Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.106 n.8 Pretoria Aug. 2016
http://dx.doi.org/10.7196/samj.2016.v106i8.10909
IN PRACTICE
CASE REPORT
Fatal encephalopathy complicating persistent vomiting in pregnancy: Importance of clinical awareness on the part of healthcare professionals
N C NgeneI; J MoodleyII
IMBBS, Dip Obst (SA), Dip HIV Man (SA), MMed (Fam Med), FCOG (SA), MMed (O&G); Department of Obstetrics and Gynaecology, School of Clinical Medicine, College of Health Sciences, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
IIMB ChB, FCOG (SA), FRCOG (UK), MD; Department of Obstetrics and Gynaecology, School of Clinical Medicine, College of Health Sciences, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
ABSTRACT
Women with persistent vomiting during pregnancy need early referral to appropriate health facilities. Delayed referral and inappropriate management may lead to metabolic encephalopathy from a variety of causes, including electrolyte derangements or thiamine deficiency (Wernicke's encephalopathy) (WE). We present a case of persistent vomiting in pregnancy in which there was delayed referral, inappropriate treatment and failure to associate neurological signs such as terminal neck stiffness with WE, resulting in poor fetomaternal outcomes. In this report, we discuss the following lessons: (i) the need for early transfer of a patient with persistent vomiting and enigmatic clinical features to a higher healthcare facility; (ii) failure to associate neurological signs with complications of hyperemesis gravidarum/WE; ( iii) lack of thiamine supplementation; and (iv) the advantages of magnetic resonance imaging over a computed tomography scan in the diagnosis of WE.
Hyperemesis gravidarum (HEG) is persistent vomiting in pregnancy that results in dehydration, electrolyte imbalance, ketosis and loss of more than 5% of prepregnancy weight or 3 kg.[1,2] HEG resulted in five in-hospital maternal deaths in South Africa between 2011 and 2013.[3] Because vomiting and nausea are the most common symptoms in pregnancy, affecting 50 - 90% of mothers,[1] some cases of vomiting are erroneously considered to be minor ailments. To assess the severity of vomiting and identify patients with HEG, the PUQE (Pregnancy-Unique Quantification of Emesis and Nausea) scoring system may be used.[4-6] HEG may result in neurological complications such as Wernicke's encephalopathy (WE), Korsakoff syndrome and osmotic demyelination (central pontine myelinolysis).[2,7,8] Wernicke's encephalopathy is an acute thiamine deficiency classically characterised by the triad of eye signs, an altered mental state and ataxia.[9] The prevalence of WE among alcoholics and non-alcoholics is 12.5% and 0.04 - 0.13%, respectively.[10]
We report a case in which non-provision of appropriate medical care to a patient with persistent HEG resulted in a fatal metabolic encephalopathy with neurological signs probably in keeping with a diagnosis of WE. The gaps in management are discussed so as to provide clinical lessons to all medical practitioners.
Case report
A 28-year-old woman, gravida 3, para 2, who had had two previous normal vaginal births, presented to a district hospital (DH) at 6 weeks' gestation with a history of persistent vomiting. She was diagnosed as having HEG, admitted and treated with an antiemetic, metoclopramide, for 6 days. She was not alcoholic. At 8 weeks' gestation, she was readmitted to the same hospital with HEG and again treated with metoclopramide and intravenous (IV) fluids for 7 days. During this admission, the medical officer managing the patient obtained advice from a doctor at a regional hospital (RH). They agreed that the patient should be reviewed in the RH in 9 days' time. The patient was not transferred on the agreed date for unknown reasons. At 11 weeks' gestation, she presented to the DH again and was referred to the regional facility. The serum electrolytes were not assessed at the DH.
When seen in the emergency obstetric unit at the RH, the patient had persistent vomiting, headache, photophobia, generalised body weakness and dehydration. Physical examination showed a Glasgow Coma Score (GCS) of 14 (motor response 5, eye opening 5, verbal response 4), abducent nerve palsy, terminal neck stiffness, a blood pressure of 102/79 mmHg, a pulse rate of 90 bpm and a temperature of 35.3oC. The serum sodium level was 146 mmol/L and the potassium level 2.5 mmol/L. She was reviewed by the internal medicine team, who made a provisional diagnosis of meningitis, prescribed ceftriazone and requested a computed tomography (CT) brain scan prior to performing a lumbar puncture.
On the 3rd day after admission to the RH, the patient was found to have renal impairment (serum creatinine level 435 μmol/L), hypokal-aemia, horizontal nystagmus and an offensive vaginal discharge. She was resuscitated with a normal saline infusion and potassium replacement therapy. On the 7th day, the CT brain scan showed no abnormalities; the planned lumbar puncture was performed, and analysis showed the cerebrospinal fluid (CSF) to be normal. At this stage, the beta human chorionic gonadotrophin (hCG) level was 71 109 IU/L, the blood urea nitrogen (BUN) level had improved from 27.5 to 3.1 mmol/L, the serum creatinine level had decreased from 435 to 41 μmol/L and the potassium level had increased from 1.8 to 2.8 mmol/L. An HIV test was negative, and thyroid dysfunction, malaria, autoimmune disorders and urinary tract infection were excluded. An ultrasound scan of the uterus revealed a live fetus of ~12 weeks' gestational age with no gross abnormalities and a normal placenta. The hCG levels were in keeping with the gestational age.
On the 9th day after admission, the patient was still vomiting and had a GCS of 8 (motor response 3, eye opening 3, verbal response 2), hypernatraemia (sodium level 164 mmol/L), hypokalaemia (potassium level 3.1 mmol/L), hypomagnesaemia (magnesium level 0.51 mmol/L) and a blood glucose level of 5.3 mmol/L. She was not polyuric. The clotting profiles were all within normal limits, and a chest radiograph and liver function tests did not show any abnormality. Thromboprophylaxis was commenced and correction of electrolyte imbalance was continued. Among the IV fluids administered during this period was 5% dextrose. A repeat obstetric scan revealed intrauterine death of the fetus.
The patient was subsequently admitted to the intensive care unit (ICU) because of inability to correct her electrolyte imbalance, especially the hypernatraemia. She received the following IV fluids in the ICU: magnesium sulphate, potassium phosphate, 5% dextrose infusion, and 0.45% saline mixed with 5% dextrose. The sodium level decreased from 164 to 158 mmol/L over a 3-day period. Because of concern about possible chorioamnionitis, misoprostol was administered to expel the products of the conception. The patient later had manual vacuum aspiration for an incomplete miscarriage. She subsequently developed respiratory failure and was mechanically ventilated.
On day 3 after ICU admission (day 13 post admission), the patient's condition in the previous 24 hours suggested that recovery was unlikely. The clinical conditions were: fixed and dilated pupils, no corneal reflex, GCS 2T, no response to pain stimulus and inability to trigger the ventilator. The ventilator was switched off after informed consent had been obtained from the patient's family, and she died. WE was thought to be the most probable cause of death, based on the presence of a metabolic encephalopathy with transient abducent nerve palsy and nystagmus in the context of prolonged vomiting. An autopsy was not performed.
Discussion
The management of HEG involves resuscitation, identification and treatment of any cause of the vomiting,[11] correction of electrolyte imbalance, symptomatic support such as rehydration, administration of antiemetics, thiamine supplementation, and nutritional as well as psychological support. It is not certain why the serum electrolytes were not assessed in the DH despite the availability of a functional laboratory. Health professionals must recognise the need to correct electrolyte imbalance and fully resuscitate pregnant women with a history of persistent vomiting. The patient was also managed in a standard hospital ward for some days. In such cases, correction of electrolyte imbalance must be carried out in a high-care area or an ICU setting. Persistent vomiting causes hyponatraemia, dehydration, increased thirst and prerenal impairment. Inadequate resuscitation and poor oral intake in our patient, who had a low GCS, may have caused the hypernatraemia. The return of the BUN and serum creatinine to normal levels following fluid therapy was consistent with prerenal failure. Rapid correction of hypernatraemia may lead to central myelinosis, and it is an alternative cause of neurological deterioration. In our patient, the correction of hypernatraemia was gradual, but not resolved prior to death. Early referral to an ICU or a high-care area is certainly recommended in cases such as ours. Acquisition of such knowledge on maternal resuscitation should begin during undergraduate education and continue after qualification by taking part in continuing education programmes dealing with obstetric emergencies, such as the Essential Steps in the Management of Obstetric Emergencies training or other similar programmes for medical practitioners.
Delayed arrival of the patient to the RH affected the outcome. Such a delay may be preventable if healthcare workers endeavour to transfer patients with non-remitting/enigmatic clinical features early enough to a higher level of care or seek appropriate advice from specialists. It may also be preventable if dedicated health workers are assigned to keep track of referred patients to ensure that they are reviewed at the referral centre.
An acute confusion state (encephalopathy) is a medical emergency that requires structured evaluation. In an encephalopathic patient, normal findings on brain imaging and CSF analysis in the absence of head trauma, recent seizures, sepsis or cardiorespiratory instability suggest metabolic encephalopathy. Causes include electrolyte and glucose abnormalities, vitamin deficiencies, and drug or alcohol withdrawal. In this case, diagnostic considerations were not expanded to include vitamin deficiencies in a patient who was unable to eat. In a previous report, loss of appetite and persistent vomiting were associated symptoms in a case of WE resulting from gastroparesis after a partial antrectomy.[12]
The body's thiamine reserve is depleted in HEG and WE, especially in tissues with a high metabolic rate such as the brain.[13] It is therefore recommended that serum thiamine be assessed and supplemented.[9] Given that the diagnosis of WE was not considered, thiamine was not administered. Furthermore, the use of dextrose-containing IV fluid could have worsened the neurological condition, as glucose infusion precipitates WE in patients who are thiamine depleted.[9] The protocol in the RH recommends against routine use of dextrose-containing fluid at the inception of management in HEG. This is regardless of a research finding that suggests that the administration of dextrose-containing IV fluids may not cause harm.[14] Nonetheless, a recent case series supports thiamine therapy before administration of glucose in any patient with altered consciousness of unknown causation.[15] To ensure appropriate management of WE or persistent HEG, a neurologist or an experienced medical practitioner should be involved early on. In a pregnant woman with persistent vomiting, dehydration and neurological signs, health professionals must consider WE. Since assessment of serum thia-mine levels is not routinely available, the diagnosis of WE can be made clinically by demonstrating response to thiamine supplementation.
Where facilities exist, patients with persistent vomiting may need magnetic resonance imaging (MRI) for evaluation. The MRI features of WE include hypersignal intensity at the thalamus.[12,13] A CT scan of the brain is not a reliable diagnostic test for WE,[9] and use of a CT scan of the brain to evaluate a patient with prolonged vomiting in pregnancy may therefore delay the diagnosis of WE. An MRI scan of the brain may reveal complications such as central pontine myelinolysis. Its use is also important in atypical cases of acute nonalcoholic WE.[12,16] Although an MRI scan was not performed, the patient did not have pseudobulbar paralysis or spastic quadriparesis, which are classic features of myelinolysis[7]
Conclusion
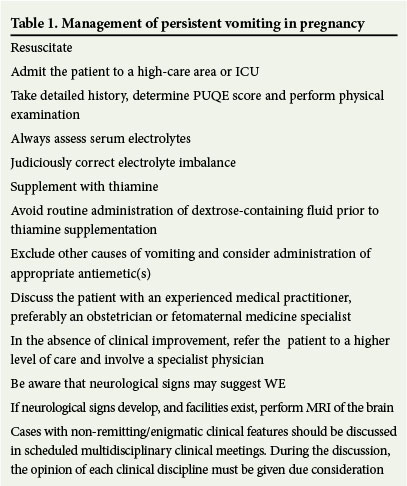
The management of HEG (Table 1) requires prompt, proper resuscitation and exclusion of other causes of vomiting. In a DH, this will mean obtaining advice from a specialist and timely referral; investigations must include a full blood count, urine dipstick testing, urine culture, blood glucose, liver function tests, hCG levels, obstetric ultrasound, thyroid function tests, serum urea, creatinine and electrolytes. Where the facilities exist, assessment of serum thiamine and evaluation of the brain with an MRI are valuable if there is an encephalopathy. Given the poor prognosis associated with undiagnosed WE, we strongly recommend routine thiamine supplementation in patients with persistent vomiting in pregnancy.
References
1. Jarvis S, Nelson-Piercy C. Management of nausea and vomiting in pregnancy. BMJ 2011;324:d3606 DOI:10.1136/bmj.d3606 [ Links ]
2. Sonkusare S. The clinical management of hyperemesis gravidarum. Arch Gynecol Obstet 2011;283(6):1183-1192. DOI:10.1007/s00404-011-1877-y [ Links ]
3. National Committee on the Confidential Enquiries into Maternal Deaths. Saving Mothers 2011 - 2013: Sixth report on the confidential enquiries into maternal deaths in South Africa. Pretoria: National Department of Health, 2015. http://www.kznhealth.gov.za/mcwh/Maternal/Saving-Mothers-2011-2013-short-report.pdf (accessed 12 July 2015). [ Links ]
4. Birkeland E, Stokke G, Tangvik RJ, et al Norwegian PUQE (Pregnancy-Unique Quantification of Emesis and Nausea) identifies patients with hyperemesis gravidarum and poor nutritional intake: A prospective cohort validation study. PLoS One 2015;10(4):e0119962. DOI:10.1371/journalpone.0119962 [ Links ]
5. Ebrahimi N, Maltepe C, Bournissen FG, Koren G. Nausea and vomiting of pregnancy: Using the 24-hour Pregnancy-Unique Quantification of Emesis (PUQE-24) scale. J Obstet Gynaecol Can 2009;31(9):803-807. DOI:10.1016/s1701-2163(16)34298-0 [ Links ]
6. Koren G, Boskovic R, Hard M, Maltepe C, Navioz Y, Einarson A. Motherisk-PUQE (Pregnancy-Unique Quantification of Emesis and Nausea) scoring system for nausea and vomiting of pregnancy. Am J Obstet Gynecol 2002;186(5, Suppl 2):S228-S231. DOI:10.1067/mob.2002.123054 [ Links ]
7. Zara G, Codemo V, Palmieri A, et al. Neurological complications in hyperemesis gravidarum. Neurol Sci 2012;33(1):133-135. DOI:10.1007/s10072-011-0660-y [ Links ]
8. Kotha VK, de Souza A. Wernicke's encephalopathy following hyperemesis gravidarum. A report of three cases. Neuroradiol J 2013;26(1):35-40. DOI:10.1177/197140091302600106 [ Links ]
9. Galvin R, Brathen G, Ivashynka A, Hillbom M, Tanasescu R, Leone MA. EFNS guidelines for diagnosis, therapy and prevention of Wernicke encephalopathy. Eur J Neurol 2010;17(10):1408-1418. DOI:10.1111/j.1468-1331.2010.03153.x [ Links ]
10. Kantor S, Prakash S, Chandwani J, Gokhale A, Sarma K, Albahrani MJ. Wernicke's encephalopathy following hyperemesis gravidarum. Indian J Crit Care Med 2014;18(3):164-166. DOI:10.4103/0972-5229.128706 [ Links ]
11. Jueckstock JK, Kaestner R, Mylonas I. Managing hyperemesis gravidarum: A multimodal challenge. BMC Med 2010;8:46. DOI:10.1186/1741-7015-8-46 [ Links ]
12. Ganie NS, Janse van Rensburg E. Wernicke's encephalopathy as a complication of gastroparesis after emergency partial antrectomy. S Afr Med J 2015;105(2):157. DOI:10.7196/SAMJ.9271 [ Links ]
13. Sutamnartpong P, Muengtaweepongsa S, Kulkantrakorn K. Wernicke's encephalopathy and central pontine myelinolysis in hyperemesis gravidarum. J Neurosci Rural Pract 2013;4(1):39-41. DOI:10.4103/0976-3147.105608 [ Links ]
14. Tan PC, Norazilah MJ, Omar SZ. Dextrose saline compared with normal saline rehydration of hyperemesis gravidarum: A randomized controlled trial. Obstet Gynecol 2013;121(2):291-298. DOI:10.1097/aog.0b013e31827c5e99 [ Links ]
15. Antel K, Singh N, Chisholm B, Heckmann JM. Encephalopathy after persistent vomiting: Three cases of non-alcohol-related Wernicke's encephalopathy. S Afr Med J 2015;105(6):442-443. DOI:10.7196/SAMJ.9299 [ Links ]
16. Elefante A, Puoti G, Senese R, et al. Non-alcoholic acute Wernicke's encephalopathy: Role of MRI in non typical cases. Eur J Radiol 2012;81(12):4009-4104. DOI:10.1016/j.ejrad.2012.08.006 [ Links ]
 Correspondence:
Correspondence:
N C Ngene
ngenenc@gmail.com
Accepted 13 April 2016.














