Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.107 n.3 Pretoria Mar. 2017
http://dx.doi.org/10.7196/samj.2017.v107i3.11206
RESEARCH
The prevalence of HIV seropositivity and associated cytopenias in full blood counts processed at an academic laboratory in Soweto, South Africa
J L VaughanI; T M WiggillII; N AlliIII; K HodkinsonIV
IMB BCh, FC Path (SA) (Haem), MMed (Haem); Department of Molecular Medicine and Haematology, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg; and National Health Laboratory Service, Johannesburg, South Africa
IIMB BCh, MMed (Haem); Department of Molecular Medicine and Haematology, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg; and National Health Laboratory Service, Johannesburg, South Africa
IIIMB BCh, FC Path (SA) (Haem); Department of Molecular Medicine and Haematology, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg; and National Health Laboratory Service, Johannesburg, South Africa
IVMB BCh; Department of Molecular Medicine and Haematology, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg; and National Health Laboratory Service, Johannesburg, South Africa
ABSTRACT
BACKGROUND. The HIV epidemic in South Africa (SA) has had a substantial impact on laboratory services, at least partially owing to the well-described propensity to cytopenias in HIV-positive patients.
OBJECTIVES. (i) To formally gauge the impact of HIV infection on the state sector haematology services in SA by determining the HIV seropositivity rate among full blood counts (FBCs) performed at a large academic state sector laboratory; and (ii) to document the prevalence of cytopenias among HIV-positive patients in this setting.
METHODS. Randomly selected FBCs submitted to the National Health Laboratory Service laboratory at Chris Hani Baragwanath Academic Hospital, Johannesburg, were extracted from the laboratory information system (LIS) and retrospectively reviewed. HIV test results and other pertinent information in the LIS were documented, as was the presence of any cytopenias.
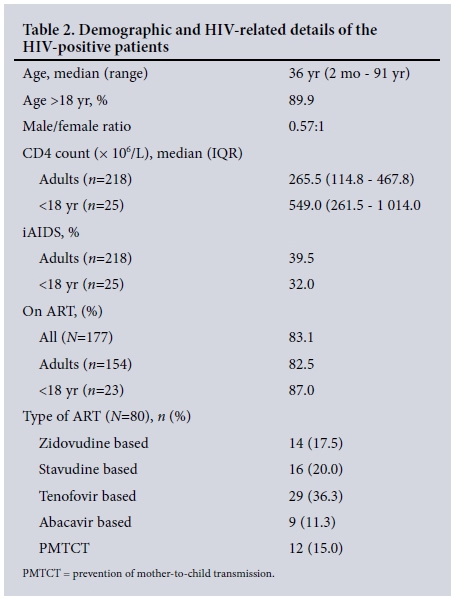
RESULTS. HIV status was documented in 561 of 1 006 samples (55.8%), with 307 (54.7%) of these being HIV-positive. Of the HIV-positive patients, 63.2% had one or more cytopenia/s. Anaemia was present in 183/307 (59.6%) of the HIV-positive patients, and was severe (haemoglobin <8 g/dL) in 32/307 (10.4%). Multivariate linear regression analysis showed significant independent associations between the presence of anaemia and both immunological AIDS (iAIDS) (p<0.0001) and male sex (p<0.025), but not HIV viral load (VL) (p=0.33) or antiretroviral therapy (ART) exposure (p=0.70). Thrombocytopenia and neutropenia were present in 37/307 (12.1%) and 11/51 (21.6%) of the HIV-positive patients, respectively, with no statistically significant association between either of these cytopenias and iAIDS, exposure to ART or VL.
CONCLUSIONS. The findings reflect the substantial impact of the HIV epidemic on state sector laboratory resources, particularly the haematology service.
The HIV epidemic in South Africa (SA) has had a substantial impact on healthcare services, particularly in the public sector. This is also true for the laboratory services owing to the increased burden of pathology in the community and the demand for therapy monitoring. The impact on haematology services is singularly notable because of the numerous haematological complications of HIV infection, which occur secondary to effects of the virus itself, as a result of associated opportunistic infections/malignancies, or as adverse drug effects.[1] Several studies have reported the prevalence of haematological complications in HIV-seropositive patients,[2-7] with variables such as disease stage and exposure to antiretroviral therapy (ART) being important determinants.[8] However, there is a paucity of published SA data in this regard, despite the fact that the burden of HIV infection in SA is among the highest in the world.[9] Documenting the SA experience in this respect is important, as the prevalence of some cytopenias has been shown to vary geographically, with anaemia being more prevalent among treatment-naive patients with AIDS from Africa than among those from Asia or the Americas.[5] Furthermore, geographical differences have been reported within Africa, with the prevalence of anaemia in patients with immunological AIDS (iAIDS) being 32.2%, 49.3% and 58.0% in Rwanda,[6] Uganda[7] and Nigeria,[4] respectively. The prevalence of cytopenias in SA patients is therefore of interest.
Objectives
(i) To document the prevalence of cytopenias in full blood counts (FBCs) from HIV-positive patients in a large academic state sector laboratory serving a community with a high HIV prevalence; and
(ii) to indirectly gauge the impact of the HIV epidemic on the state sector haematology laboratory services by determining the HIV seropositivity rate among samples submitted for an FBC. Because the FBC is the most commonly performed test in the haematology laboratory, the seropositivity rate among samples submitted for an FBC serves as a surrogate marker of the overall burden of HIV infection on the haematology services.
Methods
FBCs submitted to the National Health Laboratory Service (NHLS) laboratory at Chris Hani Baragwanath Academic Hospital (CHBAH), Soweto, Johannesburg, on 7 non-consecutive days throughout 2012 were extracted from the laboratory information system (LIS) (DisaLab version 04.16.04.373; Laboratory System Technologies, SA) and retrospectively reviewed. To ensure that the data were representative of all sites serviced by the laboratory, the 7 days sampled included every day of the week, and to avoid temporal bias with regard to cytopenia prevalence (as a result of seasonal diseases affecting blood counts), every season of the year was represented. All the FBCs performed on each randomly selected day were extracted, pooled and then listed randomly through sorting the samples alphabetically by the first letter of the patient's name. This yielded 4 456 FBCs, of which the first 1 020 were sampled for analysis. The LIS repository for the included samples was then reviewed for relevant HIV test results where available, and the presence of any cytopenia/s was recorded. The samples included specimens collected from inpatient, outpatient and casualty facilities at CHBAH, as well as primary healthcare (PHC) clinics in Soweto. Anaemia in adults was defined as a haemoglobin (Hb) concentration <14 g/dL in males and <12 g/dL in females. For children, anaemia was defined as an Hb concentration below the age-specific reference ranges. Moderate and severe anaemia were defined as an Hb concentration <10 g/dL and <8 g/dL, respectively, for all age groups. Thrombocytopenia was defined as a platelet count <150 χ 109/L, neutropenia as an absolute neutrophil count <2 χ 109/L and lymphopenia as a lymphocyte count below the age-specific reference range. The mean cell volume (MCV) was classified as low, normal or high based on age-specific laboratory reference ranges. Other information recorded from the LIS (where available) included demographic details, recent CD4 counts and HIV viral loads (VLs), as well as information pertaining to ART exposure. iAIDS was defined as a CD4 count <200 cells^L in adults, and as a CD4 count <200 cells^L or a CD4 percentage <15% in children aged >5 years, <15% in children aged 36 - 59 months, <20% in children aged 12 - 35 months and <25% in children aged <11 months. The study was approved by the Human Research Ethics Committee of the University of the Witwatersrand, Johannesburg (ref. no. M131025).
Statistical analysis
Statistical analysis was performed using Statistica software, version 12.0 (StatSoft, USA). Continuous data are presented as medians with interquartile ranges (IQRs) and categorical data as frequencies and percentages. The Mann-Whitney U-test was used to compare variables of interest. Multivariate linear regression analysis was performed to assess the relationship between anaemia, thrombocytopenia and neutropenia and various variables of interest. Where continuous data were not normally distributed, variables were log-transformed before regression analysis. For patients with an undetectable VL, the low detection limit was used for the purposes of statistical analysis. The reported adjusted beta coefficients are the antilog values of the calculated coefficients. Residual analysis was performed on all statistically significant results, and any data point with a standard residual of >2.5 was excluded from analysis. Blood counts in patients treated with different antiretroviral agents were compared by Kruskal-Wallis one-way analysis of variance followed by post hoc multiple comparisons of the mean rank scores between pairs of groups with a Bonferroni adjustment. Statistical significance was accepted at a p-value of <0.05.
Results
HIV prevalence
A total of 1 020 FBCs were extracted from the laboratory database, 14 of which were excluded from further analysis because they were repeat specimens collected on the same day. Of the remaining 1 006 samples, 212 (21.7%) were collected at PHC clinics around Soweto, 543 (54.0%) from the casualty department, wards or intensive care units (ICUs) of CHBAH, and the remainder (25.0%) from the hospital outpatient departments. HIV status was documented in 561 patients (55.8%), of whom 307 (54.7%) were HIV-positive. Test results were most frequently available for patients seen in medical wards, the haematology/oncology departments and outpatient/PHC facilities (the latter probably owing to the large proportion of samples received from these sites for the purposes of ART monitoring) (Table 1). Close to one-third of the HIV-positive patients were inpatients, the greatest proportion of whom were admitted to medical wards (46.9%), while <10% were admitted to ICUs, obstetrics/gynaecology wards and paediatric wards. Within the major hospital disciplines, the HIV seropositivity rate was highest in the medical wards (close to 60%), lowest in the paediatric units (<20%), and ~28 - 40% in the other departments assessed (Table 1). Pertinent demographic and HIV-related details of the HIV-positive patients are summarised in Table 2.
Cytopenia prevalences
Cytopenia/s were present in 194/307 (63.2%) of the patients. An isolated cytopenia was present in 157/194 (80.9%), while 32/194 (16.5%) and 5/194 (2.6%) had bi- and pancytopenia, respectively. A significantly larger proportion of patients with one or more cytopenia/s had iAIDS compared with those without any cytopenia (52.7% (77/146) v. 17.5% (17/97); p<0.0001). In contrast, the proportions of patients on ART did not differ significantly between those with and without cytopenias (79.0% (79/100) v. 88.3% (68/77); p=0.1). Cytopenias were significantly more common among inpatients (p<0.0001), with >90% of inpatients having one or more cytopenia/s as opposed to <50% of outpatients (Table 1).
Anaemia analysis
Among the HIV-positive patients, 183/307 (59.6%) had anaemia (median Hb 11.6 g/dL), which was severe in 32/307 (10.4%). Anaemia was significantly more common in HIV-positive adult males than in HIV-positive adult females (p=0.047), being present in 70/99 males (70.7%) v. 101/176 females (57.4%) (median Hb 12.3 g/dL (IQR 8.80 -14.33) v. 11.5 g/dL (IQR 9.63 - 12.68), respectively). Among HIV-positive adults, the CD4 count was significantly lower in individuals with anaemia than in those with normal Hb concentrations (median CD4 count 159 cellsμL v. 400 cells μL, respectively; p<0.0001), but did not differ between HIV-positive adult males and females with anaemia (median CD4 count 164 cells μL v. 177 cellsμL, respectively; p=0.785). Among the HIV-positive children and adolescents, only 12/31 (38.7%) had anaemia (median Hb 11.3 g/dL).
Both anaemia and severe anaemia were significantly more prevalent among inpatients than outpatients (p<0.0001), with a particularly high rate of severe anaemia among the HIV-positive patients admitted to medical wards (35.6%). Further information regarding the prevalence of anaemia among HIV-positive patient subgroups is summarised in Table 3.
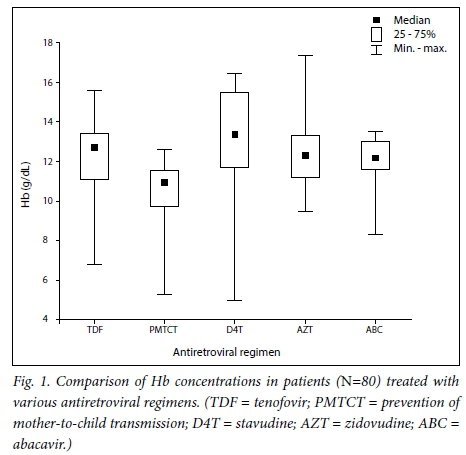
Multivariate linear regression analysis showed significant independent associations between the presence of anaemia and both iAIDS (adjusted beta coefficient 0.41; standard error (SE) 0.10; p<0.0001) and male sex (adjusted beta coefficient 0.196; SE 0.09; p<0.025), while no significant relationship was found between anaemia and exposure to ART (p=0.70), VL (p=0.33) or age (p=0.14). Severe anaemia was significantly inversely related to exposure to ART on multivariate linear regression analysis (adjusted beta coefficient -0.32; SE 0.15; p=0.035), but was not associated with the presence of iAIDS (p=0.16), sex (p=0.68), age (p=0.97) or VL (p=0.66). A Bonferroni-adjusted Kruskal-Wallis analysis showed no significant difference in the Hb concentration between patients treated with the various antiretroviral regimens (Fig. 1).
The median MCV was 91.1 fL (IQR 83.2 - 98.3), and the MCV was low, normal and high in 36/307 (11.7%), 198/307 (64.5%) and 70/307 (22.8%), respectively, of the HIV-positive patients. Of the patients with macrocytosis, normocytosis and microcytosis, 28/70 (40.0%), 43/198 21.7%) and 33/36 (91.7%), respectively, had anaemia. The median MCV and the prevalence of microcytic anaemia did not differ statistically between males and females (median MCV 90.7 fL v. 91.2 fL; p=0.94 and microcytic anaemia prevalence 12.5% v. 9.4%; p=0.85).
Thrombocytopenia analysis
Among the HIV-positive patients, the median platelet count was 254 χ 109/L (IQR 204 - 324). Thrombocytopenia was present in 37/307 (12.1%), with 20 (54.5%) of these having a platelet count <100 χ 109/L. Thrombocytopenia was uncommon in outpatients but present in close to 30% of inpa-tients, with a particularly high prevalence in patients admitted to medical wards (37.8%) (Table 1). Further information regarding the prevalence of thrombocytopenia among HIV-positive patient subgroups is summarised in Table 3. Multivariate linear regression analysis showed marginally significant independent associations between the presence of thrombocytopenia and both iAIDS (p=0.09) and exposure to ART (p=0.07), while no significant relationship was found between thrombocytopenia and VL (p=0.81). A Bon-ferroni-adjusted Kruskal-Wallis analysis showed no significant difference in the platelet count between patients treated with the various antiretroviral regimens.
Leucocyte subset analysis
A differential white cell count was requested in 51/307 HIV-positive patients (16.6%), with median neutrophil, lymphocyte and monocyte counts of 3.42 χ 109/L (IQR 2.23 -6.43), 1.34 χ 109/L (IQR 0.67 - 2.08) and 0.49 χ 109/L (IQR 0.22 - 0.80), respectively. Neutropenia was present in 11/51 patients (21.6%), with 6/51 (11.8%) and 4/51 (7.8%) having neutrophil counts <1.5 χ 109/L and <1 χ 109/L, respectively. Lymphopenia was present in 18/51 patients (35.3%). Further information regarding the prevalences of neutropenia and lymphopenia in HIV-positive patient subgroups is summarised in Table 3. On multivariate regression analysis, no significant relationship was evident between neutropenia and VL (p=0.23), ART exposure (p=0.15) or the presence of iAIDS (p=0.22), and a Bonferroni-adjusted Kruskal-Wallis analysis showed no significant differences in the neutrophil count between patients treated with the various antiretroviral regimens.
Discussion
In this study conducted at the NHLS laboratory at CHBAH, 307 (30.5%) of the 1 006 patients included were documented to be HIV-positive, of whom 63.2% had one or more cytopenia/s. These were significantly more common among individuals who were inpatients or had iAIDS, but also occurred in close to 50% of outpatients and in >50% of those on ART. Anaemia was the most prevalent blood count derangement, being present in ~60% of all patients, ~70% of ART-naive patients and ~80% of patients with iAIDS. The prevalence in ART-naive patients was generally substantially higher than prevalences documented in previous studies from other parts of Africa, which ranged from ~20% to 50%.[6,7] With regard to other studies conducted among South Africans, the prevalence of anaemia among ART-naive patients was similar to that reported by Kerkhoff et al.,[10] (~70%), but higher than that documented by Takuva et al.[11]and Firnhaber et al.,[5] who both reported anaemia (Hb <10 g/dL) in ~20 - 25% of patients (as opposed to ~40% with Hb concentrations in this range in our study). The generally higher anaemia prevalence observed in this study compared with the majority of other African cohorts may be attributable to the fact that many of the previous studies in this field were performed in patients who were either enrolled in clinical trials or seen at outpatient ART clinics. In contrast, our study included patients hospitalised with HIV-related complications, among whom the prevalence of cytopenia/s would be expected to be higher than in more clinically stable patients. Nonetheless, the findings are of concern given the well-documented adverse prognosis associated with anaemia in HIV-positive patients.[2,12]
Multivariate regression analysis confirmed significant independent associations between anaemia and both male sex and iAIDS. Interestingly, these variables were not independently associated with severe anaemia, while a significant inverse relationship between the presence of severe anaemia and ART exposure was noted. This suggests that ART is protective against severe anaemia, regardless of immune status. Also of note was that the prevalence of anaemia was substantially lower in patients aged <18 years than in older patients, which may be due to the somewhat lower prevalence of iAIDS in these patients. Although certain antiretroviral agents (particularly zidovudine) are reported to be associated with an increased risk of anaemia, the Hb level did not appear to be affected by the ART regimens used in this study. However, this finding should be treated with reserve, as the duration of ART exposure has not been taken into account, and the fairly limited data available about type of ART exposure may compromise the accuracy of these results.
Anaemia was microcytic in 18.0% of the HIV-positive patients and in 21.4% of the ART-naive patients with iAIDS. This is substantially lower than figures reported by Firnhaber et al[5]in a study that compared the prevalence of various cytopenias in ART-naive patients from Africa, Asia and the Americas, where anaemia was found to be microcytic in 50% of cases.[5] Furthermore, in contrast to other studies, we found no significant difference in the MCV between males and females,[3] no difference in the prevalence of microcytic anaemia according to sex,[2] and a higher prevalence of anaemia in males than in females.[5,9] Collectively, these findings suggest that iron deficiency (the commonest cause of microcytic anaemia, and the form to which females are particularly predisposed) is not as highly prevalent in this population of patients as in other developing countries. Further investigation in this regard would be of interest.
Thrombocytopenia and neutropenia were present in 12.1% and 21.6% of patients, respectively, with a platelet count <100 χ 109/L in 6.5% and a neutrophil count <1 χ 109/L in 7.8%. These prevalences are somewhat higher than those reported elsewhere,[3-6] probably for the same reasons cited for the differences in the prevalence of anaemia. Thrombocytopenia was marginally associated with the presence of iAIDS and exposure to ART, while no significant association was evident between any HIV-related parameters and neutropenia.
HIV status was documented in close to 50% of the samples, with the highest rates of documentation in patients admitted to the medical wards and haematology/oncology units. In contrast, documentation rates were <50% in the other departments assessed, which may be due to point-of-care screening in some instances, or known results from testing at other sites. Nonetheless, these findings raise concern about the possibility that patients are generally only tested when they present with pathology that may be attributable to HIV infection. In the context of a community with a high HIV prevalence, failure to systematically screen all patients presenting to healthcare facilities (including those without HIV-related pathology) would appear to be a missed opportunity to improve early initiation of ART in otherwise asymptomatic patients. Further studies in this respect would be of value.
Among all the patients included, we found a documented HIV seropositivity rate of >30%, with >50% of the samples with documented HIV status being collected from HIV-positive patients. Over 20% of the samples included were collected from HIV-positive patients in the outpatient/PHC setting, which probably reflects an increase in demand for laboratory testing related to ART monitoring. With the subsequent change in CD4 threshold, which means that all HIV-positive patients are now offered ART, the demand for laboratory resources would be expected to have risen since these data were collected. Among inpatients, the highest seropositivity rate was seen in the medical wards, where close to 60% of the patients were HIV-positive. The HIV seropositivity rates in most of the other disciplines assessed was ~28 - 40%, the exception being in the paediatric wards, where the lower rate (<20%) testifies to the success of the prevention of mother-to-child transmission programme. As an FBC is performed at least once in most hospital inpatients, HIV seropositivity rates in the FBCs collected from this patient subgroup can be viewed as a surrogate for rates among hospital inpatients in general. As there is very little formal documentation of the latter in the literature, these findings are of interest and reflect the significant burden of HIV infection among hospitalised state sector patients. However, these results should be treated with some degree of reserve given the fairly poor HIV documentation rate in most of the units (most notably in the obstetrics and gynaecology department). Since doctors are more likely to test for HIV when patients present with symptoms or possible complications of HIV infection, the prevalence rates reported here may be inflated. However, we found a similar seropositivity rate in the medical wards to that reported by Meintjes et al.,[13]who systematically tested patients admitted to the medical admission ward of a hospital serving a community in Cape Town of similar demographics to that served by CHBAH during 2012 and 2013. Furthermore, HIV seropositivity rates in women attending antenatal clinics in the City of Johannesburg and the West Rand in 2012 were 29.6% and 35.6%, respectively,[14] which are very similar to the rates we found in the non-medical disciplines. As sick patients with HIV are likely to seek medical assistance, it is not unexpected for hospital seropositivity rates to be higher than those of the surrounding apparently well community.
Study limitations
Limitations of this study include the limited data available on type and duration of ART exposure, which compromise accurate analysis in this respect. Differential white cell counts were available in <20% of patients, and the assessment for the prevalence of neutropenia is consequently weak. Furthermore, no information on transfusion history was available, which may affect the prevalence rates of cytopenias as well as assessment of their severity. Lastly, since this study was performed, ART guidelines have changed in respect of antiretroviral agents employed as well as the CD4 threshold for therapy initiation, which may have affected the prevalence of cytopenias to some extent. However, since cytopenias mainly occurred in patients with iAIDS (irrespective of ART), treatment of patients with normal CD4 counts is unlikely to have impacted on cytopenia rates in the short term. A follow-up study in this regard would be of interest.
Conclusions
More than 30% of the samples received for an FBC at the CHBAH NHLS laboratory were collected from HIV-positive patients, and the HIV seropositivity rate was >50% in those with documented HIV status. Among hospital inpatients, more than one-third were HIV-positive, with close to 50% of these being admitted to medical wards. Over 60% of the HIV-positive patients had one or more cytopenia/s, with anaemia being the most prevalent. Cytopenias were significantly more common among inpatients and individuals with iAIDS, but also occurred in close to 50% of outpatients and >50% of those on ART. These findings reflect the substantial impact of the HIV epidemic on state sector hospital and laboratory resources, particularly the haematology service.
REFERENCES
1. Sloand E. Hematologic complications of HIV infection. AIDS Rev 2005;7(4):187-196. [ Links ]
2. Sullivan PS, Hanson DL, Chu SY, Jones JL, Ward JW. Epidemiology of anemia in human immuno deficiency virus (HIV)-infected persons: Results from the multistate adult and adolescent spectrum of HIV disease surveillance project. Blood 1998;91(1):301-308. [ Links ]
3. Dikshit B, Wanchu A, Sachdeva RK, Sharma A, Das R. Profile of hematological abnormalities of Indian HIV infected individuals. BMC Blood Disord 2009;9(1):5. http://dx.doi.org/10.1186/1471-2326-9-5 [ Links ]
4. Akinbami A, Oshinaike O, Adeyemo T, et al. Hematologic abnormalities in treatment-naive HIV patients. Infect Dis Res Treat 2010;3(1):45-49. http://dx.doi.org/10.4137/IDRT.S6033 [ Links ]
5. Firnhaber C, Smeaton L, Saukila N, et al. Comparisons of anemia, thrombocytopenia, and neutropenia at initiation of HIV antiretroviral therapy in Africa, Asia, and the Americas. Int J Infect Dis 2010;14(12):e1088-e1092. http://dx.doi.org/10.1016/j.ijid.2010.08.002 [ Links ]
6. Munyazesa E, Emile I, Mutimura E, et al. Assessment of haematological parameters in HIV-infected and uninfected Rwandan women: A cross-sectional study. BMJ Open 2012;2(6). http://dx.doi.org/10.1136/bmjopen-2012-001600 [ Links ]
7. Kyeyune R, Saathoff E, Ezeamama AE, Loscher T, Fawzi W, Guwatudde D. Prevalence and correlates of cytopenias in HIV-infected adults initiating highly active antiretroviral therapy in Uganda. BMC Infect Dis 2014;14(1):496. http://dx.doi.org/10.1186/1471-2334-14-496 [ Links ]
8. Servais J, Nkoghe D, Schmit JC, et al. HIV-associated hematologic disorders are correlated with plasma viral load and improve under highly active antiretroviral therapy. J Acquir Immune Defic Syndr 2001;28(3):221-225. http://dx.doi.org/10.1097/00042560-200111010-00003 [ Links ]
9. UNAIDS. 2014. http://www.unaids.org/en/regionscountries/countries/southafrica (accessed 27 January 2017). [ Links ]
10. Kerkhoff AD, Wood R, Cobelens FG, Gupta-Wright A, Bekker LG, Lawn SD. Resolution of anaemia in a cohort of HIV-infected patients with a high prevalence and incidence of tuberculosis receiving antiretroviral therapy in South Africa. BMC Infect Dis 2014;14(1):3860. http://dx.doi.org/10.1186/s12879-014-0702-1 [ Links ]
11. Takuva S, Maskew M, Brennan AT, Sanne I, Macphail AP, Fox MP. Anemia among HIV-infected patients initiating antiretroviral therapy in South Africa: Improvement in hemoglobin regardless of degree of immunosuppression and the initiating ART regimen. J Trop Med 2013;2013(1):162950. http://dx.doi.org/10.1155/2013/162950 [ Links ]
12. De Santis GC, Brunetta DM, Vilar FC, et al. Hematological abnormalities in HIV-infected patients. Int J Infect Dis 2011;15(12):e808-e811. http://dx.doi.org/10.1016/j.ijid.2011.08.001 [ Links ]
13. Meintjes G, Kerkhoff AD, Burton R, et al HIV-related medical admissions to a South African district hospital remain frequent despite effective antiretroviral therapy scale-up. Medicine 2015;94(50):e2269. http://dx.doi.org/10.1097/md.0000000000002269 [ Links ]
14. The 2012 National Antenatal Sentinel HIV & Herpes Simplex Type-2 Prevalence Survey in South Africa. 2012. https://www.health-e.org.za/wp-content/uploads/2014/05/ASHIVHerp_Report2014_22May2014.pdf (accessed 1 November 2016). [ Links ]
 Correspondence:
Correspondence:
J Vaughan
jenifer.vaughan@nhls.ac.za
Accepted 25 November 2016














