Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.106 no.4 Pretoria Abr. 2016
http://dx.doi.org/10.7196/samj.2016.v106i4.10168
RESEARCH
Socioeconomic factors associated with asthma prevalence and severity among children living in low-income South African communities
A R YakubovichI; L CluverII; R GieIII
IMSc; PhD student, Department of Social Policy and Intervention, University of Oxford, UK
IIPhD; Department of Social Policy and Intervention, University of Oxford, UK
IIIFCP (Paeds); Department of Paediatrics and Child Health, Faculty of Medicine and Health Sciences, Stellenbosch University, Tygerberg, Cape Town, South Africa
ABSTRACT
BACKGROUND: Rates of asthma, poverty and social deprivation are high among young people in South Africa (SA), yet asthma interventions largely remain focused on biomedical factors
OBJECTIVE: To investigate associations between socioeconomic factors and childhood asthma
METHODS: We recruited 6 002 children aged 10 - 17 years from six low-income urban and rural sites in three SA provinces. Self-report questionnaires measured health status, sociodemographics and socioeconomic factors. Logistic regression and mediation analyses were used to test models of risk factors for asthma prevalence and severity (frequency of attacks
RESULTS: Child anxiety (odds ratio (OR) 1.08; 95% confidence interval (CI) 1.04 - 1.12) and community violence (OR 1.14; 95% CI 1.00 -1.30) were associated with increased odds of having asthma. Children doing more outdoor housework (OR 0.83; 95% CI 0.71 - 0.98) and living in greater poverty (OR 0.93; 95% CI 0.88 - 0.99) had lower odds of having asthma. Severe asthma was predicted by child depression (OR 1.14; 95% CI 1.03 - 1.26) and greater household poverty (OR 1.14; 95% CI 1.01 - 1.28). Most socioeconomic factors operated in 'risk pathways', wherein structural factors (e.g. urban living) were associated with individual factors (e.g. fewer outdoor tasks), which predicted greater odds of having asthma or severe exacerbations
CONCLUSIONS: This study suggests the need to consider the context of childhood asthma in SA for improved prevention and treatment. A multidisciplinary approach may be more effective than a biomedical model, given the plausible effects of psychosocial stress and poverty on asthma outcomes
The prevalence of childhood asthma is rising in many low- and middle-income countries, where widespread barriers to healthcare exacerbate negative health outcomes.[1] Left uncontrolled, childhood asthma can cause increased mortality, morbidity, and substantial school absences, pose an economic burden on families, and contribute to overburdened healthcare systems.
Sub-Saharan Africa (SSA) has a fast-growing asthma burden, with an estimated 50 million asthmatic children under 15, the majority of whom reside in South Africa (SA).[2] While its asthma prevalence rate ranks 25th worldwide, SA ranks fourth for asthma mortality among 5 - 34-year-olds,[3] suggesting the need for improved asthma management and prevention.
Although there are many uncertainties in the aetiology of asthma, the contribution of environmental factors to onset and prognosis is generally recognised, with increasing awareness of social determinants. Yet evidence of risk factors for childhood asthma prevalence and severity in SSA is limited.[2] Most studies in the region have focused on urban-rural differences, finding that asthma is more common among children in urban than rural areas.[2] While urban-rural comparisons are valuable, it is important to assess how other social conditions at individual, family, community and structural levels affect the development of asthma. These may influence asthma directly, as aetiological or exacerbating factors, or indirectly via psychosocial behaviour.[4]
Three studies have investigated socioeconomic determinants of asthma in SA. These found either that better socioeconomic circums tances (e.g. higher income, employment) are related to a higher prevalence of childhood asthma,[5,6] or no association.[7] In contrast, the only study that investigated disease severity found that the prevalence of frequent asthma symptoms (monthly or more) increased with socioeconomic deprivation.[6] Studies in other resource-limited countries such as India and Brazil have identified additional social risk factors for asthma prevalence and severity, including larger household size, family and community violence, low social support, informal housing, anxiety and depression.[8,9] These studies corroborate a 'stress hypothesis' for asthma, whereby greater life stress increases the likelihood of asthma onset and frequent exacerbations. No studies have tested this type of socioeconomic risk model for childhood asthma in southern Africa, however, despite high rates of violence, poverty and psychological problems.
Objective
To investigate whether socioeconomic conditions are associated with an increased prevalence of asthma and severe asthma, as well as the mechanisms by which socioeconomic risk factors may affect asthma in children living in both rural and urban low-income communities in SA.
Methods
Participants and procedure
This cross-sectional survey was conducted from 2009 to 2011 and included 6 002 children aged 10 - 17 years in three urban and three rural low-income health districts in Mpumalanga, KwaZulu-Natal, and Western Cape provinces, SA. Census enumeration areas were randomly selected from these districts and, using door-to-door household sampling, one child was randomly selected from every household with a child aged 10 - 17 years. Additionally, in KwaZulu-Natal each child's primary caregiver was also interviewed to validate the questionnaires used to investigate children's self-reports of asthma, as detailed below.
Children and their primary caregiv-ers voluntarily provided informed consent. Interviewers trained to work with vulnerable children administered a 1-hour questionnaire with standardised measures in the participant's language of choice. Confidentiality was maintained except when children were at risk for significant harm or requested assistance, in which case referrals were made to health and social services. Ethics approval for the study was received from the universities of Oxford (SSD/CUREC2/09-52), Cape Town (389/2009) and KwaZulu-Natal (HSS/0254/09), the SA Department of Social Development, and provincial departments of health and education.
Outcomes
Asthma prevalence. Asthma was defined as a positive response to the question: 'In the past year, have you had asthma?' As no asthma questionnaire has been validated with children in SA, this measure was checked by symptom corroboration, caregiver and child report triangulation, and a family history of asthma.
Severe asthma prevalence. Participants who experienced more than one asthma attack per month were classified as having severe asthma.[10] To improve recall accuracy, participants reported the number of asthma attacks experienced in the past month rather than the past year.
Child factors
Sociodemographic measures included gender, age, and urban/rural location.
Indoor and outdoor household tasks.
The Multidimensional Assessment of Caring Activities[11] was adapted to include common tasks identified by SA children during piloting. Outdoor tasks were working with crops or animals, fetching water, and collecting firewood or making fires. Indoor tasks were cooking for others, washing other people's clothes, and cleaning the home.
Psychological stress. Anxiety symptoms were measured using an abbreviated version of the Revised Children's Manifest Anxiety Scale,[12] validated locally. Depressive symptoms were measured using the 10-item Child Depression Inventory Short Form.[13]
Family factors
Household size. Participants drew a map of their dwelling and identified each person who slept there at least four nights per week.
Domestic conflict and abuse were measured using UNICEF items for SSA. [14] Participants indicated whether they had experienced physical abuse (slapped, punched or hit), emotional abuse (threatened or insulted), family conflict (verbal violence between adults), or domestic violence (physical violence between adults) in the home in the past week.
Community factors Community violence was assessed using the Child Exposure to Community Violence Checklist,[15] adapted to reflect the most common violent experiences for SA children. Participants indicated whether they had ever been assaulted or robbed or witnessed a stabbing or shooting.
Social support was measured using the standardised Social Support Scale.[16] Participants reported personal, material, and emotional support from caregivers, siblings, school teachers/principals, religious leaders, best friends and close friends.
Structural factors
Housing type was measured using census distinctions and categorised as 'informal' (shack) or 'formal' (all else).
Household employment was determined using the household maps as the number of employed people sleeping in the home.
Household poverty was measured by reported access to the nationally identified top eight socially perceived necessities for SA children.[17] Necessities were three daily meals, money for school fees, school uniform, doctor visits and required medicines, clothes to keep warm and dry, school equipment, everyday toiletries, and more than one pair of shoes.
Analyses
Analyses were executed in four phases in IBM SPSS 21.0. First, we evaluated the preliminary validity of our asthma measure: child self-report of asthma was cross-tabulated with asthma symptoms, caregiver report of the child's asthma, and caregiver self-report of asthma.
Second, models of risk factors were built empirically in two steps. In step 1, each asthma outcome was logistically regressed onto each potential risk factor, controlling for sociodemographic factors (age, gender, province, urban/rural location). Subsequently, variables that were statistically significant in step 1 were included in a hierarchical logistic regression for each outcome. We also decided a priori to include household poverty in both models as a proxy for socioeconomic status, which has shown a mixed association with asthma that may indicate that it depends on the presence of other factors.[6-8] For each asthma outcome, variables were entered into the model as follows to assess the contribution of each conceptual set: (i) sociodemographic factors; (ii) structural factors; (iii) community factors; (iv) family factors; and (v) child factors.
Finally, mediation analyses were conducted to test whether structural risk factors operated in 'risk pathways' with individual-level risk factors acting as mediators for each asthma outcome. Indirect effects were assessed using the PROCESS macro in SPSS,[18] which produces 95% bias-corrected confidence intervals by bootstrapping (random resampling with replacement). Mediation analyses controlled for all variables in the relevant risk model. Mediators were tested simultaneously where applicable to evaluate the relative importance of each. Where k exogenous variables were proposed, analyses were conducted k times to estimate each indirect effect.
Results
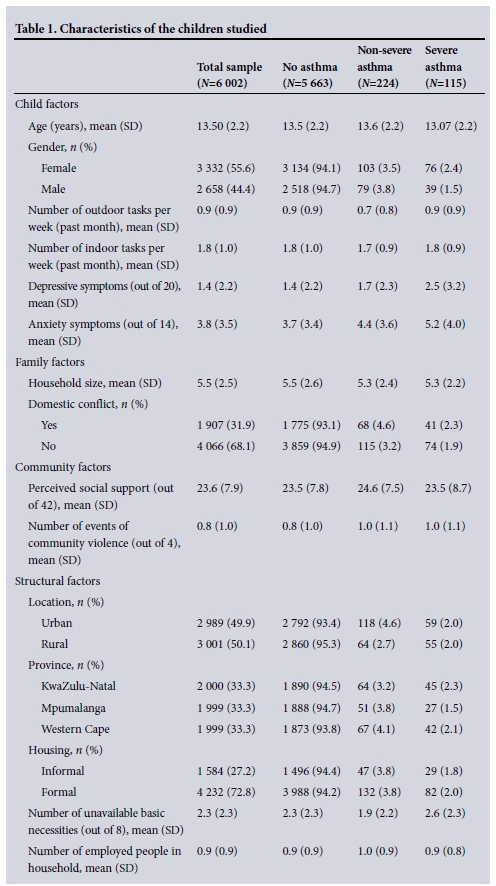
As shown in Table 1, the average age of the 6 002 children studied was 13.5 (standard deviation (SD) 2.18) years. The prevalence of asthma was 5.8%, with 38.7% of asthmatic participants experiencing severe forms of the disease (more than monthly attacks). Participants were split roughly equally between urban (n=2 991) and rural (n=3 007) areas and lacked on average 2.27 (SD 2.32) basic necessities, with 67.8% lacking at least one.
Characteristics of asthma self-report
Child self-report of asthma was cross-tabulated with typical asthma symptoms, caregiver report of the child's asthma, and biological history of asthma. A persistent cough (p<0.001), cough with sputum production (p<0.001), caregiver report of asthma (p<0.001), and biological caregivers' self-reported asthma (p<0.001) were strongly related to the child's self-reported asthma. Agreement between caregivers and children was 94.1% (k=0.416, p<0.001). In contrast, non-biological caregivers' self-report of asthma was not associated with child self-report of asthma (p>0.05).
Preliminary model building
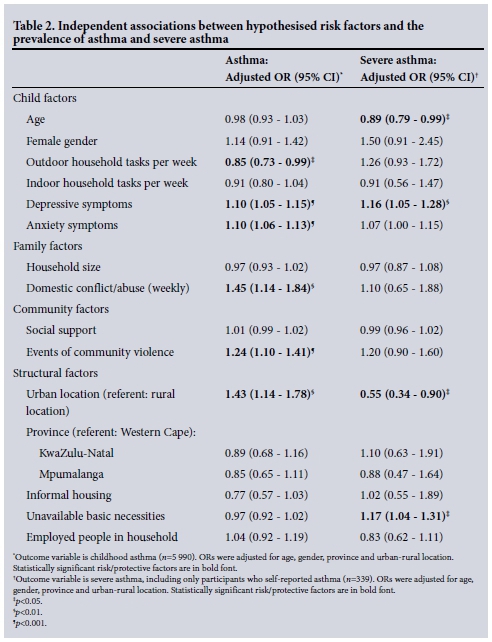
Independent multiple logistic regressions were run to determine which social conditions were significantly related to asthma and severe asthma, controlling for age, gender, province and urban/rural location (Table 2). Social factors associated with higher asthma prevalence in this preliminary stage were performing fewer outdoor tasks, greater depressive and anxiety symptoms, domestic conflict/abuse, greater community violence, and living in urban areas. Preliminary factors related to a higher prevalence of severe asthma were younger age, more depressive symptoms, rural living, and greater household poverty.
Final risk models
Statistically significant factors and socio-demographic covariates were entered into a hierarchical logistic regression for asthma and severe asthma, with household poverty included as a proxy for socioeconomic status.
Asthma prevalence
The final model for asthma prevalence (Table 3) significantly fit the data (p<0.001), with each set of factors improving model fit. Less frequent performance of outdoor tasks (odds ratio (OR) 0.83), less severe household poverty (OR 0.93), greater community violence (OR 1.14), and greater anxiety (OR 1.08) were associated with an increased prevalence of asthma among participants. Both domestic conflict/abuse and urban living became non-significant when more proximal social factors were added to the model, suggesting that these factors may instead have indirect effects on asthma prevalence. Household poverty became statistically significant in the final step, suggesting that its effect on asthma prevalence is part of a suppression effect (i.e. it is dependent on the presence of another factor).
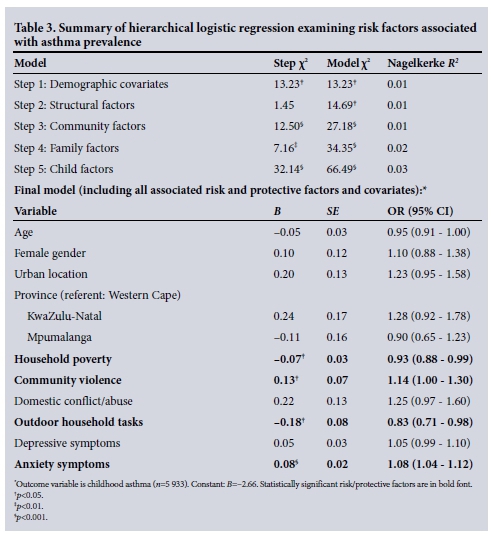
Severe asthma prevalence
The final model for severe asthma prevalence (Table 4) significantly fit the data (p<0.001), with each set of factors improving fit. Factors associated with higher prevalence of severe asthma were younger age (OR 0.87), greater household poverty (OR 1.14), and greater depressive symptoms (OR 1.14).

Mediation analyses
Mediation analyses were conducted to evaluate whether structural risk factors affected asthma outcomes via individual-level factors (Fig. 1).
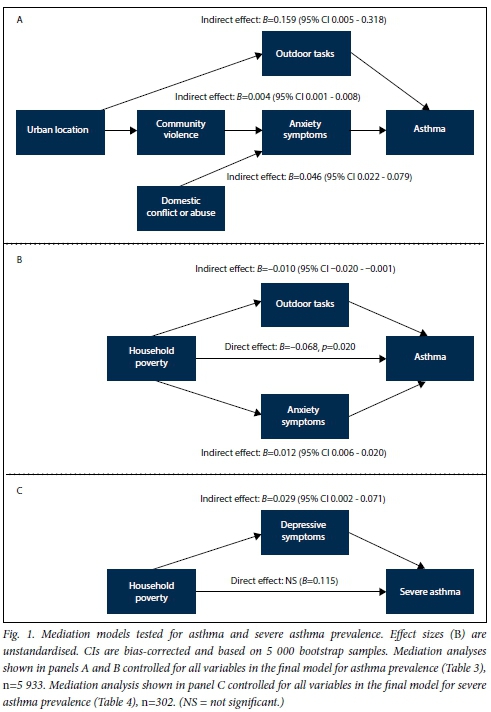
Asthma prevalence
Panel A in Fig. 1 summarises three mediation analyses that estimated the indirect effects of urban location and domestic conflict/abuse on asthma prevalence. Living in urban areas was associated with a higher asthma prevalence via greater community violence and greater anxiety. However, the effect was very small (B=0.004). Participants living in urban areas additionally performed fewer outdoor tasks, which was also associated with higher rates of asthma (B=0.16). Participants exposed to domestic conflict/abuse had greater levels of anxiety, which in turn was associated with higher asthma prevalence (B=0.05).
Panel B shows that, although overall greater household poverty was associated with lower asthma prevalence, poverty indirectly influenced childhood asthma in two contrasting ways. Participants living in more severely impoverished households tended to perform more outdoor tasks, which was related to lower asthma prevalence (5=-0.01). But simultaneously more severe poverty was associated with greater child anxiety, which was related to higher asthma prevalence (5=0.01).
Severe asthma prevalence
Household poverty was associated with greater child depression, which in turn was related to a higher prevalence of severe asthma (5=0.03).
Discussion
This study is the first large-scale investigation of socioeconomic risk factors for childhood asthma prevalence and severity in both rural and urban SA. Hierarchical modelling with additional social risk factors suggested that urban living does not directly affect asthma. Instead, greater community violence, greater anxiety, lower household poverty, and performing less outdoor housework (e.g. tending to crops and/or animals) were uniquely associated with greater prevalence rates of childhood asthma. Urban living, in contrast, affected greater asthma prevalence indirectly via at least two risk pathways: (i) decreased time on outdoor tasks; and (ii) greater community violence and anxiety.
These findings support previous studies examining pathways between higher rates of asthma and more urbanised lifestyles, which entail less agricultural activity and so less protective microbial exposure.[8] The higher prevalence of asthma observed among children with less outdoor work and living in urban communities may also reflect the risks of longer exposure to indoor allergens and irritants (e.g. environmental tobacco smoke). Additionally, our results support a psychosocial pathway to asthma that begins in violence-concentrated urban areas. This 'stress model' is further suggested by the finding that domestic conflict is associated with increased anxiety and in turn higher asthma prevalence. Indeed a systematic review of prospective cohort studies found that in addition to being a product of asthma, psychosocial stress contributes to asthma onset and prognosis.[19]
While worldwide the relationship between socioeconomic status and childhood asthma is mixed, two of three SA studies found that greater socioeconomic deprivation is associated with lower childhood asthma rates.[5,6] This study supports this conclusion, finding that more severe household poverty was associated with lower asthma prevalence. Mediation analysis revealed a more complex story: living in more severely impoverished households was associated with more outdoor housework and in turn lower odds of having asthma; however, it was also associated with greater anxiety and in turn higher odds of having asthma. The first indirect effect is congruent with cross-sectional evidence that more urbanised lifestyles - an asthma risk factor - are associated with higher socioeconomic status.[8] The latter, positive indirect effect suggests that living in more severe poverty still confers indirect risks for asthma via increased stress.
However, among asthmatic children, severe asthma (more than monthly asthma attacks) had different risk pathways. Greater household poverty was associated with having severe asthma - consistent with evidence from both high- and low-income countries that lower socioeconomic status is associated with greater asthma severity. [6] Moreover, congruent with evidence from high-income countries[20] but previously untested in SSA, this effect was mediated by having more severe depressive symptoms - suggesting that psychosocial stress exacerbates asthma severity in addition to contributing to onset.
Study limitations
This study has several limitations. Owing to the lack of complex models tested for childhood asthma in SSA, the current models were empirically created. Confirmatory, longitudinal research is needed to evaluate the social risk factors implicated before sound policy decisions can be made. Additionally, early life, biological, and environmental risk factors (e.g. breastfeeding, pollution) were not measured. Future modelling should include these to assess the relative importance of socioeconomic factors and possible interactions and mediations. Using self-reports of asthma also has weaknesses. Firstly, more impoverished children may be less likely to be diagnosed owing to poorer healthcare access. This could in part explain the association between less severe poverty and greater asthma prevalence, while under-treatment probably contributes to greater disease severity among more impoverished children. Secondly, some participants with self-reported asthma may not have been truly asthmatic. For instance, a chronic cough or wheeze may be misdiagnosed as asthma but actually indicate an HIV-related lung disease, tuberculosis or bronchiectasis. Measuring wheeze is commonly used to identify participants who are unaware of their asthma status in questionnaires.[10] However, in addition to possible conflation, the relevance of wheeze in the current context is questionable: in a random sample of low-income parents in Cape Town, only 5% described their asthmatic child's symptoms as 'wheeze'.[21] Despite these limitations, the current measure strongly correlated with asthma symptoms, biological family history and caregiver report, suggesting good specificity for identifying risk factors. Finally, we only sampled low-income, high HIV-prevalent communities; our findings are therefore relevant to the lower end of the socioeconomic gradient and are not generalisable to all of SA.
Conclusions
With the above limitations in mind, our findings have tentative implications for the direction of public health policy and research. SA's childhood asthma management guidelines focus on medical diagnosis and treatment, largely ignoring the social distribution of asthma.[22] This study suggests that successful asthma management may require consideration of the broader social factors that could affect asthma outcomes, such as violence and stress. Psychological interventions may be beneficial for asthma prevention and treatment, while it is essential to investigate how harmful social conditions hinder children's access and adherence to appropriate medication. It is likely that future public health programming will need to develop multidisciplinary interventions, including psychosocial interventions, to counter SA's rising asthma epidemic.
Acknowledgments. This study was funded by the UK Economic and Social Research Council, the South African Research Foundation, the South African Department of Social Development, the Claude Leon Foundation, the Nuffield Foundation, HEARD at the University of KwaZulu-Natal, the John Fell Fund, the Leverhulme Trust, the University of Oxford's ESRC Impact Acceleration Account, and the European Research Council under the European Union's Seventh Framework Programme (FP7/2007-2013)/ ERC grant agreement (313421). ARY received additional support from a Rotary Global Grant (GG1412399). The authors thank the fieldwork teams and all the children and families who participated.
References
1. Ait-Khaled N, Enarson D, Bousquet J. Chronic respiratory diseases in developing countries: The burden and strategies for prevention and management. Bull World Health Organ 2001;79(10):971-979. DOI:10.1590/S0042-96862001001000011 [ Links ]
2. Adeloye D, Chan KY, Rudan I, Campbell H. An estimate of asthma prevalence in Africa: A systematic analysis. Croat Med J 2013;54(6):519-531. DOI:10.3325/cmj.2013.54.519 [ Links ]
3. Masoli M, Fabian D, Holt S, Beasley RW. The global burden of asthma: Executive summary of the GINA Dissemination Committee Report. Allergy 2004;59(5):469-478. DOI:10.1111/j.1398-9995.2004.00526.x [ Links ]
4. Rona RJ. Asthma and poverty. Thorax 2000;55(3):239-244. DOI:10.1136/thorax.55.3.239 [ Links ]
5. Calvert J, Burney P. Effect of body mass on exercise-induced bronchospasm and atopy in African children. J Allergy Clin Immunol 2005;116(4):773-779. DOI:10.1016/j.jaci.2005.05.025 [ Links ]
6. Poyser MA, Nelson H, Ehrlich RI, et al. Socioeconomic deprivation and asthma prevalence and severity in young adolescents. Eur Respir J 2002;19(5):892-898. DOI:10.1183/09031936.02.00238402 [ Links ]
7. Maluleke KR, Worku Z. Environmental determinants of asthma among school children aged 1314 in and around Polokwane, Limpopo Province, South Africa. Int J Environ Res Public Health 2009;6(9):2354-2374. DOI:10.3390/ijerph6092354 [ Links ]
8. Cooper PJ, Rodrigues LC, Barreto ML. Influence of poverty and infection on asthma in Latin America. Curr Opin Allergy Clin Immunol 2012;12(2):171-178. DOI:10.1097/ACI.0b013e3283510967 [ Links ]
9. Subramanian SV, Ackerson LK, Subramanyam MA, Wright RJ. Domestic violence is associated with adult and childhood asthma prevalence in India. Int J Epidemiol 2007;36(3):569-579. DOI:10.1093/ije/dym007 [ Links ]
10. ISAAC Coordinating Committee. Manual of the International Study of Asthma and Allergies in Childhood (ISAAC). 2nd ed. Auckland/Munster: ISAAC, 1993. [ Links ]
11. Joseph S, Becker F, Becker S. Manual for Measures of Caring Activities and Outcomes for Children and Young People. London: Princess Royal Trust for Carers, 2009. [ Links ]
12. Reynolds CR, Richmond BO. What I think and feel: A revised measure of children's anxiety. J Abnorm Child Psychol 1978;6(2):271-280. DOI:10.1007/BF00919131 [ Links ]
13. Kovacs M. Children's Depression Inventory. Niagra Falls, NY: Multi-Health Systems, 1992. [ Links ]
14. Snider LM, Dawes A. Psychosocial vulnerability and resilience measures for national-level monitoring of orphans and other vulnerable children: Recommendations for revision of the UNICEF Psychological Indicator. Cape Town: UNICEF, 2006. [ Links ]
15. Richters J, Martinex P. The NIMH Community Violence Project: i. Children as victims of and witnesses of violence. Psychiatry 1993;56(1):7-21. DOI:10.1521/00332747.1993.11024617 [ Links ]
16. Seidman E, Allen LR, Aber JL, et al. Development and validation of adolescent-perceived microsystem scales: Social support, daily hassles, and involvement. Am J Community Psychol 1995;23(3):355-388. DOI:10.1007/BF02506949 [ Links ]
17. Wright G. Findings from the Indicators of Poverty and Social Exclusion Project: A Profile of Poverty Using the Socially Perceived Necessities Approach. Key Report 7. Pretoria: Department of Social Development, 2008. [ Links ]
18. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York: Guilford Press, 2013. [ Links ]
19. Chida Y, Hamer M, Steptoe A. A bidirectional relationship between psychosocial factors and atopic disorders: A systematic review and meta-analysis. Psychosom Med 2008;70(1):102-116. DOI:10.1097/.PSY.0b013e31815c1b71 [ Links ]
20. Schreier HMC, Chen E. Socioeconomic status and the health of youth: A multilevel, multidomain approach to conceptualizing pathways. Psychol Bull 2013;139(3):606-654. DOI:10.1037/a0029416 [ Links ]
21. Ehrlich RI, Jordaan E, du Toit D, Volmink JA, Weinberg E, Zwarenstein M. Underrecognition and undertreatment of asthma in Cape Town primary school children. S Afr Med J 1998;88(8):986-994. [ Links ]
22. Motala C, Green RJ, Manjra AI, Potter PC, Zar HJ. Guideline for the management of chronic asthma in children - 2009 update. S Afr Med J 2009;99(12):898-912. [ Links ]
 Correspondence:
Correspondence:
A R Yakubovich
alexa.yakubovich@spi.ox.ac.uk
Accepted 2 February 2016.














