Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.106 n.5 Pretoria May. 2016
http://dx.doi.org/10.7196/samj.2016.v106i5.9867
IN PRACTICE
CASE REPORT
On your toes: Detecting mediastinal air on the chest radiograph in ecstasy abusers
M NaidooI; M GovindII
IFamily physician working as a head of clinical unit/lecturer for the Department of Family Medicine in the School of Nursing and Public Health, College of Health Sciences, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa, and the KZN Department of Health. His special interests include primary emergency care, and he has been involved with emergency care outreach using simulation-based teaching in the province of KZN for a number of years
IIRadiologist working as an MMed co-ordinator in the Department of Academic Clinical and Professional Practice in the School of Clinical Medicine at UKZN. She has an interest in medical education
ABSTRACT
Abnormal mediastinal air may be caused by inhalational illicit drug use subsequent to barotrauma resulting from coughing after deep inhalation and breath holding. It may also arise from oesophageal rupture due to retching after ingestion of the illicit drug. The history can alert the practitioner to this cause of chest pain. As chest radiographs are widely accessible and mediastinal air is easily recognisable, the chest radiograph should be included and carefully scrutinised in the diagnostic workup of chest pain in the recreational drug abuser. It is prudent to exclude oesophageal rupture, particularly in the setting of retching, before deciding on conservative and expectant management.
The 'club drug' known as ecstasy (3,4-methylenedioxymeth-amphetamine (MDMA)) has been reported to be involved in 1% of primary and 3% of secondary drug abuse in patients presenting to treatment facilities in Durban, South Africa.[1] The emergency room (ER) presentation of patients suffering from the effects of this drug poses a particular challenge, as ecstasy is often abused in conjunction with other agents.[1] We report the case of a 19-year-old man who presented with acute chest pain following drug ingestion.
Case report
A 19-year-old man presented to the ER at Wentworth Hospital, Durban, late at night. He reported central chest pain for 22 hours following the ingestion of alcohol and seven tablets of a drug called 'Mercedes' (a form of MDMA). There was no history of retching or vomiting. The patient was clinically stable on admission with a pulse of 95/min, a blood pressure of 138/98 mmHg and a respiratory rate of 20/min. He was alert but needed assistance with mobilising. Blood tests revealed a marginally elevated creatinine kinase cardiac fraction, but troponin-T levels were normal. Findings on electrocardiography were normal. A chest radiograph (CXR) was done and misinterpreted as normal. There was no known underlying lung pathology.
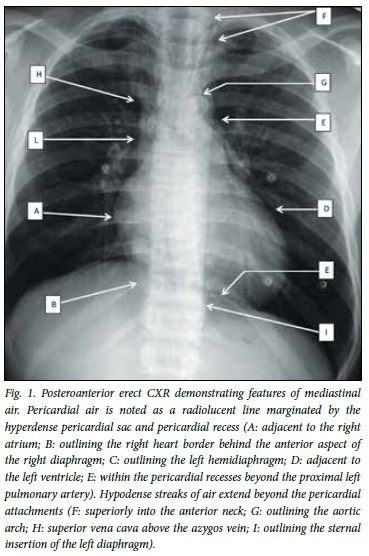
The patient was admitted to a general ward for observation. During the ward round the next day a pericardial friction rub was noted, but neck crepitus was not present. The initial CXR (Fig. 1) was reviewed and revealed mediastinal air (pneumomediastinum and pneumopericardium). On day 2 he remained stable but was referred to the cardiothoracic surgeons as a precaution. The CXR was repeated and an echocardiogram and contrast swallow were recommended. The repeat CXR demonstrated reduction in mediastinal air, and the echocardiogram was normal.
The patient was returned to a general ward in the hospital for observation. He was counselled by the social workers and made a full recovery within the week.
Discussion
Ecstasy may be inhaled as a powder or ingested as a tablet. Despite the two different modes of consumption, the underlying pathophysiology for mediastinal air in ecstasy abuse is barotrauma rather than a direct pharmacological mechanism.[3] Drug inhalation is associated with valsalva manoeuvres such as prolonged breath holding, coughing and physical exertion. These manoeuvres increase the intra-alveolar pressure causing spontaneous rupture of the alveoli, particularly in the scenario of airway inflammation, i.e. weakened alveolar integrity. As the interstitial pressure is relatively lower, the alveolar air tracks along the peribronchovascular spaces to reach the hilum and mediastinum. [4] In contrast, retching following drug ingestion can lead to rupture of the oesophagus and the direct introduction of air into the tissue planes of the mediastinum. Interstitial air can give rise to further complications by dissecting through tissue planes to extend into the potential spaces, causing secondary pneumopericardium and pneumothorax. [4] Careful examination of the CXR would assist in detecting mediastinal air and its complications. Importantly, the mechanism of drug consumption may indicate the causation of mediastinal air and therefore determine subsequent diagnostic workup.
Bakhos et al. [5] in their report on spontaneous pneumomediastinum noted that illicit drug use accounted for 24% of cases, and that 41% of all presentations of spontaneous pneumomediastinum occurred in individuals with no underlying lung pathology. They suggested a conservative approach to investigation and management, as the condition is usually benign and self-limiting. In an earlier case report, Levine et al.[6] recommended that rupture of the oesophagus be excluded before proceeding with conservative management. Similarly, Newcomb and Clark[7] recommended that a non-invasive contrasted computed tomography scan of the chest and water-soluble contrast swallow examination be included in the diagnostic work-up if there is a suspicion of oesophageal rupture. Two cases of spontaneous pneumomediastinum following ecstasy ingestion have been reported by Rezvani et al.,[8] but the pathophysiology was not described. We could not assign either mechanism of barotrauma to our case, as there was no history of deep inhalation, excessive coughing or retching.
The CXR
The CXR is an easily accessible imaging tool, and despite its limitations it can demonstrate mediastinal emphysema (pneumo-mediastinum and pneumopericardium) clearly as air contrasts well with the soft tissue of the mediastinum. Some of the pathognomonic features of mediastinal air on a plain CXR are shown in Fig. 1. Pneumomediastinum is seen as discontinuous hypodense streaks of air in the hyperdense mediastinal tissue. The air lies in the interstitial spaces and can streak upwards into the neck and the subcutaneous soft tissue of the axilla and chest, inferiorly into the retroperitoneum and beyond the anatomical attachments of the pericardium.[9] This air does not shift with change in patient positioning, as opposed to air in pericardial space, which alters with gravity.[9]
Other signs that suggest mediastinal air on the CXR include the 'continuous diaphragm sign' (air trapped posterior to the pericardium), 'Naclerio's V sign', which is formed by the junction of mediastinal air in the left lower mediastinum and extrapleural air adjacent to the left hemidiaphragm, the 'V sign' that is formed by the confluence of the superior margins of the brachiocephalic veins, the 'ring around artery sign' that results from air outlining the pulmonary artery and the main branches, the 'double bronchial wall sign' formed by air outlining the bronchi, air in the pulmonary ligament and irregular bilateral apical extrapleural air.[9] However, mediastinal air may be appreciated only on a lateral CXR as the hypolucent outline of the right pulmonary artery, aortic arch, ascending aorta, trachea and proximal bronchi. A more easily recognisable feature on the lateral CXR is the presence of retrosternal extrapleural air.[9]
Conclusion
Pneumomediastinum following MDMA use has been described as a fairly rare cause of chest pain. It is often associated with normal vital signs, and the air can be detected on the standard CXR. With the global and in particular the national trend of increasing drug abuse among teenagers and young adults, ER physicians need to be aware of this diagnosis as a complication, albeit rare, of inhalational illicit drug abuse and recognise its signs on the CXR.
The management of uncomplicated non-surgical mediastinal air is expectant observation. During this time the patient should be monitored for acute complications such as tension pneumopericardium and tension pneumothorax. Sometimes, as in the case described, the history may not suggest the diagnosis. Nevertheless, when there is a history of illicit drug use it is prudent to include the correct interpretation of a CXR in the diagnostic work-up.
References
1. Dada S, Pluddemann A, Parry C, et al. Monitoring alcohol and drug abuse trends in South Africa. SACENDU Res Br 2012;15(1):1-15. [ Links ]
2. Van Loggerenberg CJ. Emergency management of drug abuse in South Africa: Drug abuse remains both a global scourge and a significant social and medical problem in South Africa. CME 2012;30(11):409-413. [ Links ]
3. Harris R, Joseph A. Spontaneous pneumomediastinum? "Ecstasy': A hard pill to swallow. Aust N Z J Med 2000;30(3):401-403. DOI:10.1111/j.1445-5994.2000.tb00848.x [ Links ]
4. Macklin MT, Macklin CC. Malignant interstitial emphysema of the lungs and mediastinum as an important occult complication in many respiratory diseases and other conditions: An interpretation of the clinical literature in the light of laboratory experiment. Medicine 1944;23(4):281-358. [ Links ]
5. Bakhos CT, Pupovac SS, Ata A, Fantauzzi JP, Fabian T. Spontaneous pneumomediastinum: An extensive workup is not required. J Am Coll Surg 2014;219(4):713-717. DOI:10.1016/j.jamcollsurg.2014.06.001 [ Links ]
6. Levine AJ, Drew S, Rees GM. 'Ecstasy' induced pneumomediastinum. J R Soc Med 1993;86(4):232-233. [ Links ]
7. Newcomb AE, Clarke CP. Spontaneous pneumomediastinum: A benign curiosity or a significant problem? Chest J 2005;128(5):3298-3302. DOI:10.1378/chest.128.5.3298 [ Links ]
8. Rezvani K, Kurbaan A, Brenton D. Ecstasy induced pneumomediastinum. Thorax 1996;51(9):960-961. [ Links ]
9. Bejvan SM, Godwin JD. Pneumomediastinum: Old signs and new signs. AJR Am J Roentgenol 1996;166(5):1041-1048. DOI:10.2214/ajr.166.5.8615238 [ Links ]
 Correspondence:
Correspondence:
M Naidoo
naidoom@ukzn.ac.za
Accepted 7 March 2016.














