Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.105 n.10 Pretoria Oct. 2015
http://dx.doi.org/10.7196/SAMJNEW.8329
RESEARCH
Self-expanding metal stent placement for oesophageal cancer without fluoroscopy is safe and effective
M GovenderI; C AldousII; L FerndaleIII; S R ThomsonIV; D L ClarkeV
IFCS (SA); Department of Surgery, Pietermaritzburg Metropolitan Complex and College of Health Sciences, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
IIPhD; School of Clinical Medicine, College of Health Sciences, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
IIIMMedSci; Department of Surgery, Pietermaritzburg Metropolitan Complex and College of Health Sciences, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
IVMD, FRCS; Gastrointestinal Unit, Department of Internal Medicine, Faculty of Health Sciences, University of Cape Town, South Africa
VPhD; Department of Surgery, Pietermaritzburg Metropolitan Complex and College of Health Sciences, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
ABSTRACT
BACKGROUND: Self-expanding metal stents (SEMS) are widely used to palliate patients with oesophageal cancer. Placement is usually done under endoscopic and fluoroscopic guidance. We have developed an exclusively endoscopic technique to deploy these stents. This article documents the technique and periprocedural experience.
Patients and methods: All patients who had SEMS placement for oesophageal cancer at Grey's Hospital, Pietermaritzburg, South Africa, over a 5-year period (2007 - 2011) were reviewed. Stenting was performed without radiological guidance using the technique documented in this article. At endoscopy, the oesophageal lesion was identified, dilated over a guidewire if necessary, and a partially covered stent was passed over the wire and positioned and deployed under direct vision. Data were captured from completed procedure forms and included demographics, tumour length, the presence of fistulas, stent size and immediate complications.
RESULTS: A total of 480 SEMS were inserted, involving 453 patients, of whom 43 required repeat stenting. There were 185 female patients (40.8%) and 268 male patients (59.2%). The mean age was 60 years (range 38 - 101). There were 432 black patients (95.4%), 15 white patients (3.3%) and 6 Indian patients (1.3%). The reasons for palliative stenting were distributed as follows: age >70 years n=95 patients, tumour >8 cm n=142, tracheo-oesophageal fistula (TOF) n=29, and unspecified n=170. One patient refused surgery, and one stent was placed for a post-oesophagectomy leak. Repeat stenting was for stent migration (n=15), tumour overgrowth (n=26) and a blocked stent and a stricture (n=1 each). Complications were recorded in six cases (1.3%): iatrogenic TOF (n=2), false tracts (n=3) and perforation (n=1). All six were nevertheless successfully stented. There was no periprocedural mortality.
CONCLUSION: The endoscopic placement technique described is a viable and safe option with a low periprocedural complication rate. It is of particular use in situations of restricted access to fluoroscopic guidance.
Although the 5-year survival rate for oesophageal cancer has improved from 5% to 19% over the past 4 decades, the prognosis remains poor.[1-3] This is especially so in rural South Africa (SA), where patients present with advanced disease and therapy is typically directed at alleviating dysphagia, overflow of saliva, pulmonary aspiration and tracheo-oesophageal fistula. Over the past decade self-expanding metal stents (SEMS) have replaced surgical bypass and rigid plastic stents as the gold standard for mechanical palliation of this disease. Studies have shown good relief of dysphagia with SEMS insertion, with minimal risk.[4,5] In SA and in other countries, SEMS insertion is currently usually performed under fluoroscopic guidance, which requires access to a fluoroscopic suite. At Grey's Hospital in Pietermaritzburg, KwaZulu-Natal Province, SA, fluoroscopy is under great demand. We are also faced with a significant burden of inoperable oesophageal cancer. In response to this high demand for a limited resource, we developed an alternative direct-vision approach that does not require fluoroscopy. This technique, first described in the literature in 2001,[6] has been validated with several small studies in equally resource-constrained environments.[7-9] This study at Grey's Hospital was undertaken to describe the technique of stent placement using endoscopy alone and to document our periprocedural experience over a 5-year period (2007 - 2011). We hope that this alternative direct-vision approach will gain acceptance in the SA context, leading to more centres providing the service and ultimately improving patient access.
Methods
This was a retrospective analysis of all patients stented for oesophageal cancer at Grey's Hospital over the 5-year period 2007 - 2011. Data were analysed from completed gastrointestinal procedure reports and included patient demographics, tumour length, presence of a fistula, stent size used and immediate complications. Other variables included the indication for stenting, as well as the need and indication for repeat stenting during the study period.
Technique
All patients gave consent for the endoscopy, dilatation and stenting using a standard hospital consent form. Patients were counselled in the appropriate language before the procedure regarding the dietary modifications that the stent would mandate. All stenting was performed in the gastrointestinal unit, under sedation using midazolam and fentanyl. The stents used were nitinol partially covered ones with a proximal release mechanism (Ultraflex; Boston Scientific, USA). An initial gastroscopy was performed and the oesophageal tumour identified. If the endoscope could be passed beyond the tumour, proximal and distal measurements of the tumour were taken. If the scope could not initially traverse the lesion, a guidewire was passed and the lesion dilated using Savary-Gilliard dilators up to 12 mm diameter. The scope was then reintroduced and tumour measurements obtained. These were then used to select the stent size. Optimal stent size is at least 4 cm longer than tumour length in order to achieve adequate proximal and distal coverage (of 2 cm on either side of the lesion). The guidewire was then inserted under vision beyond the tumour into the stomach, and the scope was removed.
The stent delivery system, which has markings in centimetres, was then passed over the guidewire and positioned using the proximal tumour measurement as a guide. The scope was then reinserted alongside the stent delivery system and the SEMS carefully deployed under direct vision, allowing for adjustment of its position. Following the procedure, the patient recovered in the day ward unless a complication occurred. Once the patient was awake, advice regarding dietary modification was repeated. The patient was discharged with analgesia and a diet sheet back to his/her referral hospital or, in the case of inpatients, back to the ward. Fig. 1 is a photo montage of the technique of SEMS deployment.

Results
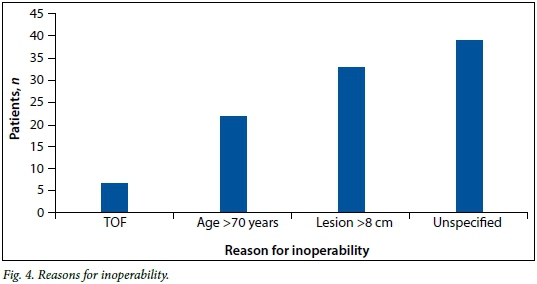
A total of 506 stents were placed in 453 patients between 2007 and 2011. Fig. 2 shows a breakdown of the numbers of procedures per year. There were 436 treatment-naive patients and 43 in whom a pre-existing SEMS had become obstructed and who required a salvage procedure. The mean age was 60 years, with the youngest patient being 38 and the oldest 101. There were 185 female patients (40.8%) and 268 male patients (59.2%). In terms of racial distribution (Fig. 3), black patients overwhelmingly predominated. The reasons for stenting were refusal of surgery (n=1), post-oesophagectomy leak (n=1), and inoperable cancer in the remainder. Six percent of patients presented with a tracheo-oesophageal fistula (TOF). Twenty-two percent of patients were older than 70 years, 32.7% had tumours that were >8 cm in length, and 39.4% (170/453) were deemed inoperable owing to comorbidities, locally advanced tumours and the presence of metastases. The reasons for irresectability are depicted in Fig. 4.


Repeat procedures
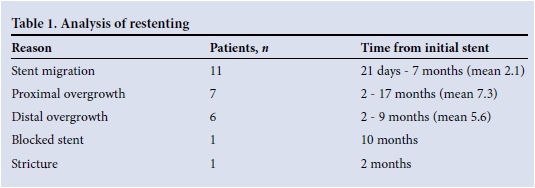
A total of 43 patients required a repeat procedure, 15 for stent migration, 26 for tumour overgrowth, 1 for a blocked stent and 1 for a stricture. Of the 436 new patients, 26 required restenting, giving a restent rate of 5.9%; an analysis of this subset is shown in Table 1. Restenting in all patients was uneventful. Six periprocedural complications (1.3%) occurred and included iatrogenic TOF (n=2), false tracts created through long tumour (n=3) and a single tumour perforation. All were successfully restented without the use of fluoroscopy, and there was no periprocedural mortality.
Discussion
The burden of disease due to oesophageal cancer in SA is large. This 5-year study reveals a significant number of patients with advanced oesophageal cancer who required palliation. In keeping with available epidemiological data, there was a male predominance and older patients were in the majority, although 15.3% of the patients were <50 years of age. Oesophageal stent placement is usually performed under fluoroscopic guidance in most centres in SA. We set out to show that the purely endoscopic technique of SEMS placement is a safe and effective alternative in the palliation of malignant dysphagia. Oesophageal SEMS insertion forms the core of palliation in patients in whom curative resection is not possible because they are too old or frail or because lesions are too advanced or extensive. In our series, 21.9% of patients were >70 years old (a local cut-off for oesophagectomy), and the rest had locally advanced or metastatic disease or were generally in a poor cachetic condition. Delays in seeking medical attention, as well as the lack of awareness of oesophageal cancer in our communities, probably contribute significantly to the advanced stage of disease at presentation.
This study suggests that an exclusively endoscopic technique is a safe and effective alternative to fluroscopically guided placement in a resource-limited setting. Accurate placement of stents was confirmed in 100% of our patients with endoscopic evaluation at the time of stent deployment. This was true for palliating dysphagia as well as for stenting over malignant TOF. Our recorded complication rates with respect to perforation, need for a salvage procedure due to stent migration and/or tumour overgrowth compare favourably with other published series utilising both the fluoroscopically guided and purely endoscopic technique.[7,10-14] Tables 2 and 3 compare our outcomes with those reported in the literature.


Currently we reserve fluoroscopic placement for a select group of patients. These include patients in whom complete luminal obstruction makes safe passage of either the endoscope or the guidewire impossible. Such patients comprise about 15 - 20% of cases at our institution. The direct-vision approach allows for the majority of patients to be stented at a regional level and selects out those for whom fluoroscopy would be necessary. Use of routine fluoroscopy for all patients therefore appears to be a waste of a valuable resource, as well as contributing to an unnecessary delay in patient management.
Conclusion
We have developed a safe technique to accurately deploy SEMS under direct vision, thus obviating the need for fluoroscopy. Our study shows that the periprocedural complication rate is low and reaffirms that the exclusively endoscopic technique of stent insertion is a safe and effective option, especially in units with limited or no access to fluoroscopy. This technique is also applicable to patients with recurrent dysphagia (whether due to stent migration or tumour overgrowth) and to the management of malignant TOF.
References
1. Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin 2012;62(1):10-29. [http://dx.doi.org/10.3322/caac.21149, http://dx.doi.org/10.3322/caac.20138, http://dx.doi.org/10.3322/caac.21153] [ Links ]
2. Dubecz A, Gall I, Solymosi N, et al. Temporal trends in longterm survival and cure rates in esophageal cancer: A SEER database analysis. J Thorac Oncol 2012;7(2):443-447. [http://dx.doi.org/10.1097/JTO.0b013e3182397751] [ Links ]
3. Berry MF. Esophageal cancer: Staging system and guidelines for staging and treatment. J Thorac Dis 2014;6(Suppl 3):S289-S297. [ Links ]
4. Knyrim K, Wagner HJ, Bethge N, Keymling M. A controlled trial of an expansile metal stent for palliation of esophageal obstruction due to inoperable cancer. N Engl J Med 1993;329(18):1302-1307. [ Links ]
5. Sarper A, Oz N, Cihangir C, Demircan A, Isin E. The efficacy of self-expanding metal stents for palliation of malignant esophageal strictures and fistulas. Eur J Cardiothorac Surg 2003;23(5):794-798. [http://dx.doi.org/10.1016/S1010-7940(03)00091-5] [ Links ]
6. White RE, Mungatana C, Topazian M. Esophageal stent placement without fluoroscopy. GI Endoscopy 2001;53(3):348-351. [http://dx.doi.org/10.1016/S0016-5107(01)70415-4, http://dx.doi.org/10.1067/mge.2001.112844] [ Links ]
7. Wilkes EA, Jackson LM, Cole AT, Freeman JG, Goddard AF. Insertion of expandable metallic stents in esophageal cancer without fluoroscopy is safe and effective: A 5-year experience. GI Endoscopy 2007;65(6):923-929. [http://dx.doi.org/10.1016/j.gie.2006.11.007] [ Links ]
8. Rathore OI, Coss A, Patchett SE, Mulcahy HE. Direct-vision stenting: The way forward for malignant oesophageal obstruction Endoscopy 2006;38(4):382-384. [http://dx.doi.org/10.1055/s-2005-921040] [ Links ]
9. Lazaraki G, Katsinelos P, Nakos A, et al. Malignant esophageal dysphagia palliation using insertion of a covered Ultraflex stent without fluoroscopy: A prospective observational study. Surg Endosc 2011;25(2):628-635. [http://dx.doi.org/10.1007/s00464-010-1236-2] [ Links ]
10. Dobrucali A, Caglar E. Palliation of malignant esophageal obstruction and fistulas with SEMS. World J Gastroenterol 2010;16(45):5739-5745. [http://dx.doi.org/10.3748/wjg.v16.i45.5739] [ Links ]
11. Christie NA, Buenaventura PO, Fernando HC, et al. Results of expandable metal stents for malignant esophageal obstruction in 100 patients: Short-term and long-term follow-up. Ann Thorac Surg 2001;71(6):1797-1801. [http://dx.doi.org/10.1016/S0003-4975(01)02619-4] [ Links ]
12. Cwikiel W, Tranberg KG, Cwikiel M, Lillo-Gil R. Malignant dysphagia: Palliation with oesophageal stents. Radiology 1998;207(2):513-518. [http://dx.doi.org/10.1148/radiology.207.2.9577503] [ Links ]
13. Ben Soussan E, Antonietti M, Lecleire S, et al. Palliative esophageal stent placement using endoscopic guidance without fluoroscopy. Gastroenterol Clin Biol 2005;29(8-9):785-788. [http://dx.doi.org/10.1016/S0399-8320(05)86348-1] [ Links ]
14. White RE, Mungatana C. Esophageal stent placement without fluoroscopy. Gastrointest Endosc 2001;53(3):348-351. [http://dx.doi.org/10.1067/mge.2001.117153] [ Links ]
Accepted 13 July 2015.
Corresponding author: D L Clarke (damianclar@gmail.com)














