Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.107 no.5 Pretoria Mai. 2017
http://dx.doi.org/10.7196/samj.2017.v107i5.12192
RESEARCH
Predicting postoperative haemoglobin changes after burn surgery
P SlabberI; Z FarinaII; N AllortoIII; R N RodsethIV, V
IMB ChB, DA (SA), FCA (SA); Department of Anaesthetics, Grey's Hospital, Pietermaritzburg, South Africa
IIMB ChB, FCA (SA); Peri-operative Research Group, Metropolitan Department of Anaesthetics, Critical Care and Pain Management, College of Health Sciences, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Pietermaritzburg, South Africa
IIIMB ChB, FCS (SA), MMed; Peri-operative Research Group, Metropolitan Department of Anaesthetics, Critical Care and Pain Management, College of Health Sciences, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Pietermaritzburg, South Africa
IVMB ChB, DA (SA), FCA (SA), MMed, MSc, Cert Crit Care, PhD Peri-operative Research Group, Metropolitan Department of Anaesthetics, Critical Care and Pain Management, College of Health Sciences, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Pietermaritzburg, South Africa
VDepartment of Outcomes Research, Cleveland Clinic, Cleveland, OH, USA
ABSTRACT
BACKGROUND. Burn surgery is associated with significant blood loss and fluid shifts that cause rapid haemoglobin (Hb) changes during and after surgery. Understanding the relationship between intraoperative and postoperative (day 1) Hb changes may assist in avoiding postoperative anaemia and unnecessary peri-operative blood transfusion.
OBJECTIVE. To describe the Hb changes into the first day after burn surgery and to identify factors predictive of Hb changes that would guide blood transfusion decisions.
METHODS. This was a single-institution, retrospective cohort study that included 158 patients who had undergone burn surgery. Hb was measured at the start and end of surgery, and on the first day (16 - 32 hours) after surgery, and the results were analysed. Peri-operative factors (Hb at the end of surgery, total body surface area operated on (TBSA-op), fluid administration and intraoperative blood administration) were evaluated to determine their association with Hb changes on the first day after surgery.
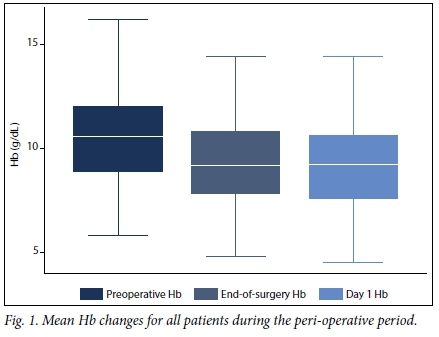
RESULTS. The mean (standard deviation) preoperative Hb was 10.6 (2.29) g/dL, the mean postoperative Hb was 9.4 (2.01) g/dL, and the mean Hb on the first day after surgery was 9.2 (2.19) g/dL. Median total burn surface area was 7% (interquartile range 9%, min. 1%, max. 45%), with a mean body surface area operated on (debridement area plus donor area) of 9.7%. Of the 158 patients, 26 (16%) had an Hb <7 g/dL (transfusion trigger) on the first day after surgery. For patients with a high (> 9 g/dL), intermediate (> 7 - <9 g/dL), or low (<7 g/dL) Hb measurement at the end of burn surgery, those with an Hb below the transfusion trigger on the first day after burn surgery were 0%, 27%, and 75%, respectively. End-of-surgery Hb and TBSA-op strongly predicted the first day Hb level. In the intermediate group, 55% of patients with a TBSA-op >11% had an Hb below the transfusion trigger on the first day after surgery.
CONCLUSION. Hb at the end of burn surgery was the best predictor of Hb on the first day after surgery. Patients with an Hb <7 g/dL remained as such on the first postoperative day. Half of the patients with an end-of-surgery Hb > 7 - <9 g/dL and who had >11% TBSA-op had an Hb <7 g/dL on the first postoperative day.
Burn surgery is associated with significant peri-operative haemoglobin (Hb) changes. During surgery, blood loss mainly occurs owing to wound debridement and skin harvesting. However, administration of clear fluid, required to maintain intravascular volume status during anaesthesia and surgery, leads to haemodilution and further lowers Hb at the end of surgery. It has become common practice to use an Hb trigger of 7 g/dL to initiate blood transfusion in surgical patients.[1,2] However, it is not clear how this trigger should be applied in burn surgery.[3,4] At the conclusion of burn surgery, it is common to be faced with a patient who has an Hb close to the transfusion threshold of 7 g/dL. Will the patient continue to lose blood from their wounds and so require a transfusion, or will the patient excrete excess intraoperative fluid, haemoconcentrate their blood, and consequently avoid the need for a transfusion? The ability to predict Hb on the first day after surgery may assist in avoiding severe postoperative anaemia and unnecessary peri-operative blood transfusion.
Methods
Study design and objectives
We conducted a retrospective single-institution cohort study at the burn service, Edendale Hospital, a regional-level hospital in Pieter-maritzburg, South Africa, between October 2014 and January 2016.
The burn service has eight beds and admits both adults and children, but also utilises general surgery beds to accommodate additional patients. [5] Contemporary burn management principles, which include attempted early excision and grafting, are followed, and the service makes use of nanocrystalline silver and hydrofibre dressings. Limitations in theatre, and blood and intensive care unit bed availability pose logistical difficulties that limit the full application of staged excision and grafting.[5]
The study was conducted after receiving approval from the Biomedical Research Ethics Committee of the University of KwaZulu-Natal (ref. no. BE 393/16), Edendale Hospital Management, and the KwaZulu-Natal Department of Health.
The primary study objective was to describe the Hb changes over the first 24 hours after completion of surgery. Three Hb measurements (at the start of surgery, at the end of surgery, and on the first day (within 16 - 32 hours) after surgery) were obtained. One anaesthetist (PS) collected all the samples, all of which were measured on the HemoCue Hb 201+ System (HemoCue, Sweden) point-of-care haemoglobinometer.
The secondary study objective was to determine if there were perioperative factors predictive of an Hb <7 g/dL on the first day after surgery, which were indicative of the need for a blood transfusion at the end of surgery. An association between the Hb level at the end of surgery, total body surface area operated on (TBSA-op), fluid administration in both the intraoperative and postoperative period, and administration of blood intraoperatively, with an Hb <7 g/dL on the first day after surgery, was sought.
Eligibility criteria and data collection
All patients who underwent burn surgery during the 16-month study period were included, where all data points were available from the burns database and patient records. Clinical data points that were required, in addition to the three Hb measurements, were weight, age, total burn surface area, debridement area, donor area, graft area, volume of intraoperative blood transfusion, and volume of intraoperative and postoperative clear fluids. Any patient who received a blood transfusion after the end of surgery, but prior to the measurement of Hb on the first postoperative day, was excluded from the study. All patients were haemodynamically stable at the end of surgery and anaesthesia.
No changes in time to burn wound excision and grafting or operative technique were implemented during the study period. Haemostasis during burn surgery is typically attained with a combination of adrenaline-soaked gauze compression, electrocautery and sutures. An intraoperative transfusion threshold of 7 g/dL was used, but this was implemented at the discretion of the primary burn surgeon and anaesthetist.
Statistical analysis
The baseline characteristics of the included patients are reported as mean (standard deviation (SD)) for continuous normally distributed variables; median and range or interquartile range (IQR) for data not normally distributed; and count (percent) for categorical variables. We reported the mean reduction or increase in postoperative Hb together with SD and 95% confidence intervals (CIs).
We identified the number of patients who had an Hb <7 g/dL on the first day after surgery, who would therefore have required transfusion. In a multivariable logistic regression model we evaluated Hb at the end of surgery, TBSA-op (debridement area plus donor area), intraoperative fluid infused (mL/kg) and intraoperative blood transfusion (mL/kg). We empirically stratified patients into three groups, based on their end-of-operation Hb: low (<7 g/dL), intermediate (7 - <9 g/dL), and high (>9 g/dL). Patients were then substratified according to the remaining significant variables. Cut-point estimations were determined using the method described by Liu.[6]
Comparisons between normally distributed data were done using Student's f-test; for data not normally distributed we used the Wil-coxon Mann-Whitney (7-test. Categorical data were analysed using the χ2 test. The Shapiro-Wilk test was used for normality testing. For all analyses, p<0.05 defined statistical significance.
Results
Patient characteristics
Within the specified time frame, we identified 158 patients with complete data sets. These included 68 children with a mean (SD) age of 3.3 (3.0) years (range 1 month - 14 years); and 90 adults with a mean age of 35.0 (14.1) (18 - 83) years. At each operation the median TBSA for the group was 7% (IQR 9%, min. 1%, max. 45%); the mean burn area being debrided was 4% (IQR 5%, min. 0%, max. 33%); the mean skin donor area was 3% (IQR 4%, min. 0%, max. 20%); and the mean skin graft area was 3% (IQR 4%, min. 0%, max. 28%). The mean TBSA-op was 9.7% (9.0% in children and 10.2% in adults). A total of 20 (12.7%) patients received an intraoperative transfusion, with a mean volume of 9.8 mL/kg of blood.
Peri-operative Hb changes into the first day after surgery
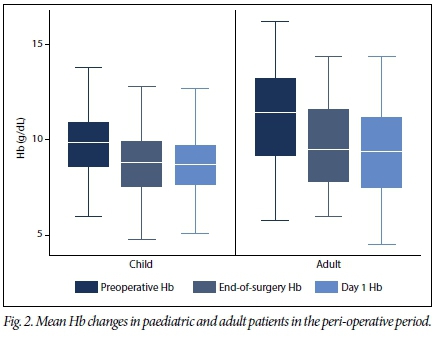
The mean preoperative Hb was 10.6 (2.29) g/dL, with a higher mean in the adult compared with the paediatric population (11.3 (2.43) g/dL v. 9.7 (1.74) g/dL; p<0.001)). The mean Hb at the end of surgery was 9.4 (2.01) g/dL, with a higher mean in the adult population (9.8 (2.2) g/dL v. 8.7 (1.58) g/dL; p<0.001). The mean Hb on the first day after surgery was 9.2 (2.19) g/dL, with a higher mean in the adult population (9.4 (2.43) g/dL v. 8.9 (1.79) g/dL; p < 0.001) (Figs 1 and 2).
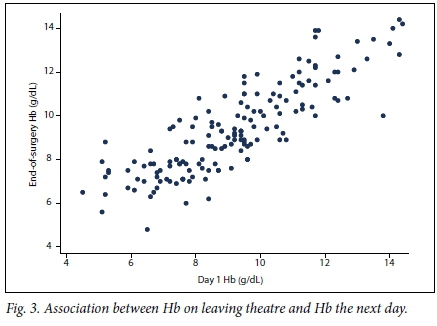
Of the 158 patients, 26 (16.5%) had a low Hb reading (<7 g/dL) on the first day after surgery (9 paediatric and 17 adult patients, p=0.392). Of these 26 patients, 17 (65%) had an Hb of >7 g/dL at the end of surgery, while 9 (35%) had an Hb of <7 g/dL at the end of surgery. In a logistic regression model, Hb at the end of surgery (odds ratio (OR) 0.19, p<0.001; 95% CI 0.087 - 0.418) and TBSA-op (OR 1.09, p=0.07; 95% CI 1.01 - 1.18) were predictive of an Hb <7 g/dL on the first day after surgery. Fig. 3 demonstrates the association between Hb at the end of surgery and Hb on the first postoperative day.
In patients with a low Hb at the end of surgery, 75% («=9/12) had an Hb <7 g/dL on the first day after surgery (Table 1). By contrast, no patient in whom surgery had been completed, with a high Hb (>9 g/dL; n=83), had an Hb <7 g/dL on the first day after surgery. In the intermediate Hb group (>7 g/dL, but <9 g/dL), 27% («=17/63) were below the transfusion trigger. The optimal cut-point for the prediction of transfusion on the first day after surgery was an end-of-surgery Hb of 7.15 g/dL.
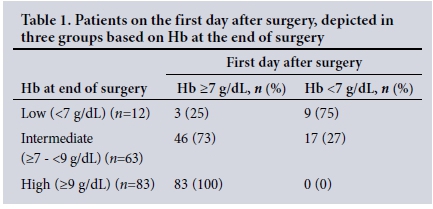
Within the intermediate Hb group, a TBSA-op of 11% best identified patients at risk of having an Hb <7 g/dL on the first day after surgery. When the TBSA-op was >11%, 55% (n=12/22) of patients required transfusion compared with 12% (n=5/41), when the TBSA- op was <11%.
Discussion
To our knowledge, this is the first study to describe the natural variation in Hb from the end of surgery through into the first day after burn surgery. Our study revealed a minor reduction in mean Hb from the end of surgery compared with the measurements performed 16 - 32 hours after completion of surgery. We further identified patients with an end-of-surgery Hb >7 g/dL but <9 g/dL, with a TBSA-op of >11%, to be at high risk of an Hb <7 g/dL on the first day after surgery.
Current blood transfusion strategies aim to minimise unnecessary peri-operative blood transfusions.[7] The global acceptance of a restrictive approach to blood transfusion has led to its adoption in most burn surgery units.[4] The association between the number of units of blood transfused and increased morbidity, especially infectious complications, is of concern in the burn population.'81 Therefore, given the associated risks and cost, it is crucial that every unnecessary blood transfusion be avoided.
There is a need to avoid under-transfusion, which may lead to severe anaemia on the first day after burn surgery and may compromise skin graft viability. Although this has never been directly studied, the absence of increased complication rates in burn units that use a transfusion threshold of 7.0 g/dL, suggests that tissue oxygen delivery is adequate with this threshold and does not affect skin graft failure rate or infectious complications.[1,4,8] The risk inherent in cases of severe anaemia (Hb <7g/dL) at the end of burn surgery is the possibility of haemodynamic instability in the early postoperative period. In addition, poor healing from suboptimal tissue oxygenation in patients who are often in pain and hypermetabolic (with increased oxygen extraction) from the surgical stress response, may increase the graft failure rate.
Because of the nature of burn surgery and its anaesthetic and resuscitative requirements, dramatic changes in Hb levels during the intra- and postoperative periods are common. Anaesthetists often assume that the Hb will slowly increase, secondary to the excretion of excess intraoperative clear fluid, once the acute surgical phase is over and bleeding has stopped. However, as we have demonstrated, it would seem that, instead of an increase, there is a continuous slow Hb reduction on the first day after surgery. The anaemia of critical illness in burn patients describes a continuous slow decrease in Hb in the first days after surgery.[9] It is therefore possible that the postoperative Hb nadir may only be reached a few days after burn surgery for patients not transfused in the postoperative period. Good clinical judgement, taking into consideration the risk associated with unnecessary blood transfusion compared with that of under-transfusion, is required with these patients.
There is a clear relationship between Hb at the end of surgery and Hb on the first day after surgery, and an inverse relationship between TBSA-op and Hb on the first postoperative day. These two factors, end-of-surgery Hb and TBSA-op, must therefore be kept in mind when making transfusion decisions. An Hb closer to 7.0 g/dL at the end of surgery and/or a TBSA-op >10.9% will increase the possibility of having an Hb <7 g/dL on the first day after surgery and therefore the need for a blood transfusion.
This study is limited because of its retrospective nature, singleinstitution design and small sample size. Because of a lack of resources, surgeons at the Edendale burn service generally operate on smaller body surface areas and therefore the study population is not representative of major burn institutions in the developed world. The larger body surface area operated on in developed institutions is associated with increased peri-operative blood and fluid administration, leading to complex fluid shifts and Hb variations not seen in our setting. Furthermore, the postoperative inflammatory response from major burn surgery affects haemostasis and results in ineffective haematopoiesis, all of which have an impact on Hb changes.'71 Moreover, this study has not considered depth and location of burn wounds, surgical experience and technique, presence of infected wounds, and time from burn injury to surgery. However, the factors that were included in the regression model represent the most commonly collected and clinically significant factors. This dramatically increases the utility of these findings and it is likely that these results may simplify peri-operative blood transfusion decision-making and could guide future transfusion-related studies.
Conclusion
In this study, end-of-burn surgery Hb was the best predictor of Hb on the first day after surgery. Patients with an Hb <7 g/dL remained below that level on the first day after surgery. Half of the patients with an end-of-surgery Hb >7 - <9 g/dL and >11% TBSA-op had an Hb <7 g/dL on the first postoperative day.
Acknowledgements. None.
Author contributions. PS, ZF, NA and RNR designed the study; PS and NA collected the data; PS and RNR analysed the data; and PS, ZF, NA and RNR were responsible for drafting the manuscript.
Funding. None.
Conflicts of interest. None.
References
1. Kwan P, Gomez M, Cartotto R. Safe and successful restriction of transfusion in burn patients. J Burn Care Res 2006;27(6):826-834. https://doi.org/10.1097/01.BCR.0000245494.45125.3E [ Links ]
2. Carson JL, Stanworth SJ, Roubinian N, et al. Transfusion thresholds and other strategies for guiding allogeneic red blood cell transfusion. Cochrane Database Syst Rev 2016;(10):CD002042. https://doi.org/10.1002/14651858.cd002042.pub3 [ Links ]
3. Hovaguimian F, Myles PS. Restrictive versus liberal transfusion strategy in the perioperative and acute care settings: A context-specific systematic review and meta-analysis of randomized controlled trials. Anesthesiology 2016;125(1):46-61. https://doi.org/10.1097/aln.0000000000001162 [ Links ]
4. Palmieri TL, Lee T, O'Mara MS, Greenhalgh DG. Effects of a restrictive blood transfusion policy on outcomes in children with burn injury. J Burn Care Res 2007;28(1):65-70. https://doi.org/10.1097/01253092-200603001-00120 [ Links ]
5. Allorto NL, Clarke DL. Merits and challenges in the development of a dedicated burn service at a regional hospital in South Africa. Burns 2015;41(3):454-461. https://doi.org/10.1016/j.burns.2014.07.021 [ Links ]
6. Liu X. Classification accuracy and cut point selection. Stat Med 2012;31(23):2676-2686. https://doi.org/10.1002/sim.4509 [ Links ]
7. Posluszny JA, Jr, Gamelli RL. Anemia of thermal injury: Combined acute blood loss anemia and anemia of critical illness. J Burn Care Res 2010;31(2):229-242. https://doi.org/10.1097/bcr.0b013e3181d0f618 [ Links ]
8. Palmieri TL, Caruso DM, Foster KN, et al. Effect of blood transfusion on outcome after major burn injury: A multicenter study. Crit Care Med 2006;34(6):1602-1607. https://doi.org/10.1097/01.ccm.0000217472.97524.0e [ Links ]
9. Posluszny JA, Jr, Conrad P, Halerz M, Shankar R, Gamelli RL. Classifying transfusions related to the anemia of critical illness in burn patients. J Trauma 2011;71(1):26-31. https://doi.org/10.1097/ta.0b013e3181f2d9ed [ Links ]
 Correspondence:
Correspondence:
P Slabber
sknoetze@yahoo.com
Accepted 11 January 2017














