Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.105 no.10 Pretoria Out. 2015
http://dx.doi.org/10.7196/SAMJNEW.8788
CONTINUING MEDICAL EDUCATION
CASE REPORT
The real value of endobronchial ultrasound
M J VorsterI; P T SchubertII; C F N KoegelenbergIII
IMB ChB, MRCP (UK), FCP (SA); Division of Pulmonology, Department of Medicine, Faculty of Medicine and Health Sciences, Stellenbosch University and Tygerberg Academic Hospital, Cape Town, South Africa
IIMB ChB, FCPath (Anat) (SA), MMed, MScMedSc, MPhil, MIAC; Division of Anatomical Pathology, Department of Pathology, Faculty of Medicine and Health Sciences, Stellenbosch University and National Health Laboratory Service, Tygerberg Hospital, Cape Town, South Africa
IIIMB ChB, FCP (SA), FRCP (UK), PhD; Division of Pulmonology, Department of Medicine, Faculty of Medicine and Health Sciences, Stellenbosch University and Tygerberg Academic Hospital, Cape Town, South Africa
ABSTRACT
Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) has become a standard procedure worldwide, used in conjunction with bronchoscopy to obtain biopsies for mediastinal disorders.
A 67-year-old man with a 40 pack-year smoking history presented with a 2-year history of hoarseness and weight loss. He also had a history of asbestos exposure. On examination under anaesthesia a lesion of the right false vocal fold was found and histology showed a moderately differentiated infiltrating keratinising squamous carcinoma. The question posed was whether this mass could be ascribed to metastatic supraglottic carcinoma or if it was indeed a metachronous primary bronchus carcinoma, as the treatment of these two malignancies differs significantly. Traditional bronchoscopy with TBNA is the least invasive procedure to obtain a cytological diagnosis, but the proximity of the aorta and pulmonary arteries and the mass being 14 mm from the bronchus would have made sampling by means of this procedure near impossible. We used EBUS to localise the mass and noted the position of the major vessels on Doppler ultrasound. Real-time ultrasound guidance allowed us to bridge the tissue plane between the mass and bronchial lumen using the longer EBUS needle and to obtain a fine-needle aspirate of the mass, which proved to be a keratinising squamous carcinoma. We describe this case in which EBUS-TBNA was pivotal in reducing the number of invasive procedures in a patient with metastatic supraglottic carcinoma.
Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) has become a standard procedure worldwide, used in conjunction with bronchoscopy to obtain biopsies for mediastinal disorders. We describe a case where EBUS-TBNA was pivotal in reducing the number of invasive procedures in a patient with metastatic supraglottic carcinoma.
Case report
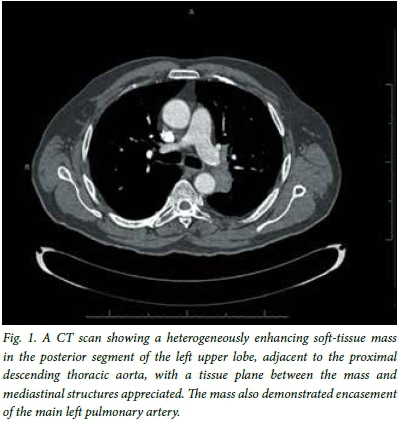
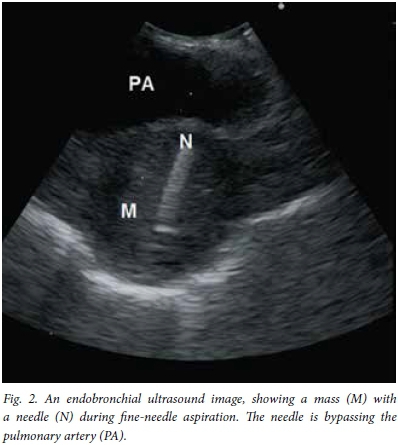
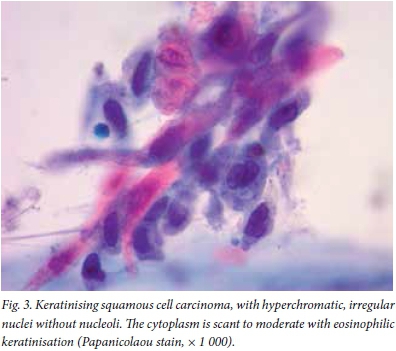
A 67-year-old man with a 40 pack-year smoking history presented with a 2-year history of hoarseness and weight loss. He also had a history of asbestos exposure. On examination under anaesthesia a lesion of the right false vocal fold was found and histology showed a moderately differentiated infiltrating keratinising squamous carcinoma. A subsequent computed tomography (CT) scan provisionally staged his supraglottic carcinoma as T2N0M0 and he underwent radical treatment with external beam radiation therapy, to which he responded well. He had been attending our clinic regularly and remained well, but on a visit 4 years later possible recurrence was considered - with hilar lymphadenopathy noted on his chest radiograph. On the CT scan of his chest there was a heterogenously enhancing soft-tissue mass (42 mm x 30 mm) in the posterior segment of the left upper lobe, adjacent to the proximal descending thoracic aorta, with a tissue plane between the mass and mediastinal structures appreciated. The mass demonstrated encasement of the left main pulmonary artery (Fig. 1). There was also a left diaphragmatic calcified plaque. The question posed was whether this mass could be ascribed to metastatic supraglottic carcinoma or if it was indeed a metachronous primary bronchus carcinoma, as the treatment of these two malignancies differs significantly. Considering traditional bronchoscopy with TBNA as the least invasive procedure to obtain a cytological diagnosis, the proximity of the aorta and pulmonary arteries and the mass being 14 mm from the bronchus would have made sampling by means of this procedure near impossible. With the assistance of EBUS the mass was localised, despite it not abutting the bronchus, and the position of the major vessels duly noted on Doppler ultrasound. Under real-time ultrasound guidance (Fig. 2) the tissue plane between the mass and bronchial lumen could be bridged by the longer EBUS needle to traverse safely between the major vessels, a window of <10 mm, and obtain a fine-needle aspirate of the mass. The result, which proved to be a keratinising squamous carcinoma (Fig. 3), was most likely of supraglottic origin. The patient was discharged the same day, with a follow-up appointment to see an oncologist.
Discussion
Conventional TBNA (cTBNA) has a history of >3 decades of use for mediastinal sampling in lung cancer, especially in more bulky disease. Traditionally, patients presenting with mediastinal lymphadeno-pathy would undergo conventional bronchoscopy and TBNA done blindly, while reserving mediastinoscopy for cases where cTBNA failed to elucidate a final diagnosis. There is now increased use of EBUS-TBNA, whereby needle aspirations are no longer done blindly but under real-time ultrasound guidance. There are two types of EBUS probes: the radial probe EBUS (RP-EBUS) and convex probe EBUS (CP-EBUS). RP-EBUS provides 360° images of the airway wall and surrounding structures. The major advantage of RP-EBUS is its ability to visualise the layers of the airway wall in detail. CP-EBUS provides a view parallel to the shaft of the bronchoscope - the angle of view is 90° and the direction of view is 30° forward oblique. Colour flow and Doppler features permit identification of vascular, ductular, and cystic structures. The major advantage of CP-EBUS is its ability to guide real-time sampling. The dedicated 22-gauge needle has an echogenic dimpled tip to enhance visibility on ultrasound. The maximum extruding stroke is 40 mm, with a safety mechanism that stops at 20 mm. The needle has an internal sheath, which prevents contamination of the sample by bronchial wall tissue.
EBUS has now become an established practice in many centres as the first-line mediastinal investigation for the diagnosis and staging of lung cancer.[1] In combination with endoscopic ultrasound the major part of the mediastinum can be assessed; this approach has been shown to be as accurate as surgical staging.[1] This strategy is also cost-effective.[1] EBUS-TBNA has been demonstrated to be a safe[2] and valuable diagnostic tool in lung cancer,[3] sarcoidosis,[4] tuberculosis[5] and lymphoma.[6]
In our patient, the value of EBUS was threefold: (i) the technique is minimally invasive and safe compared with a surgical procedure; (ii) it was used to localise the lesion not abutting the bronchial wall and the proximity of major vessels, precluding conventional bronchoscopy; and (iii) the longer EBUS needle was used owing to the depth of the lesion.
References
1. Rintoul RC, Ahmed R, Dougherty B, Carroll NR. Linear endobronchial ultrasonography: A novelty turned necessity for mediastinal nodal assessment. Thorax 2015;70(2):175-180. [http://dx.doi.org/10.1136/thoraxjnl-2014-205635] [ Links ]
2. Agarwal R, Srinivasan A, Aggarwal AN, Gupta D. Efficacy and safety of convex probe EBUS-TBNA in sarcoidosis: A systematic review and meta-analysis. Respir Med 2012;106(6):883-892. [http://dx.doi.org/10.1016/j.rmed.2012.02.014] [ Links ]
3. Hwangbo B, Lee GK, Lee HS, et al. Transbronchial and transesophageal fine-needle aspiration using an ultrasound bronchoscope in mediastinal staging of potentially operable lung cancer. Chest 2010;138:795-802. [http://dx.doi.org/10.1378/chest.09-2100] [ Links ]
4. Tremblay A, Stather DR, MacEachern P, Khalil M, Field SK. A randomized controlled trial of standard vs endobronchial ultrasonography-guided transbronchial needle aspiration in patients with suspected sarcoidosis. Chest 2009;136:340-346. [http://dx.doi.org/10.1378/chest.08-2768] [ Links ]
5. Navani N, Molyneaux PL, Breen RA, et al. Utility of endobronchial ultrasound-guided transbronchial needle aspiration in patients with tuberculous intrathoracic lymphadenopathy: A multicentre study. Thorax 2011;66(10):889-893. [http://dx.doi.org/10.1136/thoraxjnl-2011-200063] [ Links ]
6. Steinfort DP, Conron M, Tsui A, et al. Endobronchial ultrasound-guided transbronchial needle aspiration for the evaluation of suspected lymphoma. J Thorac Oncol 2010;5:804-809. [http://dx.doi.org/10.1097/JTO.0b013e3181d873be] [ Links ]
Corresponding author: M J Vorster (mvorster@sun.ac.za)














