Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.106 no.11 Pretoria Nov. 2016
http://dx.doi.org/10.7196/samj.2016.v106i11.12013
RESEARCH
Intimate partner violence at a tertiary institution
K SpencerI; M HaffejeeII; G CandyIII; E KasekeIV
IMB BCh; Department of Urology, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIMB BCh, FCS (Urol); Department of Urology, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIIMSc, PhD; Department of Surgery, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IVBA, PhD; Department of Social Work, Faculty of Humanities, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
BACKGROUND. Intimate partner violence (IPV) is actual or threatened physical, sexual, psychological, emotional or stalking abuse by an intimate partner. Despite the high prevalence of IPV in South Africa (SA), there is a paucity of data on university students training in fields where they are likely to have to manage the after-effects of such events in their personal capacity in the future.
OBJECTIVES. To ascertain the prevalence of IPV in an SA tertiary institution population with a diverse demographic profile.
Methods. Students from the faculty of health sciences and the faculty of humanities, social work department, completed an anonymous questionnaire. Students were made aware of psychological counselling available to them.
Results. Responses were obtained from 1 354 of 1 593 students (85.0%) (67.8% female, 45.9% black, 32.7% white, 16.6% Indian, 4.8% coloured). Of the respondents, 53.0% indicated that they were in a relationship. The prevalence of any type of IPV (sexual, physical or emotional abuse) among all respondents was 42.6%. Emotional abuse was reported by 54.9% of respondents, physical abuse by 20.0% and sexual abuse by 8.9%. Thirty-five females (6.5% of respondents who had suffered IPV) indicated that they had been emotionally, physically and sexually abused. Fourteen percent identified themselves as perpetrators of abuse, but only three perpetrators of sexual abuse reported having also been victims of sexual abuse. Most respondents (58.7%) knew where to get help.
CONCLUSION. The extent of IPV among the medical and social work students sampled was found to be unacceptably high, both as victims and as perpetrators. As a result of their exposure to IPV, these individuals may have difficulty in managing patients who have been subjected to abuse.
Victims of intimate partner violence (IPV) may experience numerous physical, sexual, psychological, behavioural and even fatal consequences (Table 1).[1] These include an increased number of visits to emergency departments, and an increased risk of gastrointestinal, cardiovascular, gynaecological and psychiatric disorders, including depression, substance abuse and post-traumatic stress disorder.[1] Women who refuse to have sex without a condom have an increased likelihood of becoming IPV victims, and if forced to do so face the additional risk of sexually transmitted infections, including HIV, and unplanned pregnancies.[1] The effects of IPV may not be immediately apparent, and may only manifest with targeted questioning or after an examination. It is precisely because of the complexity of these implications that it is important for the clinician to know how to screen for and manage these individuals.

The World Report on Violence and Health[1] defines IPV as 'actual or threatened physical, sexual, psychological, emotional, or stalking abuse by an intimate partner'. An intimate partner can be a current or former spouse or a non-marital partner, such as a boyfriend, girlfriend or dating partner, and can be someone of the same or the opposite sex. The South African (SA) Domestic Violence Act 116 of 1998[2] expands on this definition and speaks of a 'complainant' as any person who is or has been in a domestic relationship and has been or allegedly has been subjected to an act of domestic violence. The term domestic relationship is all-encompassing and includes customary marriages, various types of relationships and even flatmates. The definition of domestic violence is further expanded to include economic abuse, intimidation, harassment, stalking, damage to property, entry into the complainant's residence without consent, and controlling behaviour.[2]
Looking at the global prevalence rates, a review of more than 50 population-based studies from 35 nations found that 10 - 52% of females reported that they had been physically abused, and 10 - 30% had experienced sexual violence from an intimate partner at some point in their lives.[3] The reported IPV prevalence of 20 - 71% in sub-Saharan Africa has been thought to be an underestimate due to under-reporting and poor standardisation of methods.[3]
A national study from SA found a 19% lifetime prevalence of victimisation among female participants and a 27.5% prevalence of men perpetrating violence in their current or most recent relationship.[4] More than 50% of female homicide victims were killed by their intimate partners.[4] Furthermore, an SA study on female homicide indicated that every 6 hours a woman was killed by her intimate partner.[5]
University students are considered an elite sector of society, and it could be assumed that attending a tertiary institution would render individuals less likely to be perpetrators or victims of IPV.[6] Some of these students study towards careers in which they will need to deal with the victims of IPV. There is a paucity of data relating to SA students who are victims of IPV, particularly in the fields of medicine and social work. The objective of this study was to ascertain the prevalence of and gender differences in IPV in a group of students studying to be healthcare workers in an SA tertiary institution.
Methods
Approval to conduct the study was obtained from the University of the Witwatersrand Human Research Ethics Committee (ref. no. M120670).
Study participants
A sample of male and female students from the medical school and department of social work at a university in Gauteng Province, SA, were asked to complete a quantitative anonymous questionnaire. The sample consisted of all 1st- to 6th-year medical students and all 1st- to 4th-year social work students. These two faculties comprised 1 593 students, and the decision was made to use the entire group as a sample. Connor et al.[7]found that students who received education about IPV while at medical school reported having greater confidence and perceived preparedness to deal with IPV victims. We therefore selected this population because they would be exposed to IPV and would be likely to screen for it.
Data collection process
The consent process consisted of a brief presentation by the first author (KS) detailing the study prior to handing out the questionnaire. The information sheets, consent forms and questionnaires were handed out after lectures or exam sessions. Participation in the study was voluntary, and students were told they could leave questions unanswered if necessary. An electronic marking sheet was used, and the questionnaires were anonymous with no name or student number reflected anywhere on the response sheet. Completed questionnaires were then placed into a sealed box. After the survey, each student was given a form with the contact details of a dedicated psychological counselling service available to them if they experienced discomfort as a result of the survey process.
Data collection tool
Two recommended screening tools from the US Centers for Disease Control and Prevention (CDC) were combined to create 25 multiple-choice questions, which were adapted to the SA context. These tools were the computer-based IPV Questionnaire and the Women Abuse Screening Tool (WAST). The WAST had a Cronbach's alpha of 0.75 estimated for the reliability of the tool and a correlation with the construct validity of the Abuse Risk Inventory of 0.69.[8]
The data collection tool comprised four domains, of which this article covers only two - demographics and the prevalence of the different types of abuse.
The first six questions requested demographic information from the participants, including the degree for which they were enrolled (medicine or social work), year of study, age group, gender, racial group and relationship status.
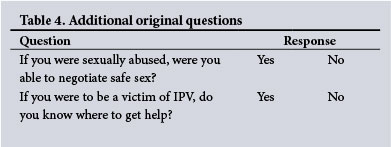
Questions 14, 15 and 16 were about relationships and were derived from the Women Abuse Screening Tool (Table 2).[8] Questions 11 -13 and 17 - 22 were derived from the questions on the computer-based IPV questionnaire listed in Table 3.[8] Two questions involving handguns from the original IPV questionnaire were not included in this questionnaire. Questions 24 and 25 were original questions (Table 4).
Statistical analysis
The results of each sheet were tallied electronically per question. Data were recorded on an Excel 2013 spreadsheet (Microsoft, USA), and Statistica version 12 (Statsoft, USA) was used for all statistical procedures. Descriptive statistics were reported as totals and percentages for categorical data. Comparative statistics were done using a χ2 test or Fisher's exact test as appropriate, with a p-value of <0.05 being considered statistically significant.
For the purposes of definition, participants were deemed to have been victims of physical abuse if they answered in the affirmative to the questions referring to being pushed, kicked, or otherwise physically hurt, victims of sexual abuse if they had been made to have sex (oral, anal, vaginal) when they did not want to, and victims of emotional abuse if they answered in the affirmative to the question directly asking the respondent whether he/she had been emotionally abused. The definition of emotional abuse was further expanded to include whether a partner gets very jealous or tries to control the respondent's life, tries to keep them away from family or friends, says insulting things or threatens them, is disagreeable, or may try to hurt them or other family members.
Results
Responses were obtained from 1 354 of the 1 593 students (85.0%). The responses collected were similar for each year of study. Most respondents were aged 20 - 24 years (61.9%) and were female (67.8%); 45.9% were black, 32.7% white, 16.6% Indian and 4.8% coloured (Table 5).

Fifty-three percent of the respondents were in a relationship, engaged or married. Of the 718 respondents who reported that they were in a relationship, 123 (17.1%) indicated that they had a jealous partner. Of the remaining 636 respondents who indicated they were not currently in a relationship, a very similar proportion (n=127; 19.9%) indicated that they had had a jealous partner in the past. The following responses pertain to respondents in a relationship (n=718): 40 (5.6%) often and 250 (34.8%) sometimes felt that their partner tried to keep them away from family and friends, while 250 (34.8%) reported that their partner was sometimes insulting or threatening towards them and 123 (17.1%) were afraid to disagree with their partner because they might hurt them or other family members. Two hundred and three respondents (28.3%) felt that there was some tension in their current relationship, 310 (43.2%) experienced some difficulty when settling arguments with their partners, 555 (77.3%) sometimes felt lowered self-esteem after settling an argument, and 124 (17.3%) were afraid not to agree with their partner.
The prevalence of any type of IPV (sexual, physical or emotional abuse) among all the respondents was 42.6% (577/1 354). Emotional abuse was the most common type of abuse (35.0% of respondents). With the expanded definition of emotional abuse (as above) the prevalence increased to 54.9%. Physical abuse (20.0%) and sexual abuse (8.9%) were reported less often. Thirty-five females (6.5% of respondents who had suffered IPV) indicated that they had been emotionally, physically and sexually abused. Most of these females (28/35, 80.0%) indicated they were not currently in a relationship.
With sexual abuse, although no trend according to age was apparent among male students, the percentage of females reporting sexual abuse increased by 6.1% between the 17 - 19-year-old (9.8%) and > 24-year-old (15.9%) age groups. Older females (>24 years) appeared more vulnerable to emotional (43.4%) and sexual abuse (15.9%) (Fig. 1).

Responses of females relating to questions pertaining to whether the partner was isolating or insulting, to whether there was tension in the relationship, and to settling of arguments and disagreeing with a partner did not appear to indicate a major problem, with less than half of the respondents reporting that these were issues. However, overall 59.5% of female respondents in a relationship aged < 25 years indicated they had a jealous partner. Furthermore, overall 68.0% had arguments resulting in the individual 'feeling bad' often (14.4%) or sometimes (55.2%). This response was also more common in the two younger age groups. Of all the victims of sexual abuse, 45.0% were at least able to negotiate protected sex. Overall, 58.7% of the respondents knew where they could get help and counselling as victims of abuse.
The perpetrators (14.0% of total respondents) of IPV tended to be males in the white and Asian ethnic groups, females among coloured respondents, and without an apparent gender difference (p=0.55) among black respondents. There were no age-related differences (males p=0.87 and females p=0.69) among the perpetrators, although younger males were more often perpetrators in the 17 - 19-year age group. Only three perpetrators of sexual abuse indicated that they themselves had been sexually abused.
Discussion
Future healthcare workers tend to provide superior management to victims of IPV when they seek assistance for themselves first. Christofides and Silo[9] found that practitioners who reported their own, a friend's or a family member's experience with IPV had an increased 'quality of care score'. This could be the result of their ability to identify and empathise with victims. Kim and Motsei[6] stated that healthcare workers who were victims of IPV tended to have the same cultural values as the victims they treated and counselled, underlining the 'gender-bound constructs' within which they operated, which extended from their personal to their professional capacities. Sugg and Inui,[10] however, reported that doctors were 'emotionally inactivated' and therefore not able to manage patients with similar experiences, and might experience personal distress.
This study determined the prevalence of IPV in an SA tertiary institution population, representative of the ethnic makeup of the national population. The study is unusual as it obtained responses from medical and social work students in all years of study and from respondents of both genders. These students, whose future professions include counselling of victims of abuse, would be expected to be aware of this problem.
The total prevalence of IPV at the institution in question was 42.6%, comparable to a study from China that found a prevalence of 37.1%.[11] The university with the highest reported prevalence of IPV victims was in Nigeria, with a figure of 58.8% for female students.[12] Studies at other universities found varying prevalences (in descending order) from 28.7% (Tennessee), 22% (Wisconsin) and 10% (Vanderbilt) in the USA, to 7% (Ontario, Canada).[13-16] A study at numerous institutions in the UK found an overall prevalence of 14.2%.[17]
In line with previous studies, the present study found a higher prevalence of female (particularly in the older age groups) than male IPV victims. A report from the Office of Justice in the USA[18] stated that female students in full-time education were at a higher risk of sexual violence than the general female population. Several risk factors were noted: 'living on campus, being unmarried, getting drunk frequently, and experiencing prior sexual victimization'.[19]
In an SA study by Gass et al.[4]it was found that the single most common risk factor for IPV victims of both genders was witnessing parental violence. Specific risk factors pertaining to male victims included 'low income and lack of closeness to a primary female caregiver', whereas risk factors for female victims included 'low educational attainment, childhood physical abuse, and adult-onset alcohol abuse/dependence and intermittent explosive disorder'.[4] IPV has been strongly linked to intergenerational cycling of violence and risk exposure across the life course.[4]
An interesting observation in our study was the low use of condoms. Peltzer[19] had similar findings, and reported that 29.2% of SA students never, 35.4% always, 19.8% regularly and 8.5% irregularly used condoms over a 3-month period. This is concerning given the high national HIV incidence and that this was a well-educated group of individuals who should be aware of the risks of unprotected sexual intercourse.
An interesting and unexpected finding was the high rate of female perpetrators, particularly among black and coloured students. The National Intimate Partner and Sexual Violence Survey by the CDC expanded the definition of IPV to include rape while under the influence of illicit drugs, undesirable touching, expressive aggression, conceiving by coercion, refusing to use a condom, and stalking.[20] With the new definition they found an equal rate of perpetration between the genders. Female aggressors are also at increased risk of becoming a victim later on.[21] Gass et al.[4]reported that risk factors in male perpetrators were likely to include cohabitation, low income and early- and adult-onset mood disorders, whereas risk factors in female perpetrators included low educational attainment and early-onset alcohol abuse/dependence.
Medical schools need to have appropriate support mechanisms in place for victims and potential victims of IPV, and students should be given a list of local resources. According to Ambuel et al.,[14] students need to be allowed to process their feelings and experiences within their academic spaces. There should be a safe environment that fosters open, respectful sharing of experiences and ideas, appropriate supervision, and encouragement of responsible self-care including access to psychotherapy and support groups. To this end, our institution has dedicated psychology and counselling services available. Broader institutional and policy changes should also be implemented in academic programmes to enable early detection and management.[14]
Study limitations
Concepts such as physical, sexual or emotional abuse could have been better defined, as the questions assumed that students had prior knowledge or understood the scope of abuse as defined by current legislation. This may have affected their ability to answer the questions. Certain components of emotional abuse as defined by the SA Domestic Violence Act were not specifically included, such as economic abuse, intimidation, harassment, stalking, damage to property, and entry into the complainant's residence without consent. The participants may also have had different perceptions of what defines sexual abuse, and the fact that a person did not agree with the statement does not mean it did not happen. If the data collection tools had covered these various other forms of IPV, labelled domestic violence under the Domestic Violence Act, the prevalence rate might have differed.
Conclusion
The extent of emotional, physical and sexual abuse among university medical and social science students sampled was unacceptably high, both as victims and as perpetrators. As a consequence of their own experiences of abuse, these individuals may have difficulty in managing patients who have been subjected to abuse. To determine possible regional differences in this unacceptable practice, it is recommended that similar surveys be undertaken at other centres of higher learning.
Acknowledgements. The authors acknowledge Amitha Betchan and Magali de la Kethulle de Ryhove for their administrative assistance, and Deidre Pretorius for her advice.
References
1. Krug EG, Dahlberg LL, Mercy JA, Zwi AB, Lozano R, eds. World Report on Violence and Health. Geneva: World Health Organization, 2002. [ Links ]
2. Republic of South Africa. Domestic Violence Act 116 of 1998. http://www.justice.gov.za/legislation/acts/1998-116.pdf (accessed 1 August 2016). [ Links ]
3. Karamagi CAS, Tumwine JK, Tylleskar T, Heggenhougen K. Intimate partner violence against women in eastern Uganda: Implications for HIV prevention. BMC Public Health 2006;6(284):458-470. DOI:10.1186/1471-2458-6-284 [ Links ]
4. Gass JD, Stein DJ, Williams DR, Seedat S. Intimate partner violence, health behaviours and chronic physical illness among South African women. S Afr Med J 2010;100(9):582-585. [ Links ]
5. Lau U. Intimate partner fact sheet. University of South Africa, 2009. http://www.mrc.ac.za/crime/intimatepartner.pdf (accessed 16 May 2016). [ Links ]
6. Kim J, Motsei M. Women enjoy punishment: Attitudes and experiences of gender-based violence among PHC nurses in rural South Africa. Soc Sci Med 2002;54(8):1243-1254. DOI:10.1016/S0277-9536(01)00093-4 [ Links ]
7. Connor PD, Nouer SS, Mackey SN, Banet MS, Tipton NG. Intimate partner violence education for medical students: Toward a comprehensive curriculum revision. South Med J 2012;105(4):211-215. DOI:10.1097/SMJ.0b013e31824f8b01 [ Links ]
8. Basile KC, Hertz MF, Back SE. Intimate Partner Violence and Sexual Violence Victimization Assessment Instruments for Use in Healthcare Settings: Version 1. Atlanta, Ga: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, 2007. https://www.cdc.gov/violenceprevention/pdf/ipv/ipvandsvscreening.pdf (accessed 16 May 2016). [ Links ]
9. Christofides NJ, Silo Z. How nurses' experiences of domestic violence influence service provision: Study conducted in North-West Province, South Africa. Nurs Health Sci 2005;7(1):9-14. DOI:10.1111/j.1442-2018.2005.00222.x [ Links ]
10. Sugg NK, Inui T. Primary care physicians' response to domestic violence: Opening Pandora's box. JAMA 1992;267(23):3157-3160. DOI:10.1001/jama.267.23.3157 [ Links ]
11. Su PY, Hao JH, Huang ZH, Xiao LM, Tao FB. An investigation on the epidemic situation of intimate partner violence in 2,575 college students. Zhonghua Liu Xing Bing Xue Za Zhi 2011;32(4):346-351. [ Links ]
12. Iliyasu Z. Prevalence and correlates of gender-based violence among female university students in Northern Nigeria. Afr J Reprod Health 2011;15(3):111-119. DOI:10.4314/ajrh.v15i3.71443 [ Links ]
13. Connor PD, Nouer SS, Mackey SN, Tipton NG, Lloyd AK. Psychometric properties of an intimate partner violence tool for health care students. J Interpers Violence 2011;26(5):1012-1035. DOI: 10.1177/0886260510365872 [ Links ]
14. Ambuel B, Butler D, Hamberger LK, Lawrence S, Guse CEE. Female and male medical students' exposure to violence: Impact on wellbeing and perceived capacity to help battered women. J Comp Fam Stud 2003;34(1):113-135. [ Links ]
15. Ernst AA, Houry D, Nick TG, Weiss SJ. Domestic violence awareness and prevalence in a first-year medical school class. Acad Emerg Med 1998;5(1):64-68. DOI:10.1097/00007611-200093080-00006 [ Links ]
16. Sprague S, Kaloty R, Madden K, Dosanjh S, Mathews DJ, Bhandari M. Perceptions of intimate partner violence: A cross sectional survey of surgical residents and medical students. J Inj Violence Res 2013;5(1):1-10. DOI:10.5249/jivr.v5i1.147 [ Links ]
17. Smith G. National Union of Students: Hidden marks, a study of women students' experiences of harassing, stalking, violence and sexual assault, 2010. http://www.nus.org.uk/Global/NUS_hidden_marks_report_2nd_edition_web.pdf (accessed 16 May 2016). [ Links ]
18. Fisher BS, Cullen FT, Turner MG. The sexual victimization of college women. US Department of Justice, 2000. https://www.ncjrs.gov/pdffiles1/nij/182369.pdf (accessed 28 August 2016). [ Links ]
19. Peltzer K. Factors affecting condom usage among South African university students. East Afr Med J 2000;77(1):46-52. DOI:10.4314/eamj.v77i1.46384 [ Links ]
20. Black MC, Basile KC, Breiding MJ, et al. The National Intimate Partner and Sexual Violence Survey. Atlanta, Ga: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, 2010. http://www.cdc.gov/violenceprevention/pdf/nisvs_report2010-a.pdf (accessed 16 May 2016). [ Links ]
21. Hoff B. US national survey: More men than women victims of intimate partner violence. J Aggress Confl Peace Res 2012;4(3):155-163. DOI:10.1108/17596591211244166 [ Links ]
 Correspondence:
Correspondence:
K Spencer
doctorkspencer@gmail.com
Accepted 19 September 2016














