Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.106 n.4 Pretoria Apr. 2016
http://dx.doi.org/10.7196/samj.2016.v106i4.10146
RESEARCH
The S'Khokho 'bushcan' initiative: Kick a bush and condoms fall out
J Pienaar
MSc; S'Khokho Community Health, KwaZulu-Natal, South Africa
ABSTRACT
BACKGROUND: People living in rural areas have limited access to condoms owing to distance, cost and time involved in travelling to public health facilities, around which most condom distribution efforts are centralised.
OBJECTIVE: In an effort to increase access to condoms in these areas, we explored the feasibility and efficacy of condom distribution by placing 'condocans' on trees along informal footpaths used by residents.
METHODS: From October 2012, steel condocans, typically seen in clinic settings, were erected on trees along pathways in bushy areas with high levels of foot traffic at several rural locations in the uMgungundlovu district of KwaZulu-Natal Province, South Africa (SA). Because of their location, the condocans were referred to as 'bushcans'. Condom uptake was closely monitored, and the bushcans were restocked when necessary.
RESULTS: Following the introduction of the bushcans, male condom distribution increased by 237% from October 2012 to December 2012. Condom distribution in these areas increased on average by 187% from October 2012 to October 2015, with more than 408 000 condoms distributed over the 3-year period using the bushcans alone. Discussions with residents revealed that they were pleased about the increased access to condoms via the bushcans, and they recommended other areas for potential implementation of this initiative.
CONCLUSIONS: The bushcan initiative highlighted the fact that condoms are not as easily accessible to all South Africans as is often thought. By providing access to condoms in a discreet and convenient manner, the bushcans have the potential to increase access to condoms in other rural and periurban areas in SA where communities face similar barriers to access.
S'Khokho is a non-profit organisation focusing on rural health and community development and operating in three rural and periurban areas of KwaZulu-Natal Province, South Africa (SA), namely Hilton, Cedara and Howick West. People living in these areas have limited access to condoms owing to distance, cost and time involved in travelling to public health facilities, around which most condom distribution efforts are centralised.
The National Department of Health, in collaboration with non-governmental organisations and the development sector in SA, has embarked on large-scale efforts to improve access to and uptake of condoms in efforts to reduce HIV and sexually transmitted infection acquisition and unplanned pregnancies. Despite condom distribution revitalisation campaigns across provinces, SA has witnessed a decline in condom uptake, a recent survey by the Human Sciences Research Council reporting that condom use declined significantly from 2008 to 2012 (p<0.001).[1] Although this may not only be due to difficulties in accessing condoms, it is noteworthy that condom access is not as universal as policy makers and public health officials believe it to be. Prevention is only effective if methods and efforts are sustained 100% of the time. A method is only useful if it is available, and condoms will not be used at the desired 100% of sex acts if condoms are not accessible 100% of the time.
Several studies have reported that distance and the cost of travelling to public health facilities play a pivotal role in predicting uptake of health services.[2-5] Referring to 'distance decay', Tanser et al.[3] found that there was a significant decline in public health facility use with increasing travel time (p<0.0001), individuals living within 30 minutes of a clinic utilising clinic services 10 times more often (adjusted odds ratio 10; 95% confidence interval 6.9 - 14.4) than those whose travel time to the clinic was in excess of 90 minutes.
Government-issued condoms are freely distributed, but they are typically distributed only in healthcare settings or government buildings. There are no condom dispensers in public places such as public toilets or taxi ranks. While considered to be widely accessible, condoms are not easily available, especially to rural community residents who have difficulty in accessing clinics as a result of distance to clinics and prohibitive transport costs.
Furthermore, women constitute the majority of the client base at public health facilities,[4] which means that men tend not to have access to government-issued condoms unless these are acquired by their female partners. However, women are ridiculed and face stigma if they are seen obtaining, stocking up on or supplying condoms.[7] Doing so can also lead to their male partners suspecting them of infidelity, and the perception that they may be engaging in sex work.
Based on these obstacles to condom access, it was considered appropriate to implement a novel approach to condom distribution specially for rural and periurban communities. People do not want to attend clinics to collect condoms, nor is this feasible for residents in these communities owing to prohibitive transport costs. Furthermore, it has been reported that healthcare practitioners have been known to ridicule clients who stock up on condoms at their clinic visits.
In an effort to increase access to condoms in rural areas, we explored the feasibility and efficacy of condom distribution by placing 'condocans' on trees along informal footpaths used by residents.
Methods
Observations of informal footpaths in local rural areas were undertaken to assess the feasibility of condom distribution along these pathways. The footpaths were frequented by local residents travelling to the nearest town for work or shopping, or used as gateways to other nearby communities. Starting in October 2012, several steel condocans, typically seen in clinic settings, were erected on trees along pathways in bushy areas with high levels of foot traffic at locations around Umngeni subdistrict. Because of their location, the condocans were referred to as 'bushcans'.
The location of the bushcans was influenced by average foot traffic, available shade from trees, and a person's ability to take the condoms with some degree of privacy as they walked past (Fig. 1). Condom uptake was closely monitored, and the bushcans were restocked when necessary. Footpaths with heavy foot traffic were prioritised, and after the success of the initial pilot, additional bushcans were erected in other rural communities. Expansion of this novel condom distribution method continued, and by April 2015, over 20 bushcans had been strategically erected along bushy footpaths, at local taxi stops and in 'lover spots'.

Results
Before the introduction of the bushcan method, S'Khokho distributed 32 500 male condoms from January 2012 to 15 October 2012. After introduction of the bushcans (Fig. 2), male condom distribution increased by 237% over a 2-month period. During November 2012, 14 850 condoms were distributed for that month alone. In total 20 025 condoms were dispensed from the bushcans over the 10-week period ending 31 December 2012, with annual distribution totalling 63 900 condoms. Initially the bushcans had to be restocked almost daily, but the demand gradually tapered once residents realised that the bushcans were restocked regularly and that this condom supply was stable.
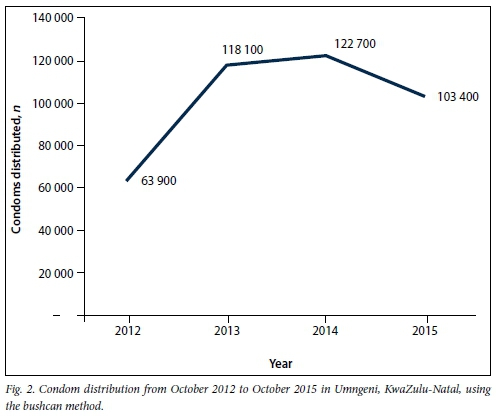
Following expansion of the bushcan initiat ive, condom uptake has increased by an overall 187%, with an annual average distribution of over 119 000 in these areas.
Qualitative findings
Informal discussions with local residents revealed that they were pleased about the increased access to condoms via the bush-cans, and they recommended other areas for potential implementation of this initiative. They reported that is very useful to have condoms available in close proximity to their place of residence or travelling routes, and requested that the service continue. Local community leaders were very vocal in supporting the initiative, and encouraged further efforts in this regard.
Conclusions
The bushcan initiative highlighted the fact that condoms are not as easily accessible to all South Africans as is often thought. By providing access to condoms in a discreet and convenient manner, the 'bushcans' have the potential to increase access to condoms in other rural and periurban areas in SA where communities face similar barriers to access. It is, however, essential that if this method is adopted, efforts must be sustained in the provision of condom access by ensuring timeous stocking up of the distribution points.
Acknowledgement. This work was supported by HiVOS (Humanistisch Instituut voor Ontwikkelingssamenwerking), grant number LO SA at HO 1009618.
References
1. Shisana O, Rehle T, Simbayi LC, et al. South African National HIV Prevalence, Incidence and Behaviour Survey, 2012. Cape Town: HSRC Press, 2014. [ Links ]
2. McLaren ZM, Ardington D, Leibbrandt M, et al. Distance decay and persistent health care disparities in South Africa. BMC Health Serv Res 2014;541. DOI:10.1186/s12913-014-0541-1 [ Links ]
3. Tanser F, Gijsbertsen B, Herbst K. Modelling and understanding primary health care accessibility and utilization in rural South Africa: An exploration using a geographical information system. Soc Sci Med 2006;63(11):691-705. DOI:10.1371/journal.pone.0013909 [ Links ]
4. Harris B, Goudge J, Ataguba JE, et al. Inequities in access to health care in South Africa. J Public Health Policy 2011;32(1):102-123. DOI:10.1057/jphp.2011.35 [ Links ]
5. Burger R, Bredenkamp C, Grobler C, van der Berg S. Have public health spending and access in South Africa become more equitable since the end of apartheid? Dev South Afr 201239(5):681-703. DOI:10.1080/0376835X.2012.730971 [ Links ]
6. Aulette-Root A, Boonzaier F, Aulette J. South African Women Living with HIV: Global Lessons from Local Voices. Bloomington, IN: Indiana University Press, 2014. [ Links ]
 Correspondence:
Correspondence:
J Pienaar
jpienaar@skhokho.org
Accepted 22 October 2015.














