Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.107 no.6 Pretoria Jun. 2017
http://dx.doi.org/10.7196/samj.2017.v107i6.12296
RESEARCH
Characteristics and outcomes of gunshot-acquired spinal cord injury in South Africa
C Joseph
RPT, PhD; Physiotherapy Department, Community and Health Sciences Faculty, University of the Western Cape, Cape Town, South Africa; and Physiotherapy Division, Department of Neurobiology, Care Sciences and Society, Karolinska Institutet, Stockholm, Sweden
ABSTRACT
BACKGROUND. Spinal cord injuries (SCIs) caused by assault present a unique challenge facing the healthcare system, in that very little is known about how these injuries manifest compared with other causes of injury. Understanding the nuances of gunshot SCIs could contribute towards better care provision.
OBJECTIVE. To determine the characteristics of gunshot SCI and compare both injury characteristics and outcomes between gunshot SCI and all other traumatic causes taken together.
METHODS. The gunshot SCI sub-cohort was derived from a 1-year prospective, population-based study, including both tertiary-level hospitals providing SCI care in the Cape Metropolitan area of South Africa (SA). All consenting 145 survivors, after a window period of 7 days, were included, and their demographic and injury characteristics were captured according to the International SCI Core Basic Data Set. Further, selected secondary medical complications (outcomes) were prospectively and routinely assessed throughout acute care. Both descriptive and inferential statistics were used to describe and compare characteristics and outcomes, respectively.
RESULTS. Of the 145 survivors of traumatic SCIs, 45 (31%) injuries were caused by gunshots. The gunshot SCI group consisted mainly of males (n=43; 96%), and the average age of injury onset was 26 years. Most survivors of the gunshot SCI group were paraplegic (69%), had complete lesions (69%) and vertebral injuries (96%), and presented with significant associated injuries (84%). When comparing gunshot SCI with all other traumatic causes, significant differences were found in relation to demographic and injury characteristics and adverse outcomes, indicating that those survivors with gunshot SCI were typically younger males with complete paraplegia, had more frequent secondary medical complications, and a longer hospital stay.
CONCLUSION. This study contributes to the knowledge base of survivors with gunshot SCIs in a region of SA. Efforts should be made to reduce the occurrence of all gunshot SCIs, since those injuries impact survivors negatively in terms of injury characteristics and adverse outcomes.
The occurrence of traumatic spinal cord injuries (TSCIs) does not seem to decline globally, despite the implementation of costly prevention campaigns and programmes.[1,2] What further challenges the discourse is the perceived increase in the prevalence of TSCIs, which, at the same time, is understood as an achievement, since improved medical and rehabilitation care is partly responsible for this - causing patients to live longer with fewer complications.[3] A fraction of the multifaceted issues regarding TSCI prevention may relate to knowledge and understanding of the causes of injury, in that these insights could guide appropriate preventive strategies. The research community has made significant strides in that regard, and we now know that causes of injury differ between continents,[4,5] let alone countries.[6] However, our knowledge of differences in characteristics and outcomes across causes of injury remains insufficient. Understanding the nuances associated with different types of injury is necessary for augmenting health systems, but also for informing primary preventive strategies in an attempt to curb certain types of injuries that are prone to be costly and to negatively impact an individual.
Gunshots resulting in spinal cord injuries (SCIs) are common in certain countries, especially in areas of conflict and in low-income countries.[6] It was only recently established that assault, i.e. gunshots, stab wounds and use of non-penetrating objects, was the leading cause of TSCI, causing ~60% of casualties in the Cape Metropolitan region of South Africa (SA).[7] Previous studies have found that gunshot-acquired SCIs mainly affect males'8,91 and those with lower socioeconomic status,[10] and result in complete lesions.[11,12] A previous descriptive study conducted in SA by Le Roux and Dunn[11] found that gunshot injuries resulted in poor neurological recovery, a substantial proportion of injured individuals with associated injuries, and a few in-hospital deaths. However, very little is known about the differences in characteristics and outcomes between gunshot-related and other more homogenous causes of injury, information that is necessary to evaluate the appropriateness of current management plans for gunshot SCI. Understanding the unique characteristics and impact of gunshot SCI could contribute to the planning of more targeted preventive strategies.
The objectives of the current study were: (i) to determine the characteristics of gunshot-acquired TSCIs; and (ii) to evaluate if any differences in characteristics and outcomes exist between injuries caused by gunshot and all other traumatic causes, as derived from a population-based cohort.
Methods
Design and setting
A population-based cohort design was used to prospectively identify all survivors of acute TSCIs within the Cape Metropolitan area of SA, with the full methodology described in a previous publication by Joseph et al.[7]The current study specifically concerns the group of survivors who acquired their injuries through gunshots, with the aim of assessing resultant injury characteristics and outcomes. Data were collected at both tertiary hospitals managing SCIs within the catchment area for a 1-year period, between September 2013 and September 2014.
It is well known that ~90% of violence-related injuries occur in low- to middle-income countries, and that they deplete healthcare budgets considerably.[13] In 2015, Cape Town registered 2 451 homicides among a population of 3.74 million people, giving it a rate of 65.53 per 100 000 people.[14] This figure suggests that this region of SA is ninth on the list of the most dangerous cities in the world. It was therefore important to have a closer look at this group, i.e. those injured by gunshots, owing to the high crime rate and prevalence of gang-related activities in certain locations within the catchment area.
Inclusion, variables and procedure
All patients satisfying the following criteria were eligible to take part in the study: (i) showing abnormal imaging, such as with magnetic resonance imaging scan or multislice computer tomography scan, confirming an acute TSCI or cauda equina lesion; (ii) the injury resulting in persisting impairment (i.e. not just a concussion) after emergence from neurogenic shock, which generally occurs within the first 24 - 72 hours after injury; (iii) being age 18 years or older; (iv) surviving at least 7 days post trauma; (v) admittance to the hospitals that are designated to manage SCI; and (vi) legitimately residing in the Cape Metropolitan area of SA.
As recommended by the International Spinal Cord Society, the International Spinal Cord Injury Basic Data Set was selected and used to, in its brevity, provide an adequate picture of injury characteristics of eligible survivors of TSCI. Items of the SCI basic dataset covered the following areas: demographics; cause of injury; additional injuries; and severity of injury according to international standards of classification. All variables of the SCI basic core set were routinely captured in the medical records of all patients on admission to either the Level 1 Trauma Units or the Acute Spinal Cord Injury Unit, with the exception of injury severity, which was also assessed at discharge. Qualified neurologists performed the neurological assessments according to international guidelines within 3 days after injury onset.[15] For the purpose of this study, the most common secondary complications were checked on a weekly basis during ward rounds, and if any were present, the nature of the complication, along with its management plan, was noted. Complications were limited to the following: pressure ulcers; pulmonary complications, including atelectasis and pneumonia; urinary tract infection; deep-vein thrombosis; neuropathic pain; pulmonary embolism; orthostatic hypotension; and autonomic dysreflexia.
Data analysis and ethics
For the description of survivors with gunshot-acquired SCI, descriptive statistics were used. Output was expressed as counts with percentage, and in the case of continuous variables, i.e. age and length of hospital stay, mean with standard deviation (SD) and median with interquartile range (IQR) were presented, depending on the normality of the data. For the assessment of differences in injury characteristics between causes of injury, we decided to dichotomise the variable 'causes of injury', as operationalised in the International SCI Core Basic Data Set, into gunshot-acquired and all other traumatic causes grouped together. The reader should keep in mind that although stab wounds and non-penetrating assault trauma are subsumed within the assault category - of which gunshots are part - they were collapsed together with motor vehicle accidents and falls, since no significant differences were found across them in relation to characteristics and outcomes. As such, the focus of this study remained completely on gunshot-acquired SCI. Concerning the comparative analysis between the two groups (gunshot-acquired and all other traumatic causes of SCI), χ2 and Fisher's exact tests were used. When comparable variables were continuous, either Student's t-test or the Mann-Whitney (7-test was used, with the final decision depending on the normality of the data.
The Senate Research Committee of the University of the Western Cape approved the project prior to the start of data collection (ref. no. 13/4/27). Further, we certify that all other institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Results
Subpopulation characteristics
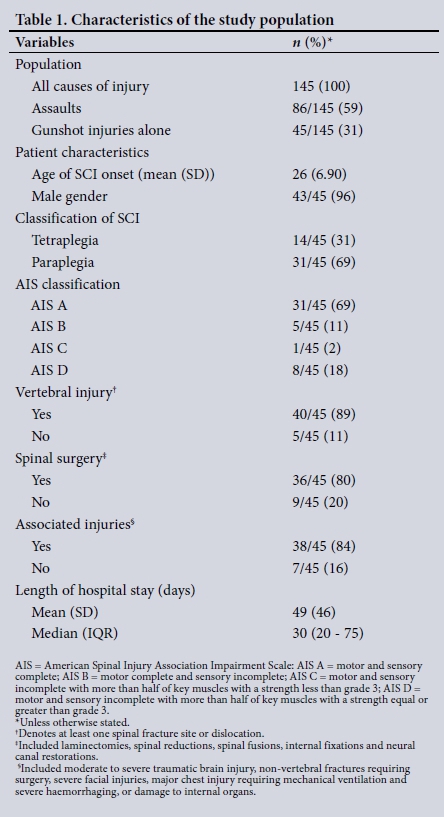
As seen in Table 1, 145 persons sustained an SCI due to traumatic causes during the surveillance period. The leading cause of injury was assault (n=86, 59.3%), followed by transport-related accidents (n=38, 26.3%), falls (n=17, 11.7%) and one sports injury, while three were categorised as 'other traumatic cause'. Of the assault-related SCIs, the majority were caused by gunshots, followed by stab wounds (n=28, 33%) and non-penetrating blunt trauma, such as getting struck by a brick (n=13, 15%). Our analysis that specifically concerned gunshot SCIs found that the mean age of injury onset was 26 years, while males were almost exclusively the victims. The majority (n=31, 69%) of SCIs resulted in complete paraplegia. Furthermore, most gunshot SCIs were accompanied by marked vertebral injuries (n=40, 89%), while all except four persons with such injuries were surgically managed, and the majority (n=38, 84%) of persons had at least one associated injury.
Comparison of characteristics between gunshot and all other traumatic causes of SCI
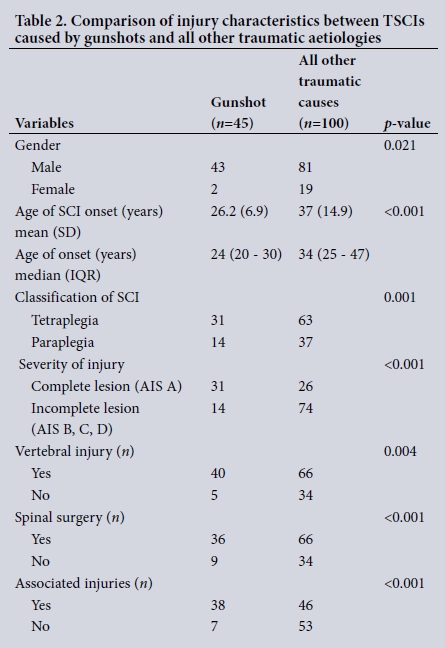
As seen in Table 2, significantly more males sustained their SCIs due to gunshots compared with all other traumatic causes. The mean age difference of injury onset between the two groups was ~10 years. The levels, i.e. tetraplegia v. paraplegia, and severity, i.e. complete v. incomplete, of injuries were significantly different between the groups, with more complete paraplegic survivors among the gunshot SCI group. Significant differences were found between the groups in relation to the proportion of survivors who had undergone spinal surgery due to vertebral injuries, and those who presented with associated injuries, with those affected by gunshots being more frequent.
Secondary complications
The findings revealed that the proportion of those with gunshot injuries had significantly more complications (at least one) than the other group. Significant differences in specific complications between the two groups related to the following: pulmonary complications (p=0.004); pressure ulcers (p<0.001); deep-vein thrombosis (p=0.006); and neuropathic pain (p=0.006). No differences were found in the proportions of those with urinary tract infections, autonomic dysreflexia, pulmonary embolism and postural hypotension between the two groups (Table 3).
Length of acute hospital stay
Hospital stay was significantly (p=0.006) longer for those having gunshot SCI compared with all other traumatic causes.
Discussion
This study investigated the characteristics and selected outcomes of gunshot-acquired SCI and the way in which they differ from all other traumatic causes of injury. Our findings revealed that survivors of TSCIs due to gunshots tended to be younger males who have more severe injuries. They further presented with more frequent secondary medical complications, and remained in hospital longer, compared with those who sustained their SCI due to other traumatic causes.
The leading cause of TSCIs in SA is assault, and most injuries are due to gunshots, followed by stab wounds and then non-penetrating blunt trauma.[7] The current investigation found that the mean age of gunshot-acquired SCI was 26 years, which was, on average, ~10 years younger than those with SCI owing to other traumatic causes. Our finding concerning the younger age onset of gunshot SCI corroborates with a previous hospital-based study conducted within the catchment area.[11] However, in contrast to the aforementioned referenced study, we found a significantly higher proportion of males to be victims of gunshot injuries. It seems necessary to identify factors that place younger men at risk of engaging in interpersonal violence and also investigate whether perpetrators are valid firearm-licence holders, since 16 persons are shot and killed each day, i.e. ~6 000 per year, in SA.[16] Another important issue to consider in SA is the high number of illegal/stolen guns that are circulating in society, necessitating the need to enforce stricter firearm control acts and confiscate guns found in possession of unauthorised users.[17]
The level and severity of injury after an SCI have a profound impact on the capabilities of survivors. In the current study, most survivors with gunshot SCI had resultant paraplegia, and most injuries were AIS A, indicating the absence of sensory and motor sparing at the sacral nerve roots. Also, the majority of survivors had a vertebral injury that in most cases required surgical management, and presented with at least one associated injury. Injury level and severity, along with vertebral and associated injuries, significantly differed between the groups under study, leaving those with gunshot SCI more negatively affected. Gunshots to the spine typically resulted in complete SCI, along with significant associated injuries, owing to multiple mechanisms of tissue damage, i.e. the direct impact of the bullet, the pressure of shock waves, and temporary cavitation.[8] It is difficult to assess from our data the type of firearm, i.e. low- or high-velocity weapon, predominantly used, although the literature indicates that low-velocity firearms are typically in use among civilians,[8,18] and given that almost all gunshot SCIs resulted in direct vertebral injuries and complete lesions. Again, an audit of firearm use in SA is necessary in order to ensure that military weapons, i.e. highvelocity guns, which may cause more detrimental damage or death, are not illegally in the hands of civilians, and that only registered and 'fit' persons possess an appropriate gun.
Secondary medical complications are common following the onset of TSCI.[19] We found in the current study that gunshot SCI resulted in a significantly higher proportion of complications, with pressure ulcers being the most common, followed by pulmonary complications, deep-vein thrombosis and neuropathic pain. A recent study by Chopra et aí.[20] found pressure ulcers to be one of the leading causes of hospital readmission, which result in high healthcare costs that could be prevented with a fraction of the resultant costs of managing ulcers. Previous studies have found that those with complete injuries were at greater risk of developing pressure ulcers;[19,21-23] however, this need not be the case since the majority of survivors with gunshot SCI had paraplegia, leaving their upper limb function intact. It is therefore necessary to educate healthcare personnel and patients with gunshot SCIs and their families on the importance of remaining free from pressure ulcers and the positive effects of regular turning and pressure relief. Concerning pulmonary complications, we found the increased number of survivors with gunshot SCI slightly unexpected, since most injuries were situated in the thoracic back, indicating normal nerve innervation of the diaphragm. We speculate that this could be due to the fact that almost all patients with gunshot SCI presented with significant associated injuries, i.e. moderate to severe traumatic brain injury, non-vertebral fractures requiring surgery, severe facial injuries, major chest injury and severe haemorrhaging or damage to internal organs, requiring mechanical ventilation,[24] which, in turn, results in a greater risk of pulmonary complications.
Unlike the preventable secondary medical complications, neuropathic pain comes with the territory, where even the removal of the bullet is not associated with the resolution of pain. Neuropathic pain has been found to influence participation and quality of life after SCI onset,[25] and should therefore be managed by administering tricyclic antidepressants[26] or anticonvulsants.[27]
The median length of hospital stay of those with gunshot SCI was 30 days, significantly different when compared with 22 days for the other trauma group. A previous local study conducted by Le Roux and Dunn[11] in 2005 found exactly the same result, indicating a length of acute stay of 30 days, and from the current data, we now know that this is significantly longer than the stay of other groups of TSCI patients. Future studies should therefore investigate possible modifiable factors related to longer durations of acute hospital stay. Alternatively, an investigation into the current management protocols for gunshot SCI should be made in order to assess whether operative standards and guidelines are followed.
Limitations
This study provides valuable insights into a previously unknown subcohort with TSCIs in SA. However, this study had limitations that should be considered. Firstly, although the sample size for the group with gunshot SCI was sufficient, the other assault-related groups, i.e. stab wounds and non-penetrating trauma, were of smaller size. It would have been ideal to analyse each assault-related specific cause separately in order to establish the impact of each. Importantly, as mentioned earlier, the other assault-related groups, when taken together, did not differ when compared with other causes of injury, specifically motor vehicle accidents and falls. Secondly, we failed to collect information on children with gunshot- or other assault-related SCI. Thirdly, we did not collect information about the kind of bullets commonly found, which may have indicated the type of weapon used, and subsequently informed firearm audits within the region. Lastly, we do not know the association between secondary medical complications and length of hospital stay, specifically, whether the onset of a particular complication resulted in a longer stay. This information is necessary in order to avert complications in the future. To gain a more comprehensive picture of the true burden of gunshot SCI, future studies should include the surveillance of all ages and those who die at the time of the accident/or within 7 days of injury. Furthermore, mortality/survival status of those with gunshot SCI should be determined.
Conclusion
This study contributes to the knowledge base of survivors with gunshot SCIs in the Cape Metropolitan region of SA, in showing that they are typically very young adult males with complete paraplegia as the most common injury, having significant associated injuries and frequent secondary medical complications, and remaining in hospital for a significantly longer time. Therefore, efforts should be made to reduce the occurrence of all assault-related SCIs, specifically those caused by gunshots, by raising awareness that is informed by a better understanding of how conflict and interpersonal violence arise in the local context. Further research is required to better understand the current management of gunshot SCI in order to facilitate the strengthening of healthcare services for this vulnerable group.
Acknowledgements. The author would like to thank all survivors of TSCIs who participated in this study, and also the Medical Research Council of South Africa for financial assistance to write this article.
Conflicts of interest. None.
Funding. None.
References
1. Bellon K, Kolakowsky-Hayner SA, Chen D, McDowell S, Bitterman B, Klaas SJ. Evidence-based practice in primary prevention of spinal cord injury. Top Spinal Cord Inj Rehabil 2013;19(1):25-30. https://doi.org/10.1310/sci1901-25 [ Links ]
2. Furlan JC, Sakakibara BM, Miller WC, Krassioukov AV. Global incidence and prevalence of traumatic spinal cord injury. Can J Neurol Sci 2013;40(4):456-464. https://doi.org/10.1017/S0317167100014530 [ Links ]
3. Parent S, Barchi S, LeBreton M, Casha S, Fehlings MG. The impact of specialized centers of care for spinal cord injury on length of stay, complications, and mortality: A systematic review of the literature. J Neurotrauma 2011;28(8):1363-1370. https://doi.org/10.1089/neu.2009.1151 [ Links ]
4. Lee BB, Cripps RA, Fitzharris M, Wing PC. The global map for traumatic spinal cord injury epidemiology: Update 2011, global incidence rate. Spinal Cord 2014;52(2):110-116. https://doi.org/10.1038/sc.2012.158 [ Links ]
5. Jazayeri SB, Beygi S, Shokraneh F, Hagen EM, Rahimi-Movaghar V. Incidence of traumatic spinal cord injury worldwide: A systematic review. Eur Spine J 201524(5):905-918. https://doi.org/10.1007/s00586-014-3424-6 [ Links ]
6. Rahimi-Movaghar V, Sayyah MK, Akbari H, et al Epidemiology oftraumatic spinal cord injury in developing countries: A systematic review. Neuroepidemiology 2013;41(2): 65-85. https://doi.org/10.1159/000350710 [ Links ]
7. Joseph C, Delcarme A, Vlok I, Wahman K, Phillips J, Nilsson Wikmar L. Incidence and aetiology of traumatic spinal cord injury in Cape Town, South Africa: A prospective, population-based study. Spinal Cord 2015;53(9):692-696. https://doi.org/10.1038/sc.2015.51 [ Links ]
8. Sidhu GS, Ghag A, Prokuski V, Vaccaro AR, Radcliff KE. Civilian gunshot injuries of the spinal cord: A systematic review of the current literature. Clin Orthop Relat Res 2013;47(12):3945-3955. https://doi.org/10.1007/s11999-013-2901-2 [ Links ]
9. Cook PJ, Lawrence BA, Ludwig J, Miller TR. The medical costs of gunshot injuries in the United States. JAMA 1999;282(5):447-454. https://doi.org/10.1001/jama.282.5.447 [ Links ]
10. Gur A, Kemaloglu MS, Cevik R, et al. Characteristics of traumatic spinal cord injuries in southeastern Anatolia, Turkey: A comparative approach to 10 years' experience. Int J Rehabil Res 2005;28(1):57-62. https://doi.org/10.1097/00004356-200503000-00008 [ Links ]
11. Le Roux JC, Dunn RN. Gunshot injuries of the spine - a review of 49 cases managed at the Groote Schuur Acute Spinal Cord Injury Unit. S Afr J Surg 2005;43(4):165-168. [ Links ]
12. Romanick PC, Smith TK, Kopaniky DR, Oldfield D. Infection about the spine associated with low-velocity-missile injury to the abdomen. J Bone Joint Surg Am 1985;67(8):1195-1201. https://doi.org/10.2106/00004623-198567080-00008 [ Links ]
13. Matzopoulos R, Bowman B, Butchart A, Mercy JA. The impact of violence on health in low- to middle-income countries. Int J Inj Contr Saf Promot 2008;15(4):177-187. https://doi.org/10.1080/17457300802396487 [ Links ]
14. Crime Statistics South Africa. Official database of crime-related activities in South Africa. http://www.crimestatssa.com/ (accessed 15 November 2016). [ Links ]
15. Waring WP III, Biering-Sorensen F, Burns S, et al. Review and revisions of the international standards for the neurological classification of spinal cord injury. J Spinal Cord Med 2010;33(4):346-352. https://doi.org/10.1080/10790268.2010.11689712 [ Links ]
16. Matzopoulos R, Thompson ML, Myers JE. Firearm and nonfirearm homicide in 5 South African cities: A retrospective population-based study. Am J Public Health 2014;104(3):455-460. https://doi.org/10.2105/AJPH.2013.310650 [ Links ]
17. McKenzie K. Domestic Gun Control Policy in Ten SADC Countries. GFSA. In: Gamba, V. Society Under Siege: Managing Arms in South Africa. Pretoria: Institute for Security Studies, 2000. [ Links ]
18. Jaiswal M, Mittal RS. Concept of gunshot wound spine. Asian Spine J 2013;7(4):359-364. https://doi.org/10.4184/asj.2013.7.4.359 [ Links ]
19. Joseph C, Nilsson Wikmar L. Prevalence of secondary medical complications and risk factors for pressure ulcers after traumatic spinal cord injury during acute care in South Africa. Spinal Cord 2016;54(7):535-539. https://doi.org/10.1038/sc.2015.189 [ Links ]
20. Chopra T, Marchaim D, Awali RA, et al. Risk factors and acute in-hospital costs for infected pressure ulcers among gunshot-spinal cord injury victims in southeastern Michigan. Am J Inf Contr 2016;44(3):315-319. https://doi.org/10.1016/j.ajic.2015.10.002 [ Links ]
21. Gélis A, Dupeyron A, Legros P, Benaïm C, Pelissier J, Fattal C. Pressure ulcer risk factors in persons with SCI: Part I: Acute and rehabilitation stages. Spinal Cord 2009;47(2):99-107. https://doi.org/10.1038/sc.2008.107 [ Links ]
22. Byrne DW, Salzberg CA. Major risk factors for pressure ulcers in the spinal cord disabled: A literature review. Spinal Cord 1996;34(5):255-263. https://doi.org/10.1038/sc.1996.46 [ Links ]
23. Verschueren JHM, Post MWM, de Groot S, van der Woude LHV, van Asbeck FWA, Rol M. Occurrence and predictors of pressure ulcers during primary in-patient spinal cord injury rehabilitation. Spinal Cord 2011;49(1):106-112. https://doi.org/10.1038/sc.2010.66 [ Links ]
24. Jackson AB, Groomes TE. Incidence of respiratory complications following spinal cord injury. Arch Phys Med Rehabil 1994;75(3):270-275. [ Links ]
25. Jensen MP, Chodroff MJ, Dworkin RH. The impact of neuropathic pain on health-related quality of life: Review and implications. Neurology 2007;68(15):1178-1182. https://doi.org/10.1212/01.wnl.0000259085.61898.9e [ Links ]
26. Sindrup SH, Otto M, Finnerup NB, Jensen TS. Antidepressants in the treatment of neuropathic pain. Basic Clin Pharmacol Toxicol 2005;96(6):399-409. https://doi.org/10.1111/j.1742-7843.2005.pto_96696601.x [ Links ]
27. Guy S, Mehta S, Leff L, Teasell R, Loh E. Anticonvulsant medication use for the management of pain following spinal cord injury: Systematic review and effectiveness analysis. Spinal Cord 2014;52(2):89-96. https://doi.org/10.1038/sc.2013.146 [ Links ]
 Correspondence:
Correspondence:
C Joseph
cjoseph@uwc.ac.za, conran.joseph@gmail.com
Accepted 7 February 2017














