Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.106 n.8 Pretoria Aug. 2016
http://dx.doi.org/10.7196/samj.2016.v106i8.11042
IN PRACTICE
COCHRANE CORNER
Antifibrinolytic drugs for acute traumatic injury
M McCaulI; T KredoII
IMSc (Clin Epi); Centre for Evidence-Based Health Care, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
IIMB ChB, MMed (Clin Pharm), Dip HIV Man (SA); Cochrane South Africa, South African Medical Research Council, Cape Town, South Africa
ABSTRACT
In South Africa, trauma is a major concern, with violence and road traffic accidents being the fifth and seventh leading causes of death, respectively. Antifibrinolytic agents have been used in trauma and major surgery to prevent fibrinolysis and reduce blood loss. We highlight an updated Cochrane review investigating the effect of antifibrinolytic drugs in patients with acute traumatic injury. The review authors conducted comprehensive literature searches in January 2015 with regard to all randomised controlled trials comparing antifibrinolytic agents after acute traumatic injury. Three randomised controlled trials, of which two (n=20 451) assessed the effect of tranexamic acid (TXA), were included. The authors concluded that TXA safely reduces mortality in trauma with bleeding without increasing the risk of adverse events. TXA should be administered as early as possible, and within 3 hours of injury. There is still uncertainty with regard to the effect of TXA on patients with traumatic brain injury; however, ongoing randomised controlled trials should shed more light on this.
Injuries are responsible for more deaths per year than HIV/AIDS, tuberculosis and malaria combined.[1] Furthermore, each year ~4 million people die as a result of traumatic injuries and violence worldwide. In South Africa, trauma is a major concern, with violence and road traffic accidents being the fifth and seventh leading causes of death respectively.[2] Antifibrinolytic agents have been used in trauma and major surgery to prevent fibrinolysis and reduce blood loss.
We summarise the evidence from an updated Cochrane review[3] investigating the effect of antifibrinolytic drugs in patients with acute traumatic injury.
Methods
The review authors conducted comprehensive literature searches in January 2015. All randomised controlled trials comparing anti-fibrinolytic agents (aprotinin, tranexamic acid (TXA), epsilon aminocaproic acid and amino-methylbenzoic acid) administered after acute traumatic injury were included. No restrictions were made with regard to language, date or publication status. Standard Cochrane methods for independent data screening and eligibility assessment, data extraction and risk-of-bias evaluation were followed.
Results
Three randomised controlled trials were included, of which two (n=20 451) assessed the effect of TXA. The Clinical Randomisation of an Antifibrinolytic in Significant Haemorrhage (CRASH)-2 trial (n=20 211),[4] the larger of the two, was conducted in 40 countries and included patients with a variety of trauma types; the other specifically investigated patients with traumatic brain injury (TBI) (n=240). The third trial assessed aprotinin in participants with major bony trauma and shock. All three trials[3] provided data for meta-analysis.
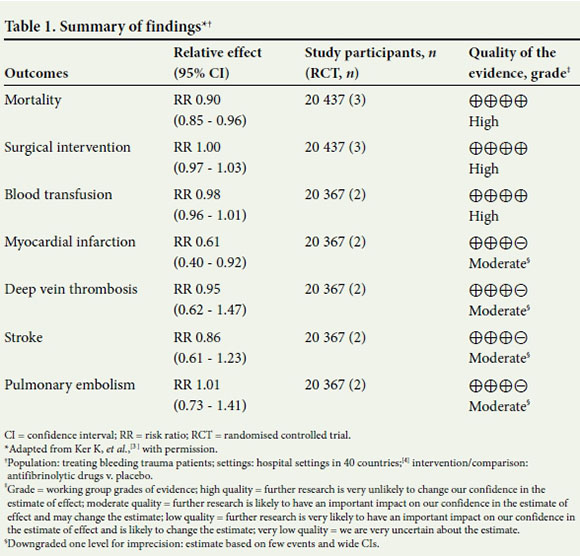
Antifibrinolytics reduced the risk of death by 10% (relative risk (RR) 0.90, 95% confidence interval (CI) 0.85 - 0.96; three trials, high-quality evidence) compared with placebo. It should be noted that this estimate was largely based on the results of CRASH-2, a methodologically rigorously conducted trial.
The authors found that antifibrinolytics do not have adverse effects on the risk of vascular occlusive events, such as deep vein thrombosis, stroke or pulmonary embolism (moderate-quality evidence). TXA reduced the risk of myocardial infarction by 39% (RR 0.61, 95% CI 0.40 - 0.92; two trials, moderate-quality evidence). Further results are shown in Table 1.
The TBI subgroup of patients who received TXA may be less likely to die (all-cause mortality) compared with patients who received placebo (RR 0.63, 95% CI 0.40 - 0.99; two trials, n=510, low-quality evidence); the low number of events and relative imprecision resulted in the downgrading of overall confidence in the results. Stronger evidence exists for the reduced risk of volume of intracranial bleeding with TXA in TBI patients compared with placebo (RR 0.75, 95% CI 0.58 -0.98; subgroup n=478, high-quality evidence).
Conclusion
The review authors concluded that TXA safely reduces mortality in trauma with bleeding, without increasing the risk of adverse events. TXA should be given as early as possible and within 3 hours of injury. There is still uncertainty with regard to the effect of TXA on patients with TBI; however, ongoing randomised controlled trials should shed more light on this. Evidence from this review has been incorporated into trauma clinical practice guidelines[5] by the National Institute for Health and Care Excellence (NICE) in the UK, which has made recommendations for TXA use in both in-hospital and prehospital settings.
References
1. World Health Organization. Injuries and Violence: The Facts. Geneva: WHO, 2010:2-18. http://scholar.google.com/scholar?hl=en&btnG=Search&q=intitle:Injuries+and+Violence:+The+Facts#0 (accessed 22 June 2016). [ Links ]
2. Naghavi M, Wang H, Lozano R, et al. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990 - 2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;385(9963):117-171. DOI:10.1016/S0140-6736(14)61682-2 [ Links ]
3. Ker K, Roberts I, Shakur H, Coats T. Antifibrinolytic drugs for acute traumatic injury. Cochrane Database Syst Rev 2015;(5):CD004896. DOI:10.1002/14651858.CD004896.pub4. [ Links ]
4. CRASH-2. The use of tranexamic acid. http://www.crash2.lshtm.ac.uk/ (accessed 27 June 2016). [ Links ]
5. National Institute for Health and Care Excellence. Major Trauma: Assessment and Initial Management. UK: NICE, 2016. https://www.nice.org.uk (accessed 22 June 2016). [ Links ]
 Correspondence:
Correspondence:
M McCaul
mmccaul@sun.ac.za
Accepted 30 May 2016.














