Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.106 no.6 Pretoria jun. 2016
http://dx.doi.org/10.7196/samj.2016.v106i6.10347
RESEARCH
Psoriatic arthritis: An assessment of clinical, biochemical and radiological features in a single-centre South African cohort
A B MaharajI, II; M RajkaranIII; J GovenderIV; K MaharajV; N de VriesVI; P P TakVI
IMBBS, H Dip Int Med (SA), FCP (SA), Cert Rheumatol (SA); Department of Internal Medicine, Prince Mshiyeni Memorial Hospital and School of Clinical Medicine, College of Health Sciences, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
IIMBBS, H Dip Int Med (SA), FCP (SA), Cert Rheumatol (SA); Division of Clinical Immunology and Rheumatology, Academic Medical Center, University of Amsterdam, Netherlands
IIIMB BCh, FCP (SA); Cert Rheumatol (SA); Department of Internal Medicine, Prince Mshiyeni Memorial Hospital and School of Clinical Medicine, College of Health Sciences, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
IVBSc Hons, MB ChB; Cert Rheumatol (SA); Department of Internal Medicine, Prince Mshiyeni Memorial Hospital and School of Clinical Medicine, College of Health Sciences, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
VMB ChB, FCP (SA); Cert Rheumatol (SA); Department of Internal Medicine, Prince Mshiyeni Memorial Hospital and School of Clinical Medicine, College of Health Sciences, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
VIMD, PhD; Cert Rheumatol (SA); Division of Clinical Immunology and Rheumatology, Academic Medical Center, University of Amsterdam, Netherlands
ABSTRACT
BACKGROUND. Although psoriatic arthritis (PsA) is a well-documented clinical entity, epidemiological, clinical and radiological studies of South African (SA) patients are scarce.
OBJECTIVES. To assess clinical, biochemical and radiological features in a single-centre SA cohort.
METHODS. We conducted a prospective assessment of the clinical, biochemical and radiological features of 384 consecutive patients with PsA seen at the rheumatology clinic at Prince Mshiyeni Memorial Hospital, Durban, SA, between January 2007 and December 2013. Patients were assessed at enrolment and 6 months after enrolment. They were classified into five groups as described by Moll and Wright, being entered into the group that best described the clinical manifestations. Clinicopathological characteristics recorded at enrolment were age at the time of examination, racial background, personal and family medical history, age and symptoms at the onset of PsA, pattern of joint involvement, joint pain, and the relationship between joint pain and the onset of PsA.
RESULTS. Of the patients, 59.1% had a polyarticular presentation indistinguishable from rheumatoid arthritis, 19.0% had distal interphalangeal involvement, 9.1% had spondyloarthropathy, 11.9% had oligoarthritis and 0.9% had arthritis mutilans. The epidemiological trends (male/female ratio 1.45:1, mean age at onset of arthritis 50.2 (standard deviation 11.8) years, female preponderance in the polyarticular group and male preponderance in the spondyloarthropathy and oligoarticular groups) were similar to trends published elsewhere. A notable characteristic of our cohort was the complete absence of black South Africans with PsA.
CONCLUSIONS. The complete absence of black South Africans with PsA is interesting. We anticipate that our findings will prompt genetic studies to isolate both protective and susceptibility genes for further elucidating PsA.
Although psoriatic arthritis (PsA) is a well-documented clinical entity,[1] epidemiological, clinical and radiological studies of South African (SA) patients are scarce. There are, in fact, no published data regarding the prevalence and incidence of PsA in the SA population. In 1973, Moll and Wright[1] defined PsA as an inflammatory arthritis associated with psoriasis in the absence of rheumatoid factor (RF), and it was not until 2006 that the ClASsification criteria for Psoriatic ARthritis (CASPAR) were introduced for the purpose of diagnosis.[2] The long-recognised Moll and Wright criteria[1] are widely accepted diagnostic criteria that divide PsA into five different types, based on the patterns of joint involvement: (i) polyarticular; (ii) distal interphalangeal (DIP); (iii) spondyloarthropathy; (iv) oligoarticular; and (v) arthritis mutilans.[1] There are some patients in the reported literature who presented with overlapping symptoms and therefore cannot be classified into a specific group.[1]
PsA is a heterogeneous disease associated with inflammatory arthritis, enthesopathies and new bone formation together with erosive arthropathy.[3,4] The absence of RF is well documented in patients with PsA.[5] For many years, PsA was considered a less aggressive disease than rheumatoid arthritis; however, recent studies have revealed severe erosions and ankylosis in patients with PsA.[6-8] We examined the clinical, biochemical and radiological features of PsA in a cohort of 384 SA patients.
Objectives
To document the features of PsA in SA patients and determine the similarities and differences between our patients and those reported globally.
Methods
Patients
Our study, which was approved by the Pharma-Ethics Independent Research Committee of South Africa (Ref. No. 1309560), included 384 consecutive patients diagnosed with PsA at the rheumatology clinic at Prince Mshiyeni Memorial Hospital (PMMH), Durban, SA, between January 2007 and December 2013. The duration of disease symptoms varied between patients. PsA was diagnosed by one of several consultants with a special interest in the disorder, and the diagnoses were based on the Moll and Wright criteria.[1] RF positivity is well documented in a small proportion of healthy individuals, and the prevalence increases with age.[9] Nevertheless, patients who were RF-positive were included in the study if they fulfilled the Moll and Wright diagnostic criteria.[1,10] Patients with rheumatoid arthritis, osteoarthritis or other mechanical joint disease, reactive arthritis, and other seronegative arthritides or crystal-associated arthropathy were excluded, as were those with evidence of collagen vascular disease. Patients with PsA with secondary mechanical arthropathies were included. All the patients in the study provided written informed consent to participate.
Assessment of patient and disease characteristics
Patients' clinicopathological characteristics, determined at the time of initial examination, were recorded. These included age at the time of examination, racial group, personal and family medical history, age and symptoms at the onset of PsA, pattern of joint involvement, joint pain and the relationship between joint pain and the onset of PsA. Any extra-articular manifestations were also recorded. Peripheral joint involvement was assessed using the 68/66 tender/swollen joint count. The evaluation of axial involvement included the occiput-to-wall distance, tragus-to-wall distance and goniometric assessment of the range of movement of the cervical spine. Mobility of the lumbar spine was assessed based on a modified Schober test, fingertip-to-floor distance and lateral flexion of the lumbar spine. Thoracic spine movement was assessed based on chest expansion. The sacroiliac joints were examined using Patrick's FABER (Flexion, ABduction, and External Rotation) test, anterior posterior pelvic pressure over the anterior superior iliac spine, lateral pelvic compression, direct pressure over the sacroiliac joints and Gaenslen's test (Table 1).[11] Treatment was begun at enrolment, and treatment strategies were recorded.
At enrolment, a full blood count was done and the erythrocyte sedimentation rate (ESR, Westergren), C-reactive protein (CRP), urea and electrolytes, serum uric acid, serum lipids and plasma glucose concentration were measured. The presence of anti-cyclic citrullinated peptide (anti-CCP) antibodies was detected using an enzyme-linked immunosorbent assay, and antinuclear antibodies (ANAs) were detected by immunofluorescence. HLA-B27 typing was performed in all patients, and liver function tests were done.
Plain radiographs of the hands, feet, pelvis and lumbar spine were obtained on all patients at enrolment. The radiographs were read by one of several radiologists with an interest in inflammatory arthritis and were evaluated for erosions and new bone formation. The sacroiliac joints were assessed and described based on the modified New York criteria.[12]
At enrolment, patients were categorised into one of five clinical groups according to the Moll and Wright PsA subtypes.[1] Categorisation was based on both clinical and radiographic findings.
Results
Overall patient characteristics
Of the 384 patients in the study, 157 were women and 227 were men (male/female ratio 1.45:1). Most patients were referred to the clinic by a general practitioner, family practitioner or dermatologist, and a small percentage of patients (5.1%) were self-referred. Two hundred and forty-seven of the patients were of Indian descent, 135 were of European descent, and 2 were of mixed descent. Ninety-three (24.2 %) of the patients had a family history of psoriasis or PsA. The mean age at the onset of psoriasis was 38.4 (standard deviation (SD) 9.3) years, and the mean age at the onset of arthritis was 50.2 (SD 11.8) years. In 341 patients (88.8%) the psoriasis preceded the arthritis. Six patients had nail changes without skin changes, and their disease was characterised by DIP involvement. Five patients had inflammatory arthritis with dactylitis and enthesopathy and a family history of psoriasis, but no current evidence of psoriasis. Five patients had uveitis as the only extra-articular manifestation, and 3 of these 5 patients were HLA-B27-positive. No other extra-articular manifestations were noted in our patient cohort.
Joint distribution
All five Moll and Wright PsA subtypes were represented in our study (Table 2), with polyarthritis, indistinguishable from rheumatoid arthritis, found most often (59.1% of the 352 patients in whom subtypes did not overlap). The next most common subtype was the DIP subtype (19.0%) followed by the oligoarticular type (11.9%); spondyloarthropathy accounted for 9.1% of the cases and arthritis mutilans for 0.9%.
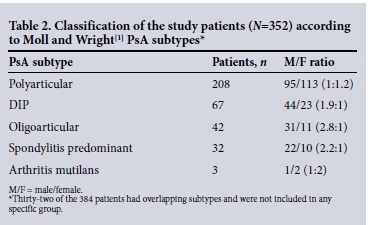
Among the patients in the polyarticular PsA group, 81.7% (170/208) were found to have metacarpophalangeal (MCP) involvement, 68.3% (142/208) radiocarpal involvement and 68.3% (142/208) metatarsophalangeal (MTP) involvement (Table 3). Among patients in the oligoarticular PsA group, the knees (52.4%) and ankles (35.7%) were most frequently involved. In nine patients in this group, asymmetrical oligoarticular involvement of the lower limbs was associated with sacroiliitis. Only three patients had severe arthritis mutilans. In all three, the arthritis mutilans involved digits of the upper and lower limbs. Female sex was predominant in the polyarthritis group (113/208 (54.3%) women v. 95/208 (45.7%) men) and male sex was predominant in the spondyloarthritis group (22/32 (68.7%) men v. 10/32 (31.3%) women) (Table 2). There was also a male preponderance in the oligoarticular group, with a male/female ratio of 2.8:1. Fingernail changes, including pitting of the nails, onycholysis and nail dystrophy, were observed in 72.1% (277/384) of the patients.

Laboratory data
ESR, CRP, RF and anti-CCP measurements at enrolment are shown in Table 4. An elevated ESR was noted in only 99/384 patients (25.8%). The ESR elevation was greater in the polyarticular group than in the spondyloarthropathy group (mean 46 mm/h v. 38 mm/h). However, CRP was elevated in 243 (63.3%) of patients, to a mean concentration of 15.3 mg/L (normal range 0 - 8). After 6 months of disease-modifying antirheumatic drug (DMARD) therapy, the mean CRP level dropped to 7.1 mg/L. Results of liver function tests were normal, with the exception of hyperglobulinaemia in all patients. Nineteen patients (4.9%) tested positive for RF and 15 (3.9%) for anti-CCP antibodies. Six patients tested positive for ANAs; however, none of them fulfilled the American College of Rheumatology criteria for a diagnosis of systemic lupus erythematosus (SLE).

HLA-B27 positivity was noted in 57 patients (14.8% ). Twenty-eight of these patients had axial involvement, and 29 patients with oligo- or polyarticular disease exhibited HLA-B27 positivity. Of the patients who were positive for HLA-B27, 35 (61.4%) were of European descent, only 22 (38.6%) being of Indian origin.
Radiological assessment
All patients underwent radiological examination of the hands, feet, sacroiliac joints and lumbar spine at enrolment. Sacroiliitis of grade 2 or above was noted in 22 of the 32 patients with spondyloarthropathy (14 men v. 8 women). Five patients had syndesmophytes, which were asymmetrical and unilateral. The radiographic features of peripheral joint involvement included soft-tissue swelling, erosion, joint space narrowing, ankylosis and new bone formation.
Treatment
Treatment was assessed at 6 months. All the patients were DMARD naive at enrolment. Of the total of 384 patients, 256 (66.6%) received methotrexate monotherapy at an average dose of 17.5 mg/week (range 7.5 - 25). Disease activity remained low in these patients, with a mean simplified disease activity index of 7.6. Seventy-three patients (19.0%) were given a combination of methotrexate and sulfasalazine, and 45 (11.7%) triple therapy with methotrexate, sulfasalazine and leflunomide. Only 10 patients received biologicals, and none received hydroxychloroquine or chloroquine. Corticosteroids were only used intra-articularly for acute flare-ups.
Discussion
To the best of our knowledge, this is the first study to explore the clinical, laboratory and radiological characteristics of a fairly large cohort of SA PsA patients. Three hundred and eighty-four patients diagnosed with PsA were included, of whom 352 could be classified according to the Moll and Wright criteria.[1] The epidemiological findings in our study (male/female ratio 1.45:1, mean age at onset of arthritis 50.2 (SD 11.8) years, female preponderance in the polyarticular group and male preponderance in the spondyloarthropathy and oligoarticular groups) are similar to trends published elsewhere.[13] Other classification criteria have also been found to be similar when applied to an SA cohort.[14] One notable characteristic of our patient group was the complete absence of black South Africans with PsA. PMMH is a large regional hospital to the south of Durban and is the only referral rheumatology centre in this region. The catchment population is 1.6 million (82.4% black Africans), and 92.3% of hospital outpatients are black Africans. At the rheumatology clinic, 63.5% of patients are black Africans presenting with various other rheumatological problems including rheumatoid arthritis, SLE, osteoarthritis and HIV-associated arthropathy.[15] The racial distribution needs to be explored further. Whether black Africans with PsA would also be lacking in a larger patient group remains to be determined, but it appears that psoriasis/PsA may be absent in the black population. The reasons for this lack of susceptibility are not clear, but could be related to the low prevalence of HLA-B27 in this population. Psoriasis has been noted in the HIV-positive black population.
In most of our patients, the psoriasis developed before the arthritis. The distribution of joint involvement observed in our cohort was similar to distributions published elsewhere.[13]
The reason for the limited use of biological therapy in our patient group was that PsA is not well covered by medical insurance in SA. Medical insurance in SA does not reimburse PsA patients for biological therapy.
Conclusions
This study of the epidemiological, clinical and radiological features of a fairly large cohort of SA patients with PsA yielded data similar to results for other populations. The complete absence of black South Africans with PsA in our cohort may be related to the low prevalence of HLA-B27 in this population. There may be yet-to-be-identified protective genes in this population group. We anticipate that our findings will prompt genetic studies to isolate both protective and susceptibility genes for further elucidating PsA.
Acknowledgement. We thank Prof. V Chandran (University of Toronto and University Health Network and Mount Sinai Hospitals, Toronto, Canada) for all his assistance and guidance, as well as his input regarding the final manuscript.
References
1. Moll JM, Wright V. Psoriatic arthritis. Semin Arthritis Rheum 1973;3(1):55-78. DOI:10.1016/0049-0172(73)90035-8 [ Links ]
2. Taylor W, Gladman D, Helliwell P, et al. Classification criteria for psoriatic arthritis: Development of new criteria from a large international study. Arthritis Rheum 2006;54(8):2665-2673. DOI:10.1002/art.21972 [ Links ]
3. O'Neill T, Silman AJ. Psoriatic arthritis: Historical background and epidemiology. Baillieres Clin Rheumatol 1994;8(2):245-261. [ Links ]
4. Gladman DD. Clinical aspects of the spondyloarthropathies. Am J Med Sci 1998;316(4):234-238. [ Links ]
5. Punzi L, Podswiadek M, Oliviero F, et al. Laboratory findings in psoriatic arthritis. Reumatismo 2007;59(Suppl 1):52-55. DOI: 10.4081/reumatismo.2007.1s.52 [ Links ]
6. Gladman DD, Chandran V. Review of clinical registries of psoriatic arthritis: Lessons learned? Value for the future? Curr Rheumatol Rep 2011;13(4):346-352. DOI:10.1007/s11926-011-0182-x [ Links ]
7. McHugh NJ, Balachrishnan C, Jones SM. Progression of peripheral joint disease in psoriatic arthritis: A 5-yr prospective study. Rheumatology (Oxford) 2003;42(6):778-783. DOI:10.1093/rheumatology/keg217 [ Links ]
8. Schoellnast H, Deutschmann HA, Hermann J, et al. Psoriatic arthritis and rheumatoid arthritis: Findings in contrast-enhanced MRI. AJR Am J Roentgenol 2006;187(2):351-357. DOI:10.2214/ARJ.04.1798 [ Links ]
9. Simard JF, Holmqvist M. Rheumatoid factor positivity in the general population. BMJ 2012;345:e5841. DOI:10.1136/bmj.e5841 [ Links ]
10. Gladman DD, Shuckett R, Russell ML, et al. Psoriatic arthritis (PSA) - an analysis of 220 patients. Q J Med 1987;62(2):127-141. [ Links ]
11. Macrae IF, Wright V. Measurement of back movement. Ann Rheum Dis 1969;28(6):584-589. [ Links ]
12. Van der Linden S, Valkenburg HA, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis: A proposal for modification of the New York criteria. Arthritis Rheum 1984;27(4):361-368. DOI:10.1002/art.1780270401 [ Links ]
13. Gladman DD, Antoni C, Mease P, et al. Psoriatic arthritis: Epidemiology, clinical features, course, and outcome. Ann Rheum Dis 2005;64(Suppl 2):ii14-ii17. DOI:10.1136/ard.2004.032482 [ Links ]
14. Maharaj AB, Govender J, Maharaj K, et al. Summary of sensitivity and specificity for psoriatic arthritis in a South African cohort according to classification criteria. J Rheumatol 2015;42(6):960-962. DOI:10.3899/jrheum.141537 [ Links ]
15. Maharaj AB, Tak PP. Spondyloarthritis in African blacks. J Rheumatol 2015;42(1):139. DOI:10.3899/jrheum.141023 [ Links ]
 Correspondence:
Correspondence:
A B Maharaj
maharaja30@ukzn.ac.za
Accepted 2 December 2015.














