients without sufficient information: 'I get a reasonable referral letter from [doctor], I get no information whatsoever from [other doctor]. So there is no liaison, zilch' (Doctor, 027). This was particularly problematic in situations involving patients listed for transplant where, for instance, a patient had become ineligible for a transplant and the doctor in charge of patient management had not alerted the transplant centre:
'. it's particularly hell of an irritating when [the patient who has been called to present for transplant] is obviously sick, that recipient, and you do get a bit irritated with your colleagues when they've had someone on the list that they know had a problem [and they have been called to come for a transplant because we have a matching organ and] they've got something wrong which precludes transplant. That is extremely annoying because it basically means that you have to re-initiate the process all over again but you are already four or five hours into ischaemic time.' (Doctor, 003)
Both doctors and allied professionals were critical of transplant co-ordinators, stating that information essential to the transplant was not always forthcoming in a timely manner:
'Not getting notified in time is a common experience for me. I see it commonly among my colleagues. It becomes frustrating when the first I hear about a transplant is when my mate . walks in and says: "I've come to see a patient pre-transplant." And that occurs with relative frequency. That's why I mention the co-ordinators in that scenario, that's their role, is to share that information. So that has been a source of frustration. But we get around it.' (Doctor, 016)
In response to some of these challenges, professionals explained novel mechanisms they developed to obtain information. One allied professional had negotiated an arrangement with a transplant co-ordinator where:
as soon as there's [an organ] that [the co-ordinator is] aware of she will SMS [text] me: "Prepare yourself, there's [an organ] coming. Don't know when, maybe this time, maybe that time." At least I know about it and I will start calling the hospital and find out what's going on.' (Allied professional, 007)
Aggression in transplantation
Communication gaps could sometimes result in aggressive behaviour: 'If the message is delivered in a short time it's really very stressful . it causes some friction when the transplant is not well organised. Sometimes we have big problems.' (Allied professional, 017)
Conflict seemed heightened during the frenetic phase of organ retrieval from a brain stem death donor in theatre, where several teams interact under marked time pressure:
'In the actual operating theatre is a bunch of prima donna surgeons each saying that their organ is the only one that is important and screw the other organs. And depending on who the surgeons are it can be quite rough.' (Doctor, 014)
This type of behaviour was seen to discourage health professionals from taking part in transplantation and possibly becoming transplant specialists, with sentiments such as:
'. and I said: "No, I am stopping. I am stopping and I am not going to harvest anymore."' (Allied professional, 017)
However, the notion that there was a patient at the end of the process also spurred transplant professionals to continue working under these circumstances:
'If patient care plays any role, it plays a role in [the teams] tolerating that kind of stuff. If it plays a role, it's probably the only thing that stops [the teams] from killing each other. You say: "Fine, there's a ... patient on the other side of this" so you are very annoyed there has been a delay of two hours, but you tolerate it because there's a patient at the end of it.' (Doctor, 002)
Some participants had developed mechanisms to cope with aggressive behaviour, which primarily involved being calm, rational and unemotional:
And then, ja, and then obviously I'm not going to make a big noise, shout and scream and carry on like that because there's better ways to handle the situation.' (Allied professional, 007)
' You actually get more right being nice than screaming and shouting. Because I think it's already such a sensitive situation. You can go and 'shout and scream1 outside, but you don't scream and shout at the person. Because you might get more out of being actually nice.' (Transplant co-ordinator, FG2P1)
Discussion
Participants seemed aware of the crucial need for careful communication to facilitate successful organ transplantation in Gauteng. The importance of teamwork was recognised and a strong sense of cohesion among individual transplant teams was observed. However, there appear to be a number of barriers to interprofessional communication. This is cause for concern, because effective communication is an essential foundation for ethical practice and providing optimal patient care.[3,21] Communication breakdowns that impact on patient care or result in aggressive behaviour can have profound effects on some transplant professionals, possibly resulting in moral distress and their leaving the profession.
Findings from Gauteng may not be entirely surprising, considering the influence of SA's complex healthcare context, the complicated nature of transplantation and the large number of stakeholders involved (Fig. 2). As medical interventions become more complex, so too does the communication that must necessarily take place within them. Transplantation represents all this complexity.
Transplantation in Gauteng appears to be distinctly hierarchical. While hierarchy is a feature of many health settings,'221 in transplantation the hierarchy was found to be especially acute, possibly because of the number of professionals involved and the high-stakes nature of the intervention. This hierarchy influences interprofessional communication and frames interactions. Doctors, at the top of the hierarchy, were sometimes seen to communicate inadequately, while allied professionals, at the bottom of the hierarchy, were not always included in communication and did not appear to be communicating actively with those at the top to any substantial extent. Lupton'221 argues that healthcare hierarchies are constructed according to position in society, and locates the essence of the healthcare hierarchy as a convergence of asymmetries in status, gender and the types of tasks performed. For instance, a general perception that allied professionals are involved in less complex tasks than doctors'221 may explain why allied participants in Gauteng often saw their role as one of following orders - without scope to engage with doctors by offering opinions or asking questions. Transplant co-ordinators were in the middle of the hierarchy, and seemed more assertive than allied professionals, which may be due to the more complex tasks transplant co-ordinators undertake.
Continuity of care across transplantation in Gauteng was found to be variable, with gaps in communication and instances where transplant professionals were not informed of all the necessary facts. In order to act in the best interests of a patient, it is important that health providers have all relevant information communicated to them,'231 and communication failures are one of the most significant risks to patients in the healthcare setting.[24] When information was not passed on effectively in Gauteng transplantation, patient care sometimes seemed compromised, for instance when organ quality diminished (as a result of increased ischaemic time) because of delays resulting from miscommunication.
Strong cohesion, good collective mood and collective efficacy were found among individual transplant teams. This was framed by mutual support, understanding and shared objectives. It may also be helpful that these teams work within institutional boundaries and in close geographical proximity, often in the same hospital complex. [2] The main factor limiting individual teams was new or irregular team members who had not been assimilated into the team culture, creating uncertainty. [25,26]
'Interservice challenges', which refers to the interaction between individual teams contributing to the transplant process, were identified in multi-team interaction.[3] These mainly related to timetables and geographical proximity, when professionals were too busy to communicate or late for procedures or where continuity of care was inadequate, especially across institutions in Gauteng. In transplantation, it is essential that teams interact effectively in order to prevent delays that could compromise organ quality and thus may also affect the mandate to provide care in the best interests of the recipient.
Sometimes there was friction between surgical teams in Gauteng transplantation, and aggressive behaviour directed towards other professionals. Disruptive and aggressive behaviour has been found to have a direct impact on patient safety.[25,27,28] The extent to which aggressive behaviour affects patient best interests in Gauteng transplantation is unclear from these study results, because participants noted that they would continue to actively participate in transplantation because they were cognisant of the potential recipient at the end of the process.
Aggression seems to be shaped by the healthcare hierarchy, and disrespectful interchanges have been confirmed in international publications.[28] It has been found that allied professionals who were on the receiving end of aggressive behaviour did little to mitigate the situation, rather choosing to accept it within the framework of shame. This feeling of being shamed resulted in attitudes of 'self-blame' and 'avoidance' which are psychologically damaging[29] and can lead to moral distress.
Moral distress is a sensation of frustration and failure when health professionals are aware of their obligations to patients, but feel unable to fulfil their fiduciary duty because of external constraints to their role in patient care.'301 It appears that allied professionals did not stand up for themselves, preferring to be 'nice and calm' than to question the status quo or object to aggressive behaviour. They did not always feel empowered to request information that would be considered essential for patient care. Allied professional participants acknowledged that aggressive behaviour and inadequate continuity of care could negatively affect patients, but seemed prevented from actively doing anything about it because of their position in the hierarchy.[30] This led to moral distress. Moral distress in healthcare is seen as a reason for leaving the profession.
The qualitative design of this study allowed for a particularly detailed exploration of interprofessional transplant communication in Gauteng,[19,31,32] and it has enabled identification of a number of barriers to and facilitators of transplantation that have not previously been reported in SA academic literature. The value of qualitative research in health sciences is sometimes questioned, because results are not seen to be generalisable. However, it is widely argued that qualitative research enhances 'understanding' because it allows for exploration of aspects that, owing to their abstract and complex nature, are not conventionally quantifiable.[19,33] Communication is one such concept.
Recommendations
Some participants had developed mechanisms to overcome communication gaps, and combined with synthesis of relevant literature and the findings of this study, these inform the following recommendations.
• Communication specialist. Integrating a communication specialist into the transplant process in Gauteng may assist in promoting better communication, as this role would involve trouble-shooting and promoting new communication strategies that could lead to improvements.
• Teamwork - 'knotworking'. Multi-team communication challenges arise under time pressure and are influenced by the unpredictability of transplantation. 'Knotworking' - rapid negotiating and trouble-shooting to solve problems in real time - may be helpful in these situations.[3]
• Aggressive behaviour - apology. It may be helpful for transplant professionals to consider the role of apology in mitigating aggressive behaviour, because it could help to restore trust between role-players. [34] Ideally, aggressive behaviour would be minimised and a sense of accountability for behaving in such a manner would be instilled.
• Continuity of care - advance warning system. A text message-based advance warning system could contain the contact details of all healthcare professionals involved in Gauteng transplantation. When there is a potential transplant, a nominated co-ordinator could send a brief text message alert to all staff. The message need not be detailed, because staff could decide how to respond based on their call status and could take steps to elicit more information about the transplant if there is a likelihood of their being involved. An advance warning system may have benefits in helping to improve continuity of care and cohesion in Gauteng transplantation. It may also promote professional autonomy by allowing time to rearrange personal and professional schedules if necessary. Furthermore, this system is relatively simple. While there is scope to recommend a more sophisticated telecommunication transplant algorithm, such an intervention may be very expensive, and even the recommendation made here may face barriers in an upper-middle-income country like SA, because sufficient resources may not always be available to implement it effectively.
Study limitations
This study had a number of limitations. It took place across a single province, the sample size was small (although this is appropriate for qualitative research), and paediatric transplantation was not included.
Conclusion
Participants in Gauteng appreciated that good communication is essential to optimal transplant practice, and pockets of effective communication were identified. However, a healthcare hierarchy seemed to affect interprofessional communication, and inadequate continuity of care, aggressive behaviour and difficult team interaction were also found.
The findings presented in this article may not be unique to organ transplantation, and could occur across other medical specialties. However, the complex transplant context, with its inherent physiological challenges and large number of role-players, makes it especially susceptible to communication breakdowns. Addressing these issues in Gauteng is essential to heightening ethical practice and limiting moral distress. Future research could include exploring transplant communication in other regions of SA, and patient-orientated projects, although ethically challenging, may also enhance our understanding of these phenomena.
Acknowledgements. None.
Author contributions. HRE: field work, analysis, first draft; CP: supervision, analysis, feedback on article; JW: supervision, analysis, feedback on article.
Funding. Funding was received from the National Research Foundation, SANPAD (the South Africa-Netherlands Research Programme on Alternatives in Development) and the Oppenheimer Memorial Trust.
Conflicts of interest. None.
References
1. Mayosi BM, Benatar SR. Health and health care in South Africa - 20 years after Mandela. N Engl J Med 2014,371(14):1344-1353. http://doi.org/10.1056/NEJMsr1405012 [ Links ]
2. Etheredge HR. 'Hey sister! Where's my kidney?' - exploring ethics and communication in organ transplantation in Gauteng Province, South Africa. PhD thesis. Johannesburg: University of the Witwatersrand, 2015. http://wiredspace.wits.ac.za/handle/10539/21425 (accessed 26 January 2017). [ Links ]
3. Lingard L, McDougall A, Levstik M, Chandok N, Spafford MM, Schryer C. Representing complexity well: A story about teamwork, with implications for how we teach collaboration. Med Educ 2012;46(6):869-877. http://doi.org/10.1111/j.1365-2923.2012.04339.x [ Links ]
4. Baldwin-Ragavan L, de Gruchy J, London L. An Ambulance ofthe Wrong Colour. Cape Town: University of Cape Town Press, 1999. [ Links ]
5. Mesthrie R. South Africa: A sociolinguistic overview. In: Mesthrie R, ed. Language in South Africa. Cambridge, UK: Cambridge University Press, 2002:11-27. [ Links ]
6. Hassim A, Heywood M, Burger J. Health and Democracy. Cape Town: Siberink, 2007. [ Links ]
7. Schiavo R. Health Communication: From Theory to Practice. 2nd ed. Hoboken, NJ: Jossey-Bass, 2013. [ Links ]
8. Lindberg C, Fagerstrõm C, Sivberg B, Willman A. Concept analysis: Patient autonomy in a caring context. J Adv Nurs 2014;70(10):2208-2221. http://doi.org/10.1111/jan.12412 [ Links ]
9. McGee S. Patient centered health care in South Africa. BRICS Forum - ISPOR International Congress. 23 May 2016. https://www.ispor.org/Event/GetReleasedPresentation/630 (accessed 26 Janaury 2017). [ Links ]
10. Cornell University ILR School. Kozlowski SWJ, Bell BS. Work Groups and Teams in Organizations. 2001. http://digtdcommons.ür.cornefledu/cgi/viewcontent.cgi?article=1396&context=artides (accessed 26 January 2017). [ Links ]
11. Tousignant P, Diop M, Fournier M, et al. Validation of 2 new measures of continuity of care based on year-to-year follow-up with known providers of health care. Ann Fam Med 2014;12(6):559-567. http://doi.org/10.1370/afm.1692 [ Links ]
12. Fabian J, Maher H, Bentley A, et al. Favourable outcomes for the first 10 years of kidney and pancreas transplantation at Wits Donald Gordon Medical Centre, Johannesburg, South Africa. S Afr Med J 2016;106(2):172-176. http://doi.org/10.7196/SAMJ.2016.v106i2.10190 [ Links ]
13. Etheredge H, Turner R, Kahn D. Public attitudes to organ donation among a sample of urban-dwelling South African adults: A 2012 study. Clin Transplant 2013;27(5):684-692. http://doi.org/10.1111/ctr.12200 [ Links ]
14. Labuschagne D. An analysis of organ transplantation in South Africa with specific reference to organ procurement. UP Institutional Repository. 2013. http://repository.up.ac.za/bitstream/handle/2263/40613/Labuschagne_Analysis_2013.pdf?sequence= (accessed 26 January 2017). [ Links ]
15. Ndlovu S, Kobryn AM, Modiba M. Attitudes of black South Africans concerning organ donation. J Transpl Coord 1998;8(4):241-242. [ Links ]
16. Organ Donor Foundation of South Africa. Transplant Centres. 2017. https://www.odf.org.za/ (accessed 26 January 2017). [ Links ]
17. Marshall C, Rossman GB. Designing Qualitative Research. 5th ed. Thousand Oaks, Calif.: Sage, 2014. [ Links ]
18. Braun V, Clarke V. Thematic analysis. In: Teo T, ed. Encyclopedia of Critical Psychology. New York: Springer, 2014:1947-1952. [ Links ]
19. Malterud K. Qualitative research: Standards, challenges, and guidelines. Lancet 2001;358(9280):483-488. http://doi.org/10.1016/S0140-6736(01)05627-6 [ Links ]
20. Green J, Thorogood N. Qualitative Methods for Health Research. 3rd ed. London: Sage, 2014. [ Links ]
21. Samela K, Fennelly E, Brosnan M, Robinson J. Interdisciplinary approach to the management of intestinal transplant recipients: Evaluation, discharge, and lifetime management. Prog Transplant 2005;15(1):54-59. http://doi.org/10.7182/prtr.15.Lk601342358250414 [ Links ]
22. Lupton D. Medicine as Culture. 2nd ed. Thousand Oaks, Calif.: Sage, 2003. [ Links ]
23. Reach G. Patient autonomy in chronic care: Solving a paradox. Patient Prefer Adherence 2014;12(8):15-24. http://doi.org/10.2147/PPA.S55022 [ Links ]
24. Sutcliffe KM, Lewton E, Rosenthal MM. Communication failures: An insidious contributor to medical mishaps. Acad Med 2004;79(2):186-194. [ Links ]
25. Porto G, Lauve R. Disruptive clinical behavior: A persistent threat to patient safety. Pat Saf Qual Healthc 2006;3:16-24. [ Links ]
26. Treadwell I, van Rooyen M, Havenga H, Theron M. The effect of an interprofessional clinical simulation on medical students. Afr J Health Prof Educ 2014;6(1):3-5. http://doi.org/10.7196/AJHPE.231 [ Links ]
27. Galandiuk S. Surgical behaviour. Br J Surg 2013;100(s6):34-35. http://doi.org/10.1002/bjs.9147 [ Links ]
28. Katz JD. Conflict and its resolution in the operating room. J Clin Anesth 2007;19(2):152-158. http://doi.org/10.1016/j.jclinane.2006.07.007 [ Links ]
29. Felblinger DM. Incivility and bullying in the workplace and nurses' shame responses. J Obstet Gynecol Neonatal Nurs 2008;37(2):234-242. http://doi.org/10.1111/j.1552-6909.2008.00227.x [ Links ]
30. Austin W, Lemermeyer G, Goldberg L, Bergum V, Johnson MS. Moral distress in healthcare practice: The situation ofnurses. HEC Forum 2005;17(1):33-48. http://doi.org/10.1007/s10730-005-4949-1 [ Links ]
31. Barbour RS. The role of qualitative research in broadening the evidence base for clinical practice. J Eval Clin Pract 2000;6(2):155-163. http://doi.org/10.1046/j.1365-2753.2000.00213.x [ Links ]
32. Silverman D. Doing Qualitative Research. 3rd ed. Thousand Oaks, Calif.: Sage, 2010. [ Links ]
33. Jones R. Why do qualitative research? It should begin to close the gap between the sciences of discovery and implementation. BMJ 1995;311(6996):2. [ Links ]
34. Lin N. Restoring trust: The role of apology in preventing hospital violence in China. Presented at the Australian Association of Bioethics and Health Law Conference - How Should We Decide? Perth, Australia, 2 - 4 October 2014. [ Links ]
 Correspondence:
Correspondence:
H R Etheredge
harriet.etheredge@mediclinic.co.za
Accepted 9 March 2017














