Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.106 n.1 Pretoria Jan. 2016
http://dx.doi.org/10.7196/SAMJ.2016.V106I1.10215
RESEARCH
The socioeconomic and environmental health situation of international migrants in Johannesburg, South Africa
A MatheeI, II, III; N NaickerIV, V
IPhD; Environment & Health Research Unit, South African Medical Research Council, Johannesburg, South Africa
IIPhD; Environment Health, Faculty of Health Sciences, University of Johannesburg, South Africa
IIIPhD; School of Public Health Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IVMB BCh, FCPHM, MMed, PhD; Environment & Health Research Unit, South African Medical Research Council, Johannesburg, South Africa
VMB BCh, FCPHM, MMed, PhD; School of Public Health Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
BACKGROUND: Around the world, cities are dealing with growing numbers of international migrants (IMs). Many migrants are likely to have encountered exceptional challenges through the migration process, with implications for their health. Nevertheless, studies conducted in several developed countries point to a pattern of better health in migrant groups - the 'healthy migrant' effect. However, little is known about the health of migrants in poorly resourced destination countries, especially in African settings.
OBJECTIVES: To compare living conditions and environmental health status in IMs relative to South African (SA) households, both living in settings of poverty in Johannesburg, SA.
METHODS: Data were extracted from a long-term panel study underway in five neighbourhoods of Johannesburg. Cross-sectional studies, undertaken annually from 2006 to 2010, involved the annual administration of questionnaires to around 500 households to obtain information on living conditions and health.
RESULTS: Most of the differences observed through univariate analyses in living conditions and health status between IM and SA households were explained by controlling for socioeconomic and neighbourhood factors.
CONCLUSION: This study revealed that SA respondents and IMs in settings of urban poverty in Johannesburg had remarkably similar health status, with little evidence of a 'healthy migrant' effect. Nevertheless the authors argue for vigilance and a finer understanding of the unique sociocultural dimensions of health in migrant communities in Johannesburg as they continue to transform the profile of urban health in SA and other African cities.
International migrants (IMs) constitute a groupof growing proportion and importance in cities around the world. Many migrants are likely to have encountered exceptional challenges through the migration process, which may have implications for their health in the short or longer term. For example, they may have needed to adapt to a foreign local culture and a new urban system and language, and may have experienced trauma in their country of origin.[1] Under certain circumstances, migrants may encounter poverty, marginalisation and exclusion, or even a hostile reception in their destination country. In 2008, for example, a wave of xenophobic violence swept across South Africa (SA), resulting in the deaths of 62 IMs, injury to 670, and the displacement of around 100 000.[2]
Notwithstanding the recognised challenges associated with migration, studies conducted in several parts of the world point to a pattern of better health in migrant groups. While uncertainty continues to prevail in this regard, postulated explanations include the 'healthy migrant' effect (those who migrate are healthier than their counterparts who remain),[3] 'salmon bias' (migrants return to their home countries on retirement or becoming seriously ill),[4] and the 'best of both worlds' (the continuation or preservation of traditional behaviours favourable to health, family support and better access to healthcare).[5] For example, a study undertaken in the USA showed lower levels of psychiatric disorders in immigrants compared with locally born residents.[6] In Germany, it was shown that Eastern European immigrants had higher levels of 'health satisfaction' than their counterparts of local origin.[7] In further studies, migrant groups have been shown to have lower levels of mortality, chronic conditions and mental ill health.[8] The health advantage in certain migrant groups has, however, been shown to decline over time.[7]
The city of Johannesburg, SA, is characterised by high degrees of diversity and inequality, including diversity and inequality in respect of socioeconomic status, living conditions, culture and lifestyle. The observed inequalities are in part associated with the implementation over several decades of racially differentiated economic and development policies, resulting in SA currently having among the highest Gini coefficients (a measure of economic inequality) in the world. Despite the prevailing poverty and inequality, since the dissolution of apartheid SA, and Johannesburg in particular, has attracted large numbers of refugees and economic migrants from elsewhere on the African continent, further diversifying the city's population and garnering the description of a cultural melting pot.[9]
Despite the increasing size of the IM population in Johannesburg, few household-level studies have been conducted to gain a deeper understanding of the situation and health needs of this subgroup of the city's population. The primary focus of most health-related studies conducted to date has been IMs' access to, and treatment in, local health services.[10] In 2006, the World Health Organization (WHO) Collaborating Centre for Urban Health (a partnership of the South African Medical Research Council, the University of Johannesburg, the University of the Witwatersrand and the City of Johannesburg) initiated a study (the Health, Environment and Development (HEAD) study) of indicators of living conditions and health status in five sites of relative impoverishment in Johannesburg. Three of the five study sites (Hillbrow, Bertrams and Hospital Hill) house significant proportions of IMs. In this article, HEAD study data from these sites are used to describe the environmental health situation of IMs in relation to their SA counterparts.
Methods
The data used in the preparation of this article were extracted from the Johannesburg-based HEAD study. The HEAD study is a long-term panel study involving the administration of prestructured questionnaires to respondents from households living in a predetermined set of dwellings in five relatively impoverished neighbourhoods: Hillbrow, Bertrams, Riverlea Extension 1, Braamfischerville and Hospi- tal Hill. At the start of the study in 2006, participating dwellings were randomly selected in the suburbs of Bertrams, Riverlea and Braamfischerville, conveniently sampled in Hospital Hill (an informal settlement for which no town planning maps were available), and systematically sampled in the high-rise suburb of Hillbrow (buildings, followed by floors and then apartments, were randomly selected). In each neighbourhood around 50% of dwellings were targeted for inclusion in the study. Data on, for example, socioeconomic status, place of birth, living conditions, health status, quality of life and perceptions of neighbourhood infrastructure and services were collected during August each year. Data were collected from 2006 to 2010. Respondents aged at least 18 years from the main or primary household on the dwelling site, from whom prior written informed consent had been obtained, were interviewed. Households were defined as a group of people eating meals together. Interviews were conducted by environmental health students from the University of Johannesburg, who had been trained in interviewing techniques and fieldwork processes.
IMs were defined as having been born beyond SA borders. The status of the respondent (international migrant or SA native) was defined as the status of the household. To obtain an indicator of socioeconomic status, respondents were asked about ownership of a set of household commodities - such as a telephone, refri- gerator, motor vehicle, microwave oven and satellite television - and the arithmetical mean was calculated. Data were analysed using the Stata version 9 statistical package. Analyses were conducted in survey mode and weighted for area. Ethical clearance for the study was obtained from the University of the Witwatersrand Human Research Ethics Committee (Medical) (Ref. No. MO50451).
Results
Over the 5-year period of the study, the total proportion of respondents who reported having been born outside SA remained relatively constant: 18.4%, 22.0%, 23.3%, 26.0% and 22.0%, respectively, for the years 2006 - 2010 (p=0.18, non-parametric (NP) test for trend) (Fig. 1). At the suburb level, there was also no significant change in the proportion of IM households in Hospital Hill and Bertrams over the 5 years (p=0.71 and p=0.28, χ2). In Hillbrow, however, the proportion of IM households increased from 30.0% in 2006 to 47.0% in 2010, a statistically significant increase (p=0.04). The vast majority of IM households were Zimbabwean, with smaller proportions having migrated from a range of African countries including Malawi, Nigeria, Zambia, Ethiopia, Mali, Kenya, Somalia, Lesotho, Mozambique, Uganda, the Democratic Republic of the Congo, Ivory Coast, Rwanda and the Republic of the Congo.

IM households were not evenly distributed across the five HEAD study sites (p<0.01). As shown in Fig. 2, relative to Hillbrow and Bertrams, very few households in Riverlea and Braamfischerville were of international origin. Over the 5-year period of the study, the data showed that, on average, 41% of households in Hillbrow were of international origin, while the proportions for Bertrams and Hospital Hill were 20% and 10.0%, respectively. Given the very low numbers of IM households in Riverlea (2%) and Braamfischerville (1%) (Fig. 2), these sites were excluded from further analysis.

Household characteristics
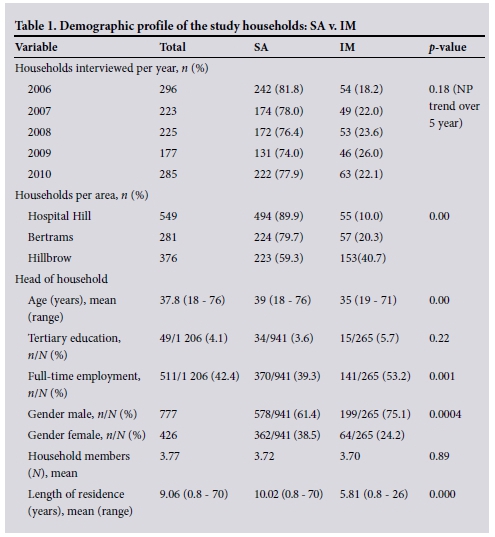
Both SA and IM households comprised around four members. The average age of the heads of SA households was 39 years (range 18 - 76 years), while that for the heads of IM households was 35 (19 - 71) years. More IM (75%) than SA households (61%) were headed by men (p=0.0004). Educational status was low in both groups, with 6% of the heads of IM households having a tertiary education compared with 4% in SA households (p=0.215). However, significantly more IM (53%) than SA (39%) household heads were employed on a full- time basis (p=0.001) (Table 1).
Indicators of socioeconomic status
Table 2 gives a breakdown by migration status of a range of indicators of socio- economic and environmental health status in Hillbrow, Bertrams and Hospital Hill. As can be seen, from an economic perspective IM households appeared to be better off than their local counterparts. More IM relative to SA households earned relatively high incomes and fewer earned very low incomes. Over the study period, there was no statistically significant increase in IM or SA household incomes (NP trend: IM p=0.48, SA p=0.23 for low incomes and IM p=0.40, SA p=0.41 for high incomes). On average IM households also owned more commodities (such as refrigerators, microwave ovens, dishwashing machines, motor vehicles, computers, telephones, etc.) than SA households (4.4 v. 3.9, respectively) (p=0.003). IMs spent more on, and lived in, housing of a higher standard. For example, a higher proportion of IM households lived in dwellings with indoor taps and used electricity for daily cooking. There was a lower level of concern among IM households over food insecurity, and a higher regard for the health and police services in their neighbourhoods (Table 2). Only average commodity ownership (p=0.012) and the average perception of police (p=0.003) and health services (p=0.000) remained significantly different after controlling for area of residence.
As can be seen from Table 3, univariate analyses in respect of the total sample indicated that the prevalences of diseases of lifestyle (diabetes, hypertension, and stroke) were significantly higher in SA relative to IM households. SA households were also more likely to have a household member die (using a 1-year recall period) and to have children miss school because of illness. Multivariate analyses illustrated the importance of socioeconomic status and the areas or neighbourhoods in which households lived - after controlling for these aspects, there were no statistically significant health differences between SA and IM households. The health status of SA and IM households neither improved nor declined over the study period.

Table 4 gives further evidence of the role of neighbourhood and socioeconomic status in comparisons of the health of local and migrant communities. It gives a comparative breakdown of the socio- environmental characteristics of IM households in the informal settlement of Hospital Hill relative to those living in the inner-city neighbourhoods of Hillbrow and Bertrams, combined. As can be seen, there were significant differences between the two groups of IMs in respect of socioeconomic factors, environmental conditions and perceptions of local services. Similar differences were observed among SA citizens living in different neighbourhoods.
Discussion
Migration, national and international, is a phenomenon of growing importance for countries around the world, and may increase as the spectre of climate change unfolds.[11] While numerous studies of the health status of IMs have been undertaken in relatively wealthy recipient countries such as the USA and various European countries, there is a paucity of similar information available for African settings. This is especially the case for international, intra-African migration, for which there is a particular dearth of information. Our research seeks to address this gap, providing information on the environmental health situation of intra-African migrants living in three relatively impoverished neighbourhoods in Johannesburg. Overall, as a proportion of the total study sample across five neighbourhoods, the IM population remained stable in the study settings over the study period. However, population changes could be observed at the neighbourhood level. For example, in the sample from the inner-city, high-rise residential area of Hillbrow, the proportion of IMs increased from 31% to 46% over the 5-year study period. Hillbrow has an established reputation as a magnet for new migrants to the city, both national and international. In contrast, the proportion of IM households in the study suburbs of Riverlea and Braamfischerville remained low and static throughout the study period. This clustering in particular neighbourhoods may indicate the value of social networks and cultural familiarity to IMs on arrival in their adoptive country.
Crude analyses of the socioenvironmental health status of the two groups indicated a number of differences between SA and IM households, including differences in respect of economic status, living conditions, food security and health status (chronic ill-health conditions, common mental disorders, school absenteeism and mortality levels). However, multivariate analyses showed that differences in socioeconomic status and area of residence accounted for most of the variance observed. After socioeconomic status and area of residence were controlled for, the health of IMs was similar to that of SA households in respect of all parameters studied. The only differences that remained statistically significant were the higher level of ownership of household commodities and the higher regard among IMs for local health and police services. Instead, statistically significant differences in socioeconomic and living conditions were shown among IMs living in different Johannesburg neighbourhoods.
The absence of a higher level of health (this was the case in respect of indicators of chronic diseases, mental ill health, and communicable and acute ill health, as well as indicators of exposure to violence) in IMs (even though around 80% of respondents reported having lived in SA for less than 5 years) relative to locals in this study is unexpected. Studies undertaken in other parts of the world have often shown that migrants enjoy better health than non- migrants,[3] albeit for a limited period.[7] In this study the vast majority of IMs originated from SA's immediate northern neighbour, Zimbabwe. The relatively short distance between the countries, low cost of travel, porous national borders and relatively easy access to existing social networks at the destination may make the contemplation and act of migration possible for a relatively broad socioeconomic and health cross-section of Zimbabwean citizens (and other Africans), while the process of migration from African countries to locations such as the USA or European countries may be considerably more challenging in terms of cost, social support at the point of destination and stringent immigration policies. Intra- African migration may therefore not be as self-selecting of high levels of health as is the case in those migrating from Africa to destinations in developed countries, which may have contributed to the absence of or a narrower gap in health status (i.e. the absence of the healthy migrant effect) between migrants and locals in the destination country, such as shown in the current study.
Notwithstanding the lack of stark differences in health status between native and migrant communities observed in this study, vigilance and further research to gain a deeper understanding of the unique health needs of migrant communities in SA is warranted, in part because IMs now constitute the majority population in certain neighbourhoods. In this study for example, IMs at times comprised up to 54% of the study sample in Hillbrow, and their health status and unique health needs are therefore of increasing importance in the SA urban health landscape. There are other compelling reasons for gaining a finer understanding of the health needs of IM populations; a recent study in Johannesburg of the prevalence of geophagia in pregnant women showed that around one-fifth of the sample were IMs, and that the level of geophagia in this group was twice as high as that among SA women (17% in women born in SA v. 32% in IMs).[12] Geophagia is associated with an increased risk of intestinal obstruction, lead exposure (both maternal and fetal) and anaemia, yet the current antenatal health screening tool in SA excludes a history of pica or geophagia. This and other aspects of the health system may need to change to respond more effectively to the health needs and status of SA urban populations as they are transformed by international, as well as national, migration in a longer-term process of urbanisation.
Study strengths and limitations
There is a particular paucity of data on international migration and health in Africa, and this study helps to fill that gap.
Xenophobic violence may have been responsible for low response rates in two of the study sites in some years, resulting in bias. Data were collected on a household rather than individual level, and as a result the study does not provide information on individual risk factors or consequences of migration. It is possible that health information may have been under-reported because respondents were not fully aware of the health histories of all household members. This study is prone to the weaknesses generally associated with studies of a cross-sectional design. In this study households were regarded as IM households if the respondent had been born outside SA. Given that a degree of integration might have occurred, an IM respondent does not necessarily imply that the entire household comprised migrants. Hillbrow and Bertrams are unusual inner-city settings in Johannesburg, and the findings may not be representative of the situation of communities in other SA cities.
Conclusions
This study has revealed that on average, and taking account of differences in area and socioeconomic status, the living conditions and health status of SA and IM households are remarkably similar, showing little evidence of a healthy migrant effect. Despite this, the authors argue for increased research aimed at achieving a deeper understanding of the unique sociocultural dimensions of health in migrant communities as they continue to transform the profile of urban health in SA and African cities.
Acknowledgements. The authors are grateful to the respondents for granting permission to be interviewed.
Funding. The study was funded by the South African Medical Research Council, the South African National Research Foundation and the University of Johannesburg.
References
1. Pernice R, Brook J. Relationship of migrant status (refugee or immigrant) to mental health. Int J Soc Psychiatry 1994;40(3):177-188. [ Links ]
2. Kapp C. South Africa failing people displaced by xenophobia riots. Lancet 2008;371(9629):1986-1987. [http://dx.doi.org/10.1016/S0140-6736(08)60852-1] [ Links ]
3. Khlat M, Darmon N. Is there a Mediterranean migrants mortality paradox in Europe? Int J Epidemiol 2003;32(6):1115-1118. [http://dx.doi.org/10.1093/ije/dyg308] [ Links ]
4. Abraido-Lanza A, Dohrenwend B, Ng-Mak D, et al. The Latino mortality paradox: A test of the 'salmon bias' and healthy migrant hypotheses. Am J Public Health 1999;89(10):1543-1548. [http://dx.doi.org/10.2105/AJPH.89.10.1543] [ Links ]
5. Powles J. The best of both worlds: Attempting to explain the persisting low mortality of Greek migrants to Australia. In: Caldwell J, Findley S, Caldwell P, et al., eds. What We Know about The Health Transition: The Cultural, Social and Behavioural Determinants of Health. Canberra: Health Transition Centre, 1990:584-594. [ Links ]
6. Breslau J, Aguilar-Gaxiola S, Borges G, et al. Risk for psychiatric disorder among immigrants and their US-born descendants: Evidence from the National Comorbidity Survey Replication. J Nerv Ment Dis 2007;195(3):189-195. [http://dx.doi.org/10.1097/01.nmd.0000243779.35541.c6] [ Links ]
7. Ronellenfitsch U, Razum O. Deteriorating health satisfaction among immigrants from Eastern Europe to Germany. Int J Equity Health 2004;3(1):4. [http://dx.doi.org/10.1186/1475-9276-3-4] [ Links ]
8. Lu Y. Test of the 'healthy migrant hypothesis': A longitudinal analysis of health selectivity of internal migration in Indonesia. Soc Sci Med 2008;67(8):1331-1339. [http://dx.doi.org/10.1016/j.socscimed.2008.06.017] [ Links ]
9. Van der Berg S. Inequality, poverty and prospects for redistribution. Development Southern Africa 2014;31(2):197-218. [http://dx.doi.org/10.1080/0376835X.2013.871196] [ Links ]
10. Vearey J. Migration, access to ART, and survivalist livelihood strategies in Johannesburg. African Journal of AIDS Research 2008;7(3):361-374. [http://dx.doi.org/10.2989/AJAR.2008.7.3.13.660] [ Links ]
11. Zimmerman C, Kiss L, Hossain M. Migration and health: A framework for 21st century policy- making. PLoS Med 2011;8(5):e1001034. [http://dx.doi.org/10.1371/journal.pmed.1001034] [ Links ]
12. Mathee A, Naicker N, Kootbodien T, et al. A cross-sectional analytical study of geophagia practices and blood metal concentrations in pregnant women in Johannesburg, South Africa. S Afr Med J 2014;104(8):568-573. [http://dx.doi.org/10.7196/SAMJ.7466] [ Links ]
 Correspondence:
Correspondence:
A Mathee
amathee@mrc.ac.za
Accepted 23 October 2015.














