Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.106 n.8 Pretoria Aug. 2016
http://dx.doi.org/10.7196/samj.2016.v106i8.10566
RESEARCH
A clinical audit of the utilisation of red cell products in elective total hip replacement surgery
Y G PetersI, II; A R BirdIII; G R M BellairsIV; G M DavisonV
IBTech; Western Province Blood Transfusion Service, Pinelands, Cape Town, South Africa
IIBTech; Department of Biomedical Sciences, Faculty of Health and Wellness Sciences, Cape Peninsula University of Technology, Bellville, Cape Town, South Africa
IIIMMed, FCPath (SA); Western Province Blood Transfusion Service, Pinelands, Cape Town, South Africa
IVMB ChB, MBA, Postgrad Dip Transfusion Med; Western Province Blood Transfusion Service, Pinelands, Cape Town, South Africa
VPhD; Department of Biomedical Sciences, Faculty of Health and Wellness Sciences, Cape Peninsula University of Technology, Bellville, Cape Town, South Africa
ABSTRACT
BACKGROUND: Previous studies have documented a marked variation in transfusion practice for total hip replacement (THR) surgery.
OBJECTIVE: To audit red cell product utilisation for THR at two Western Cape tertiary referral hospitals (HY and HG).
METHODS. The folders of 207 consecutive patients undergoing elective THR surgery from January 2013 to December 2013 were reviewed. Information relating to age, sex, clinical observations, indications for surgery, pre- and postoperative haemoglobin (Hb) values, comorbidities, length of hospital stay and transfusion history was recorded.
RESULTS: The transfusion rate at HY (41.6%) was significantly higher than that at HG (10.0%). The mean postoperative Hb in the transfused patients at HG was 8.3 g/dL v. 9.1 g/dL at HY. Females had a significantly higher transfusion rate (33.0%) than males (15.0%) (p<0.05), and the mean age of transfused patients was significantly greater than that of untransfused patients (p<0.005). Although patients with comorbidities had a higher transfusion rate than those without, this did not reach statistical significance. Of 120 patients with complete data, 113 (94.2%) had a blood bank order, of which the vast majority, 102/113 (90.3%), were group-and-screen (G&S) requests; 29/113 (25.7%) were converted to a full crossmatch.
CONCLUSIONS: Overall, the transfusion rate for both hospitals was 25.8%, which is well within published rates. A guideline Hb trigger of 8.0 g/dL is recommended as per published guidelines, with the caveat that the clinical judgement of the attending clinician whether a transfusion is indicated is paramount. Causes of preoperative anaemia should be investigated and treated. Routine cross-matching preoperatively is unnecessary, and a G&S order is sufficient.
As a result of recent advances in diagnostic technology developed to screen for transfusion-transmissible diseases (TTDs), the inactivation of pathogens and improvement in good manufacturing practice, the risk of acquiring a TTD is extremely low. In South Africa (SA), there have been one documented HIV and two hepatitis B virus window period infections since the introduction of individual donation screening by nucleic acid amplification testing in October 2005 (C Ingram, South African National Blood Service, personal communication, 2015).
However, blood transfusions still carry infectious risks, even though these are very slight, as well as other well-documented hazards. Consequently there has been an increased focus on appropriate blood management, with the publication of clinical trials carried out to establish evidence-based guidelines for the use of blood products. The publication of the TRICC (Transfusion Requirements in Critical Care) trial in 1999 showed that a restrictive approach to the use of red cell concentrates (RCCs) with a low haemoglobin (Hb) trigger of <8 g/dL had no harmful clinical effects and clinical outcomes were similar to those in patients treated with a more liberal transfusion regimen with the transfusion trigger set at 10 g/dL.[1] These findings have been supported by other studies focusing on high-risk patients undergoing hip surgery.[2]
Numerous clinical audits of blood utilisation measured against clinical guidelines have been published over the past decade. These audits serve as a tool to identify areas of practice that can be improved and therefore form part of quality improvement initiatives that may be used to enhance patient outcomes, improve safety and minimise costs. Elective surgical procedures are the most common target of transfusion audits, because they have the advantage of providing well-defined patient groups. One of the earliest and most comprehensive blood utilisation audits was the Sanguis project, which collected data from 43 teaching hospitals in Central and Western Europe. This study selected the following elective procedures, as they were frequently performed and often involved a request for blood products: right and left hemicolectomy (COLE) for colonic cancer, coronary artery bypass graft (CABG), unilateral total hip replacement (THR), abdominal aorta aneurysmectomy (AAA), laparoscopic cholecystectomy (CHOLE), and transurethral prostatectomy (TURP). The results indicated an extremely wide range of transfusion rates, prescribed doses and types of blood products used within the same patient category.[3,4] Furthermore, recent publications have continued to show this trend.[5-7]
Very few studies of blood utilisation practice have been conducted in SA.[8-10] Blood is a valuable and scarce resource, especially in a middle-income developing country, and there is therefore a need for transfusion audits to achieve optimal practice. In addition, there have been no audits examining the blood ordering practice for THR in SA. To fill this gap, a study of the utilisation of RCCs as well as blood ordering practices in elective THR was carried out by means of a retrospective clinical audit at two tertiary referral hospitals in the Western Cape Province.
Methods
Patient population and ethics
The study population consisted of consecutive patients each of whom had undergone elective THR surgery between 1 January and 31 December 2013. The folders were examined consecutively to avoid selection bias. Patients were excluded from the study if they had been admitted with a fracture to the hip due to trauma. The hospitals were encoded green (HG) and yellow (HY) to ensure anonymity, as per agreement with their management.
Ethics approval was obtained from the Cape Peninsula University of Technology Ethics Committee (Ref. no. CPUT/HW-REC2013/H38). Once approved, permission was obtained from the management of the respective hospitals.
Data collection and statistical analysis
A data collection form was devised as a tool to record the informat ion required for the audit. This included information relating to age, gender, clinical observations, indications for surgery, pre- and postoperative Hb values, comorbidities, length of hospital stay and transfusion history.
Data from individual data collection sheets were uploaded onto the IBM SPSS version 22 statistical package (IBM, USA) for analysis. From this, frequency tables, contingency tables and descriptive analysis for numerical variables using means, standard deviations (SDs) and standard errors were deduced. Summary statistics were given as means and SDs, and average values were presented as means or medians where deemed appropriate.
Performance indicators included the number of patients transfused per hospital as well as the number of units transfused per hospital. The χ2 test was used to identify significant differences between two or more groups pertaining to categorical variables or to test for a significant association between two categorical variables. Student's t-test was used to compare the difference of a numerical variable between two groups (e.g. mean female Hb v. mean male Hb), and p-values were given to test the null hypothesis. A p-value of <0.05 was considered significant and would therefore reject the null hypothesis.
Results
Study population
Two hundred and seven consecutive patients admitted for elective THR at two tertiary referral hospitals in the Western Cape between 1 January and 31 December 2013 were studied. Eighty-seven patients were excluded owing to incomplete data, recent hip trauma or underlying malignant disease, with the remaining 120 patients (Table 1) equally divided between the two hospitals.
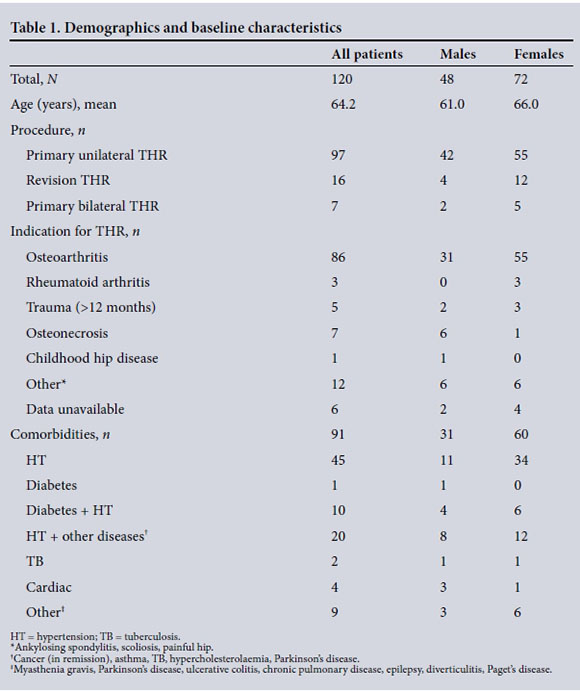
Transfusion rates
Fig. 1 compares the transfusion rates between the two hospitals. Thirty-one (25.8%) of all patients were transfused with RCCs, either intraoperatively or within 24 hours post-operatively. Of the 31 transfused patients, 6/60 (10.0%) were at HG and the remaining 25/60 (41.7%) at HY. Two to three units was the average dose (mean 2.7). The difference between the two hospitals was significant (χ2=15.701, p<0.001). Female patients had a significantly higher transfusion rate than males (χ2=5.285, p<0.05), and although patients with comorbidities were more likely to receive blood, this did not reach statistical significance.
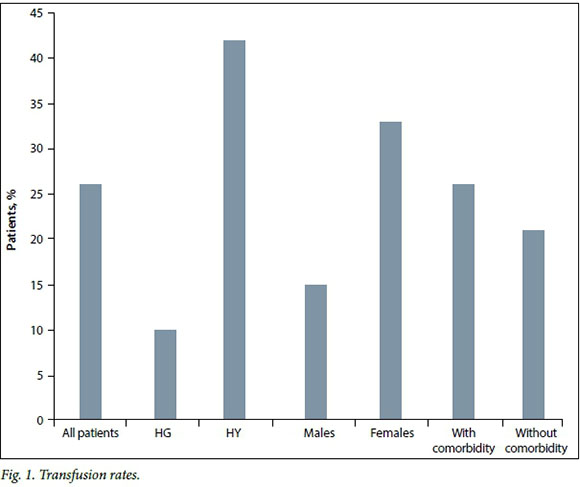
Haemoglobin values
Fig. 2 summarises the pre- and post-surgery Hb values for all patients and is further broken down into those who were transfused v. those who received no RCCs. On average, the postoperative Hb was 2.7 g/dL lower than the preoperative Hb in all patients. The transfused patients had significantly lower mean Hb values than those who were not transfused (pre-surgery Hb: t=4.821, p<0.001; post-surgery Hb: t=5.225, p<0.001).
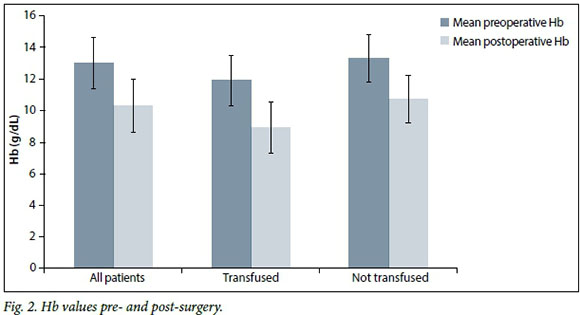
Fig. 3 compares the mean preoperative and postoperative Hb levels in transfused patients at each hospital. Postoperatively, the mean Hb value of the transfused patients was 8.1 g/dL at HG and 9.3 g/dL at HY. Three of the 6 transfused patients at HG (50.0%) had Hb values >8 g/dL, whereas at HY 17 of the 25 transfused patients (68.0%) had postoperative Hb values >8 g/dL.
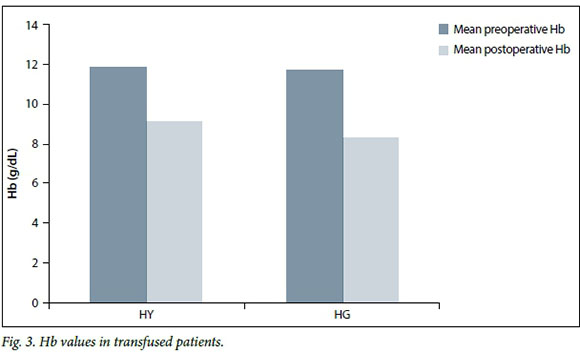
Gender
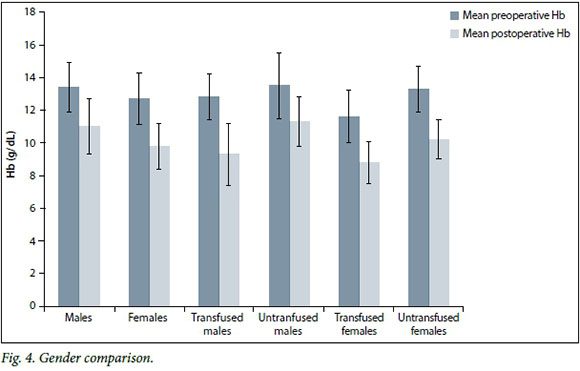
It is well established that there is a difference between the Hb values of males and females, and this is reflected in Fig. 4. The mean preoperative Hb for males and females was within the normal reference range for the Western Cape (National Health Laboratory Service). Despite this, the transfusion rate was significantly higher in female patients (p<0.05).
Patient age
There was no significant difference in the mean ages of the patients receiving blood at the two institutions (t=1.485, p>0.05).
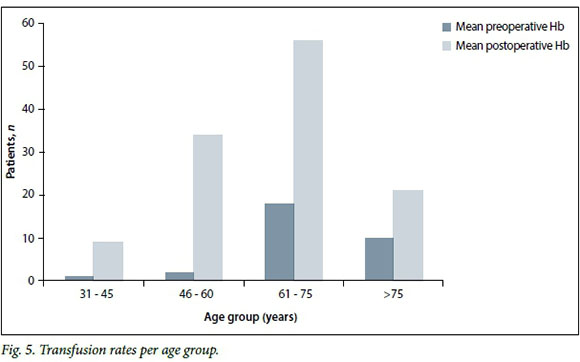
The majority of patients undergoing THR were aged >60 years; however, the transfusion rate increased significantly with increasing age. The mean age of those who did not receive a transfusion was 62.16 (SD 11.75) years, while the mean age of those who were transfused was 70.03 (SD 10.01) years (t=3.33, p<0.005).
Length of hospital stay (LOS)
The majority of patients were discharged within 6 - 10 days. No patient discharged by day 5 was transfused; in contrast, those receiving transfusions remained in hospital for a significantly longer period. In addition, LOS differed significantly between the two hospitals (mean p<0.001).
Comorbidities
As shown in Fig. 1, the transfusion rate for all patients with comorbidities was higher than in those without comorbidities, but this did not reach statistical significance.
Blood bank ordering analysis
Both hospitals used the group and screen (G&S) as the default order (n=54 at HG, n=48 at HY). Not unexpectedly, given the higher transfusion rate, HY had a larger number converted to a full cross-match, and the number of full cross-matches ordered preoperatively was three- to four-fold greater than at HG. HG requested full cross-matches for 10 patients, of whom 6 were transfused with 11 units of RCCs, and an average of two units per patient was transfused. At HY, blood was cross-matched for 30 patients, of whom 25 were transfused with 73 units of RCCs, averaging three units per patient.
Discussion
Variation in transfusion rates for THR has been well documented, but is not confined to this operation. Other major elective surgical operations such as CABG, total knee replacement and COLE show similar variations,[3,11,12] but these do not appear to be the result of patient mix, surgical technique or anaesthetic practices. A national auditof THR in the UK documented a 1 - 100% variation.[5] Studies in Europe revealed a similar variation.[6,7] In the Sanguis study,[3] a number of patients also received albumin, artificial colloids, plasma and platelets.
Although the variation in blood utilisation practice is not as wide, our study has demonstrated a significant difference in the rate of transfusion of RCCs between the two tertiary referral hospitals. A consistent 2 - 3 g/dL drop in Hb values postoperatively was documented in the studies mentioned above, and our study showed a similar mean decrease in postoperative Hb values of 2.7 g/ dL. This suggests that the average intra- and postoperative blood loss is fairly consistent and that variable blood loss from centre to centre is unlikely to be the cause of the variation.
In a systematic review published in 2011, Barr et al.[13] found that two factors consistently influenced the use of RCCs in orthopaedic surgery, namely preoperative Hb and age. Other factors were increased surgical complexity (e.g. revision THR), low body weight, comorbidities and female gender.[13] In our study, the transfused patients had significantly lower mean preoperative and postoperative Hb values (Fig. 2). Extrapolating from Fig. 2, the 'trigger' Hb value for transfusion at HG is 8.1 g/ dL, whereas at HY this appears to be higher at 9.3 g/dL. Three of the 6 patients (50.0%) transfused at HG had Hb values >8.0 g/dL, while at HY 17 (68.0%) of the 25 transfused patients had Hb values >8.0 g/dL.
In common with other studies, female gender had a significant association with the likelihood of transfusion. The mean preoperative Hb was within the normal NHLS reference range for both females and males, however, so the reason for the higher transfusion rate in females is unclear.
The mean age of patients in most published studies of THR ranged from 63 to 70 years. The mean age of the patients in our study is comparable, and there was no significant difference between HG and HY. However, the mean age of patients who received blood was 70 years, which is significantly greater than that of patients who received no blood (p<0.005).
Patients with comorbidities had a higher transfusion rate than those without, but this did not reach statistical significance (p>0.05). This may simply reflect the smaller number of patients studied compared with other reports, where the numbers were far greater and comorbidities influenced the likelihood of transfusion.
Although Barr et al.[13] did not identify LOS as a factor influencing the transfusion rate, our study revealed that an increased LOS was associated with an increased likelihood of transfusion. At both HG and HY, significantly more patients who were transfused had a hospital stay of >6 days, and all untransfused patients had an LOS of <5 days. This association could, however, reflect the clinical condition of the patients and the presence of comorbidities that were also present in patients receiving blood transfusions.
A G&S was the majority order of choice. This is appropriate given the overall transfusion rate and is in line with local clinical guidelines. If the blood bank is on the hospital premises, an argument could be made to dispense with the G&S since blood can be ordered and delivered rapidly from an on-site blood bank.
Study limitations
This was an observational retrospective study and as such has inherent weaknesses. Nevertheless, it has highlighted the need for clinical audits in units with regular blood product use to benchmark blood management practice. Concurrent or prospective audits are preferable, although they are more difficult to conduct.
Conclusions
The findings of this audit have led to the conclusion and recommendation that all centres should have a policy for blood management that should include the following:
• A guideline 'trigger' Hb value of 8.0 g/dL is recommended because studies have shown that a restrictive transfusion policy is safe in otherwise stable isovolaemic patients, and guidelines[14,15] have endorsed this.This is a guideline, however, and must be used together with clinical evaluation.
• Transfusion rates must be monitored and reviewed regularly. Although it is difficult to provide a benchmark, given the wide variation documented, Barr et al.[13] reported that the average transfusion rate in patients undergoing THR or total knee arthroplasty was 26%. There are, however, a number of centres reporting a transfusion rate of <20%,[13] so it would not be unreasonable to have this as a target.
• This study also noted that many patients were anaemic preoperatively, in which case the cause of the anaemia should be identified and it should be treated if the cause is treatable (e.g. iron deficiency).[16,17]
• A G&S is recommended as the pre-operative blood order.
In summary, this study demonstrated a significant difference in the transfusion rates between the two hospitals. Regular follow-up audits of blood utilisation should be conducted to compare current practice with local or international standards. This would ensure that blood wastage and unnecessary expenditure are kept to a minimum. Furthermore, blood donations would be optimally utilised and blood bank requests would be appropriate and essential.
The authors would like to thank Dr Corrie Uys from the Cape Peninsula University of Technology for performing the statistical analysis.
References
1. Hebert PC, Wells G, Blajchman MA, et al., with the Transfusion Requirements in Critical Care Investigators for the Canadian Critical Care Trials Group. A multicentre randomized controlled clinical trial of transfusion requirements in critical care. N Engl J Med 1999;340(6):409-417. DOI:10.1056/NEJM.19990211 [ Links ]
2. Carson J, Terrin M, Noveck H, et al Liberal or restrictive transfusion in high risk patients after hip surgery. N Engl J Med 2011;365(26):2453-2462. DOI:10.1056/NEJM? [ Links ]
3. Sanguis Study Group. Group use of blood products for elective surgery in 43 European hospitals Transfus Med 1994;4(4):251-266. DOI:10.1111/j.1365-3148.1994.tboo262.x [ Links ]
4. McClelland DBL. Red cell transfusion for elective surgery: A suitable case for treatment. Transfus Med 1994;4(4):247-249. DOI:10.1111/1365-3148.1994.tboo201.x [ Links ]
5. Boralessa B, Goldhill DR, Tucker K, et al. National comparative audit of blood use in elective primary unilateral total hip replacement surgery. Ann R Coll Surg Engl 2009;91(7):599-605. DOI:10.1308/003588409X432464 [ Links ]
6. Jans O, Kehlet H, Hussain Z, Johansson PI. Transfusion practice in hip arthroplasty. Vox Sang 2011;100(4):374-380. DOI:10.1111/j.1423-0410.2010.01428.x [ Links ]
7. Rosencher N, Kerkkamp HEM, Macheras G, et al. Orthopaedic Surgery Transfusion Haemoglobin European Overview (OSTHEO) Study: Blood management in elective knee and hip arthroplasty in Europe. Transfusion 2003;43(4):459-469. DOI:10.1046/j.1537-2995.00348.x [ Links ]
8. Rund RL, Bird AR, James MFM. Blood usage in elective surgery - a 3-month audit at Groote Schuur Hospital, Cape Town. S Afr Med J 1992;81(4):415-418. [ Links ]
9. Bidmos A, Nel T. The usage of red cell products at Kimberley Hospital Complex: A retrospective study. Afr J Haematol Oncol 2011;2(2):195-196. [ Links ]
10. Harrison MC, Pillay S, Joolay Y, et al Resource implications of adopting a restrictive neonatal blood transfusion policy. S Afr Med J 2013;103(12):916-917. DOI:10.7196/SAMJ.6858 [ Links ]
11. Bennet-Guerrero E, Zhao Y, O'Brien SM, et al. Variation in use of blood transfusion in coronary artery bypass surgery. JAMA 2010;304(14):1568-1575. DOI:10.1001/jama.2010.1046 [ Links ]
12. Gombotz H, Rehak PH, Shander A, Hoffman A. Blood use in elective surgery: The Austrian benchmark study. Transfusion 2007;47(8):1468-1480. DOI:10.1111/j.1537-2995.2007.01286.x [ Links ]
13. Barr PJ, Donnelly M, Cardwell C, et al. Drivers of transfusion decision making and quality of the evidence in orthopaedic surgery: A systematic review of the literature. Transfus Med Rev 2011;25(4):304-316. DOI:10.1016/j.tmrv.2011.04.003 [ Links ]
14. Carson J, Grossman B, Kleinman S, et al. Red blood cell transfusion: A clinical practice guideline from the AABB. Ann Intern Med 2012;157(1):49-58. DOI:10.7326/0003-4819-157-1-201206190-00429 [ Links ]
15. Ingram C, Bellairs G, Bird AR, eds. Clinical Guidelines for the Use of Blood Products in South Africa. 5th ed. WP Blood Transfusion Service and SANBS, 2014. http://www.sanbs.org.za/PDFDocuments/services/Clinical%20Guidelines/Clinical_Guigelines_5th-Edition2014.pdf (accessed 11 July 2016). [ Links ]
16. Spahn DR. Anemia and patient blood management in hip and knee surgery: A systematic review of the literature. Anesthesiology 2010;113(2):482-495. DOI:10.1097/ALN.0b013e3181e08e97 [ Links ]
17. Shander A, van Aken H, Colomina MJ, et al. Patient blood management in Europe. Br J Anaesth 2012;109(1):55-68. DOI:10.1093/bja/aes139 [ Links ]
 Correspondence:
Correspondence:
G M Davison
davisong@cput.ac.za
Accepted 31 January 2016.














