Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.106 n.2 Pretoria Feb. 2016
http://dx.doi.org/10.7196/SAMJ.2016.V106I2.10328
CME
An approach to the patient with suspected pericardial disease
C G KyriakakisI; B M MayosiII; E de VriesIII; A IsaacsIV; A F DoubellV
IMB ChB, FCP (SA), MMed (Int), Cert Cardiology (SA); Division of Cardiology, Department of Medicine, Faculty of Medicine and Health Sciences, Stellenbosch University and Tygerberg Academic Hospital, Cape Town, South Africa
IIMB ChB, FCP (SA), DPhil; Department of Medicine, Faculty of Health Sciences, Groote Schuur Hospital and University of Cape Town, South Africa
IIIMB ChB, MFamMed, FCFP (SA); Department of Family Medicine, Mitchell's Plain Hospital, Cape Town, South Africa
IVMB ChB, MFamMed; Division of Family Medicine, School of Public Health and Family Medicine, Faculty of Health Sciences, University of Cape Town, South Africa
VMB ChB, MMed (Int), FCP (SA), BSc Hons, PhD; Division of Cardiology, Department of Medicine, Faculty of Medicine and Health Sciences, Stellenbosch University and Tygerberg Academic Hospital, Cape Town, South Africa
ABSTRACT
Diseases of the pericardium commonly manifest in one of three ways: acute pericarditis, pericardial effusion and constrictive pericarditis. In the developed world, the most common cause of acute pericarditis is viral or idiopathic disease, while in the developing world tuberculous aetiology, particularly in sub-Saharan Africa, is commonplace owing to the high prevalence of HIV. This article provides an approach to the diagnosis, investigation and management of these patients.
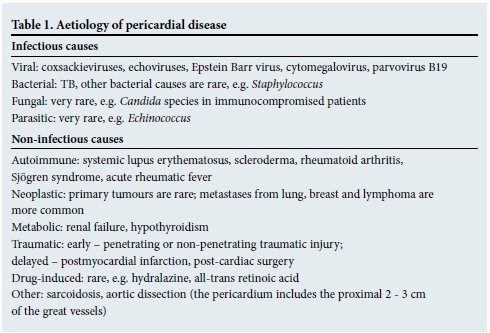
Pericardial diseases are relatively common in clinical practice, presenting in one of three ways: pericarditis (which may recur or become chronic), pericardial effusion with or without pericardial tamponade and constrictive pericarditis. Less common manifestations include pericardial cysts and neoplasms. A variety of aetiologies (Table 1) are implicated in pericardial disease, and establishing a definitive diagnosis is challenging, as the yield of diagnostic tests is relatively low.[1] The incidence of acute pericarditis is 27.7/100 000 cases in the developed world and accounts for 5% of emergency room admissions for chest pain.[2,3] Viral infection is responsible for the majority of cases in the developed world, while in the developing world Mycobacterium tuberculosis, particularly with HIV co-infection in sub-Saharan Africa, remains prevalent.[4,5]
A paucity of randomised data exists in the field of pericardial disease; however, more recently multicentre randomised trials have defined the role of colchicine in acute and recurrent pericarditis and that of steroid therapy in tuberculous pericarditis.[6-8] This review focuses predominantly on an approach to acute pericarditis commonly encountered at primary care level, and offers brief insights into effusive disease and constriction.
An approach to pericarditis
The following is a stepwise approach to acute pericarditis:
- Presenting symptoms and signs.
- Appropriate special investigations.
- When to consider hospital admission.
- Evidence-based medical therapy and assessing for a response.
- Prognosis.
- Recurrent pericarditis.
Presenting symptoms and signs
Positional pleuritic chest pain, improved by sitting forward and exacerbated by deep inspiration, is present in >85 - 90% of cases.[3] Radiation of pain to the trapezius ridge is virtually pathognomonic of pericarditis, as the phrenic nerve that innervates these muscles traverses the pericardium.[9] Prodromal symptoms of a viral illness may be present and constitutional symptoms of tuberculosis (TB) should be sought. Sinus tachycardia and low-grade fever are common, while a temperature >38oC suggests a specific cause of pericarditis. A triphasic pericardial friction rub is audible in approximately one-third of cases, best heard with the diaphragm of the stethoscope over the left lateral sternal border with the patient leaning forward (Audio 1).[3] This can be transient and frequent evaluation for its presence is useful as it is highly specific for the disease.
Signs of an underlying systemic inflammatory disease may point to a specific cause, e.g. systemic lupus erythematosus with a pericardial serositis.
A clinical diagnosis of pericarditis can be established when two of the following criteria are present:[3]
- Pericarditic chest pain.
- Pericardial friction rub.
- Characteristic electrocardiogram (ECG) changes.
- Pericardial effusion.
Appropriate special investigations
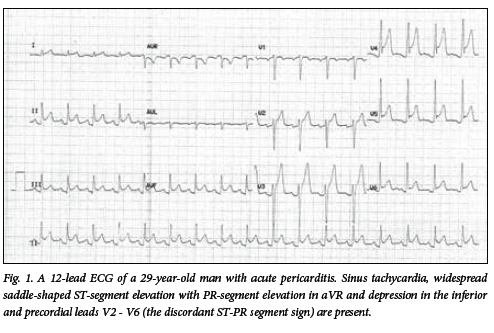
The following are recommended in all patients with suspected pericarditis: a 12-lead ECG, a chest radiograph, inflammatory markers and a transthoracic echocardiogram.[10]
A 12-lead ECG is the first-line investigation
- Typical ECG findings are found in up to 60% of patients, are highly variable between different patients and are influenced by therapy.[11]
- They include (Fig. 1):
- Widespread saddle-shaped (concave upward) ST-segment elevation not confined to a single coronary territory with reciprocal ST depression in aVR.
- Inferior and precordial PR-segment depression with PR-segment elevation in aVR - the discordant ST-PR segment sign. This is more specific for pericarditis than diffuse ST elevation alone.[12]
- Sinus tachycardia.
- Q waves may be present in post-myocardial infarction (MI) pericarditis. Both early and late (Dressler's syndrome) manifestations are rare in the era of reperfusion therapy; they may however occur after a silent MI or a missed infarct.
- Ultimately the ST and PR segments normalise, which may be followed by widespread T-wave inversion.
- The most important differential diagnosis is that of an ST-elevation acute coronary syndrome. This necessitates a thorough evaluation of the nature of the chest pain and the morphology and distribution of ST elevation on ECG.
Chest radiograph
- Features of pleuropulmonary disease may point to a specific aetiology, e.g. TB.[13]
- The cardiac silhouette only increases when >300 mL of pericardial fluid has collected and is therefore commonly normal in acute pericarditis.[14]
Laboratory tests
- Inflammatory markers: C-reactive protein (CRP), or erythrocyte sedimentation rate (ESR) where CRP is not available, and a white cell count should be undertaken in all cases. Elevations are supportive of a diagnosis of acute pericarditis and are valuable for monitoring disease activity and response to therapy.[15]
- Troponins may be elevated in patients with associated myocarditis.[16]
- Given its high prevalence in sub-Saharan Africa, TB should always be considered as a possible cause. Constitutional symptoms of TB and/or radiological evidence of the disease mandate further work-up. A high index of suspicion for TB must be maintained in patients from a disadvantaged socioeconomic setting.[17]
- Retroviral serology and serum creatinine level determination should be undertaken routinely.
- Routine serological markers for connective tissue disease are not indicated in low-risk cases; neither is routine viral serology as it has a low yield and does not alter management.[1]
- A more detailed search for a specific cause is undertaken in patients requiring hospital admission or who fail a trial of medical therapy.
Transthoracic echocardiogram (TTE)
- An associated pericardial effusion, its haemodynamic effects and possible myocarditis can be evaluated via TTE.
- TTE is recommended in all patients.[10] However, in under-resourced areas it would not be unreasonable to limit it to patients requiring hospital admission or in whom a specific aetiology is suspected.
Cardiac magnetic resonance and cardiac computed tomography
CMR can more accurately delineate pericardial inflammation by means of pericardial late gadolinium enhancement.[13] Cardiac CT also offers a more accurate assessment of pericardial thickness than TTE, at the expense of exposure to ionising radiation. Neither of these adjunctive imaging modalities take preference over TTE as a first-line investigation. Their value is in the rare setting where a high clinical suspicion of pericarditis exists, yet the clinical diagnostic criteria remain unmet.[13]
When to consider hospital admission
High-risk cases[18]
Hospital admission is required when a specific aetiology is suspected or when >1 of the following poor prognostic features are present:
- Temperature >38°C.
- Subacute onset.
- Large pericardial effusion (diastolic echo-free space >20 mm) with or without cardiac tamponade.
- Myopericarditis.
- Traumatic pericarditis.
- Chronic oral anticoagulant or immuno-suppressive therapy.
- Failure to respond to at least 1 week of aspirin or non-steroidal anti-inflammatory drug (NSAID) therapy.
A more detailed work-up, including evaluation for TB, connective tissue disease and metabolic diseases, is required. When a specific cause is identified, therapy aimed at the underlying cause is indicated.
Evidence-based medical therapy and assessing for a response
- Low-risk patients, in whom no specific cause is suspected and who do not have predictors of a poor prognosis, can be managed as outpatients.[10] It would not be unreasonable to limit TTE in this group to those who fail to respond to 1 week of anti-inflammatory therapy, particularly when managed at primary healthcare level.
- Restriction of physical activity is recommended until symptoms resolve and the CRP normalises. In athletes, a restriction of athletic activity for at least 3 months is advised, provided the CRP, ECG and TTE have returned to normal at the end of this period.[10] In suspected myopericarditis (elevated troponin level) athletic activity should be avoided for 6 months.[10]
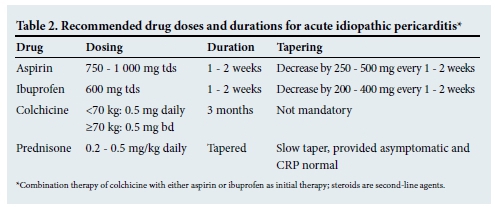
- First-line medical therapy includes aspirin or NSAIDs and colchicine.[6,7] Gastro-protection, preferably proton pump inhibitors, should be provided (Table 2).
- Anti-inflammatory therapy commonly provides abrupt symptomatic relief.
- Colchicine, added to aspirin or NSAID therapy, has been evaluated in two well-conducted, placebo-controlled, randomised clinical trials, where it has been shown to improve the response to medical therapy and prevent recurrences.[6,7]
- Corticosteroids are associated with the evolution of acute pericarditis into a chronic, recurrent disease and are therefore not indicated as first-line therapy.[10] They are considered when NSAIDs or aspirin are contraindicated or have failed to provide a response, and an infective aetiology has been excluded. Alternatively, they are indicated when a specific cause mandates their use, such as connective tissue disease. When indicated for idiopathic disease, they should be used at a low-to-moderate dose together with colchicine and tapered once the CRP has normalised (Table 2).[10]
- Low-risk patients should be re-evaluated after 1 week for a response. Those who fail to respond (persistent symptoms and/or elevated CRP) are considered to be moderate risk and require hospital admission and an aetiology search. Those who respond infrequently require >2 weeks of NSAID or aspirin therapy, while colchicine should be continued for 3 months (Table 2).[10]
Prognosis
- Acute idiopathic or viral pericarditis has a good prognosis with a low complication rate.[19]
- Cardiac tamponade and constrictive pericarditis are more commonly associated with specific underlying aetiologies, particul arly TB and purulent pericarditis.[19]
- Up to 30% of idiopathic cases can develop recurrent pericarditis, associated with considerable morbidity.[20] This risk can be halved by the administration of colchicine at the outset.[20]
Recurrent pericarditis
- This is defined as a recurrence of pericarditis after a symptom-free period of 4 - 6 weeks after the initial illness. While up to 30% of patients may experience a recurrence after the index episode, the risk of a second recurrence may be as high as 50% in those not treated with colchicine, and even higher after corticosteroid administration.[20]
- The most common cause for recurrent pericarditis is the inadequate treatment of an initial episode.[20]
- A search for a potential underlying cause is required and referral for tertiary evaluation is recommended.
- In cases of idiopathic disease, treatment is similar to that for a first attack, except for an extended duration of therapy with both NSAIDs (weeks - months) and weight-adjusted colchicine (>6 months' duration). [20]
- Corticosteroids remain second-line therapy owing to their risk for precipitating a chronic form of the disease.
- In patients who do not respond to anti-inflammatory therapy or who require high maintenance doses of prednisone, azathioprine, intravenous immunoglobulin and anakinra (a recombinant interleukin β receptor antagonist) have been attempted.[10]
- As a last resort, after failed medical therapy, pericardiectomy may be required.[10]
- Overall, the prognosis is good in that a case of constrictive pericarditis has never been attributed to idiopathic recurrent pericarditis. However, morbidity is high owing to persistent symptoms.
An approach to pericardial effusions
- In sub-Saharan Africa TB is responsible in >90% of HIV-positive and 50 - 70% of HIV-negative patients who present with a large pericardial effusion. Emphasis must therefore be placed on excluding TB.[21]
- The development of cardiac tamponade, a life-threatening condition, is determined by the rate of fluid accumulation, pericardial compliance and position of a loculated collection. The rapid accumulation of 200 mL of fluid can lead to acute tamponade, whereas slow accumulation can be well tolerated owing to pericardial distensibility.
- Loculated collections situated over low-pressure chambers, e.g. the right ventricle, can result in early haemodynamic compromise.
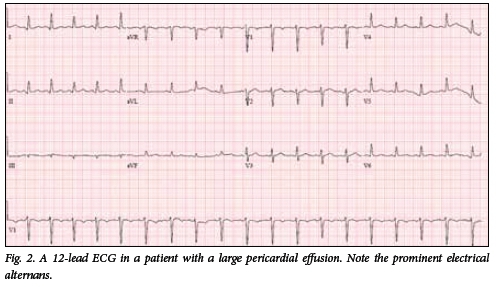
- The 12-lead ECG may reveal small-voltage QRS complexes with electrical alternans due to swinging of the heart within a large collection (Fig. 2 and Video 1).
- Cardiac tamponade remains a clinical diagnosis. Clinical signs include:
- Tachycardia and elevated jugular venous pressure (JVP).
- Muffled heart sounds.
- Pulsus paradoxus (>10 mmHg inspiratory drop in systolic blood pressure).
- A TTE confirms the presence of an effusion, identifies the safest approach for needle aspiration and provides supportive evidence of associated haemodynamic compromise. Pericardiocentesis has a complication rate of 4 - 10%, depending on operator experience and procedural urgency.[22]'Blind' pericardiocentesis is discouraged and TTE or ultrasonographic guidance to determine the site and angle of puncture is recommended.[22] In under-resourced areas, emergency pericardiocentesis in a haemodynamically unstable patient may be necessary without ultrasound guidance, provided the diagnosis of pericardial tamponade is established as accurately as clinically possible.
- Ultrasound or TTE availability is also useful for confirming a puncture that is within the pericardial space and not a cardiac chamber or pleural cavity by the injection of agitated contrast saline bubbles (Video 2).[23]
- All effusions should be evaluated for a specific underlying aetiology. If safely accessible, pericardiocentesis should be undertaken in a controlled environment by a skilled operator.
- A pericardial fluid adenosine deaminase level >35 U/L has a sensitivity and specificity of 89% and 74%, respectively, for the diagnosis of TB pericarditis.[24] Traditional diagnostic tests for pericardial TB are insensitive and require long culture periods. The organism is not identified in the pericardial fluid of 27 - 48% of cases and adenosine deaminase therefore remains an important biochemical diagnostic aid[24,25]
- In our local experience complete percutaneous drainage of a tuberculous effusion, in combination with antituberculous therapy, is associated with an extremely low risk for constriction and cardiac death.[25] One small trial has shown that the addition of intrapericardial urokinase may facilitate this approach.[26] The administration of intrapericardial steroids did not influence the risk of developing constriction in an underpowered trial of 57 patients.[27] However, more recently adjunctive oral steroid therapy has been shown to reduce the risk of constriction in both HIV-positive and -negative patients.[8] In this trial a definite diagnosis of TB pericarditis was established in 16.7% of participants. High-dose oral prednisone did not translate into a mortality benefit and was unfortunately associated with an increase in HIV-related cancers in the HIV-positive group.[8]
An approach to constrictive pericarditis
- Constriction is a form of diastolic heart failure that is potentially curable.
- The heart becomes encased in a rigid shell of pericardium, isolating it from the rest of the thoracic cavity.
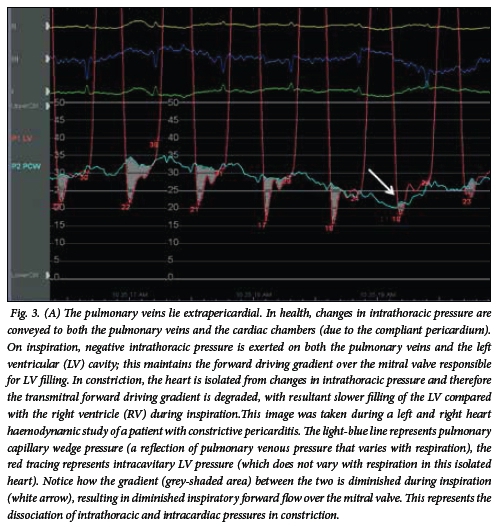
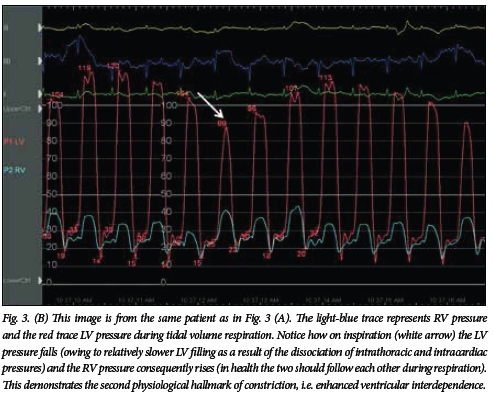
- Respiratory changes in intrathoracic pressure can therefore not be transmitted to the heart, leading to the two hallmark physiological features of constriction:
- dissociation of intrathoracic and intracardiac pressures; and
- enhanced ventricular interdependence (Fig. 3 A and B, and Video 3).
- Establishing a clinical diagnosis is challenging and the disease therefore often goes unrecognised until late in its course, when overt right heart failure develops.
- A high index of suspicion is required in patients who have had prior TB, cardiac surgery, thoracic irradiation or pericarditis. TB remains the most important cause in South Africa.[8]
- Symptoms range from a change in effort tolerance to those of predominant right heart failure.
- Clinical signs may be subtle and careful evaluation for their presence is required:
- A raised JVP with rapid y-descents (Video 4). The JVP may be raised to a point within the cranium at a recumbent level of 45° and may therefore not be visible. The level of elevation often only becomes apparent in the upright position.
- Kussmaul's sign - paradoxical inspiratory elevation of the JVP.
- Diastolic apex beat.
- A right ventricular pericardial knock (Audio 2).
- Ascites that is more prominent than the degree of peripheral oedema.
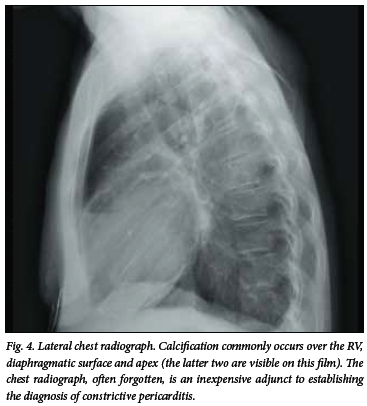
- A lateral chest radiograph can reveal pericardial calcification in up to 50% of patients with tuberculous constriction (Fig. 4).
- The clinical diagnosis can be confirmed by TTE, with tissue Doppler imaging aiding in both establishing the diagnosis and differentiating constriction from restrictive cardiomyopathy. An invasive left and right heart study is infrequently required, but is most useful to distinguish constriction from restrictive cardiomyopathy if doubt exists despite a detailed TTE.
- Early diagnosis leads to timelier referral for surgical pericardiectomy, thereby reducing perioperative mortality. This risk is as high as 15% in patients who already have a New York Heart Association class IV effort tolerance and/or hyponatraemia at the time of surgery.[28]
References
1. Zayas R, Anguita M, Torres F, et al. Incidence of specific etiology and role of methods for specific etiologic diagnosis of primary acute pericarditis. Am J Cardiol 1995;75(5):378-382. [http://dx.doi.org/10.1016/S0002-9149(99)80558-X] [ Links ]
2. Imazio M, Cecchi E, Demichelis B, et al. Myopericarditis versus viral or idiopathic acute pericarditis. Heart 2008;94:498-501. [http://dx.doi.org/10.1136/hrt.2006.104067] [ Links ]
3. Imazio M. Contemporary management of pericardial diseases. Curr Opin Cardiol 2012;27:308-317. [http://dx.doi.org/10.1097/HCO.0b013e3283524fbe] [ Links ]
4. Imazio M, Spodick DH, Brucato A, et al. Controversial issues in the management of pericardial diseases. Circulation 2010;121:916-928. [http://dx.doi.org/10.1161/CIRCULATIONAHA.108.844753] [ Links ]
5. Sliwa K, Mocumbi AO. Forgotten cardiovascular diseases in Africa. Clin Res Cardiol 2010;99:65-74. [http://dx.doi.org/10.1007/s00392-009-0094-1] [ Links ]
6. Imazio M, Bobbio M, Cecchi E, et al. Colchicine in addition to conventional therapy for acute pericarditis: Results of the COlchicine for acute PEricarditis (COPE) trial. Circulation 2005;112:2012-2016. [http://dx.doi.org/10.1161/CIRCULATIONAHA.105.542738] [ Links ]
7. Imazio M, Brucato A, Cemin R, et al. A randomised trial of colchicine for acute pericarditis. N Engl J Med 2013;369:1522-1528. [http://dx.doi.org/10.1056/NEJMoa1208536] [ Links ]
8. Mayosi BM, Ntsekhe M, Bosch J, et al Prednisolone and Mycobacterium indicus pranii in tuberculous pericarditis. N Engl J Med 2014;371:1121-1130. [http://dx.doi.org/10.1056/NEJMoa1407380] [ Links ]
9. Shabetai R. The Pericardium. Norwell, MA: Kluwer, 2003. [http://dx.doi.org/10.1007/978-1-4419-9137-9] [ Links ]
10. The Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC). 2015 ESC Guidelines for the diagnosis and management of pericardial diseases. Eur Heart J 2015;36(42):2921-1264. [http://dx.doi.org/10.1093/eurheartj/ehv318] [ Links ]
11. Imazio M, Demichelis B, Parrini I, et al. Day-hospital treatment of acute pericarditis: A management program for outpatient therapy. J Am Coll Cardiol 2004;43(6):1042-1046. [http://dx.doi.org/10.1016/j.jacc.2003.09.055] [ Links ]
12. Alraies MC, Klein AL. Should we still use electrocardiography to diagnose pericardial disease: Cleveland Clinic J Med 2013;80(2):97-100. [http://dx.doi.org/10.3949/ccjm.80a.11144] [ Links ]
13. Klein AL, Abbara S, Agler DA, et al. American Society of Echocardiography clinical recommendations for multimodality cardiovascular imaging of patients with pericardial disease: Endorsed by the Society for Cardiovascular Magnetic Resonance and Society of Cardiovascular Computed Tomography. J Am Soc Echocardiogr 2013;26:965-1012.e15. http://dx.doi.org/10.1016/j.echo.2013.06.023] [ Links ]
14. Imazio M, Adler Y. Management of pericardial effusion. Eur Heart J 2013;34:1186-1197. [http://dx.doi.org/10.1093/eurheartj/ehs372] [ Links ]
15. Imazio M, Brucato A, Maestroni S, et al. Prevalence of C-reactive protein elevation and time course of normailzation in acute pericarditis: Implications for the diagnosis, therapy and prognosis of pericarditis. Circulation 2011;123:1092-1097. [http://dx.doi.org/10.1161/CIRCULATIONAHA.110.986372] [ Links ]
16. Imazio M, Cecchi E, Demichelis B, et al. Myopericarditis versus viral or idiopathic acute pericarditis. Heart 2008;94:498-501. [http://dx.doi.org/10.1136/hrt.2006.104067] [ Links ]
17. Mayosi BM. Contemporary trends in the epidemiology and management of cardiomyopathy and pericarditis in sub-Saharan Africa. Heart 2007;93:1176-1183. [http://dx.doi.org/10.1136/hrt.2007.127746] [ Links ]
18. Imazio M, Cecchi E, Demichelis B, et al. Indicators of poor prognosis of acute pericarditis. Circulation 2007;115:2739-2744. [http://dx.doi.org/10.1161/CIRCULATIONAHA.106.662114] [ Links ]
19. Imazio M, Brucato A, Maestroni S, et al. Risk of constrictive pericarditis after acute pericarditis. Circulation 2011;124:1270-1275. [http://dx.doi.org/10.1161/CIRCULATIONAHA.111.018580] [ Links ]
20. Imazio M, Brucato A, Cemin R, et al. Colchicine for recurrent pericarditis (CORP): A randomised trial. Ann Intern Med 2011;155:409-414. [http://dx.doi.org/10.7326/0003-4819-155-7-201110040-00359] [ Links ]
21. Reuter H, Burgess LJ, Doubell AF. Epidemiology of pericardial effusions at a large academic hospital in South Africa. Epidemiol Infect 2005;133:393-399. [http://dx.doi.org/10.1017/S0950268804003577] [ Links ]
22. Maisch B, Ristic AD, Seferovic PM, et al. Interventional Pericardiology: Pericardiocentesis, Pericardioscopy, Pericardial Biopsy, Balloon Pericardiotomy and Intrapericardial Therapy. Heidelberg: Springer, 2011. [http://dx.doi.org/10.1007/978-3-642-11335-2] [ Links ]
23. Ainsworth CD, Salehian O. Echo-guided Pericardiocentesis: Let the bubbles show the way. Circulation 2011;123:e210-e211. [http://dx.doi.org/10.1161/CIRCULATIONAHA.110.005512] [ Links ]
24. Burgess LJ, Reuter H, Carstens ME, et al. The use of adenosine deaminase and interferon- as diagnostic tools for tuberculous pericarditis. Chest 2002;122:900-905. [http://dx.doi.org/10.1378/chest.122.3.900] [ Links ]
25. Reuter H, Burgess LJ, Louw VJ, Doubell AF. The management of tuberculous pericardial effusion: Experience in 233 consecutive patients. Cardiovasc J S Afr 2007;18(1):20-25. [ Links ]
26. Cui HB, Chen XY, Cui CC, et al. Prevention of pericardial constriction by transcatheter intrapericardial fibrinolysis with urokinase. Chin Med Sci J 2005;20:5-10. [ Links ]
27. Reuter H, Burgess LJ, Louw VJ, Doubell AF. Experience with adjunctive corticosteroids in managing tuberculous pericarditis. Cardiovasc J S Afr 2006;17:233-238. [ Links ]
28. Mutyaba AK, Balkaran S, Cloete R, et al. Constrictive pericarditis requiring pericardiectomy at Groote Schuur Hospital, Cape Town, South Africa: Causes and perioperative outcome in the HIV era (1990-2012). J Thorac Cardiovasc Surg 2014;148:3058-3065. [http://dx.doi.org/10.1016/j.jtcvs.2014.07.065] [ Links ]
 Correspondence:
Correspondence:
C G Kyriakakis
cgk@sun.ac.za
Audiofiles (headphones are required) and videoclips
Audio 1. Typical triphasic pericardial rub recorded in a patient with acute pericarditis.
Audio 2. Recording of a pericardial knock in a patient with constrictive pericarditis. The early diastolic knock is heard just after the second heart sound over the left sternal border, occurring earlier in diastole than an S3.
Video 1. Apical 4-chamber TTE image of a patient with a large pericardial effusion. Note the electrical alternans on the recorded ECG strip. As the heart swings to and fro within the fluid, the direction of the main vector of depolarisation changes from beat to beat, producing the ECG finding of electrical alternans.
Video 2. Pericardiocentesis in the emergency room. Before a 6-French sheath or central venous pressure line is inserted, the puncture needle is held in place and agitated saline bubble contrast injected to confirm one's position. Note the echobright saline bubbles within the pericardial space, which confirms that the operator has punctured the pericardial space and can safely proceed with the aspiration procedure.
Video 3. Apical 4-chamber TTE image (RV on left of image, LV on the right) in the same patient as in Fig. 3A and B. Note the simultaneous respirometer trace and bi-atrial dilatation. During inspiration the RV fills relatively more quickly than the LV owing to the degraded transmitral forward driving gradient. The result is respiratophasic septal shift into the LV.
Video 4. Rapid y-descents seen in the JVP of a patient with constrictive pericarditis. These are generally appreciated as rapid inward 'flicking' movements in the presence of an elevated JVP (co Dr Annari van Rensburg).














