Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.105 no.8 Pretoria ago. 2015
http://dx.doi.org/10.7196/SAMJNEW.8097
CONTINUING MEDICAL EDUCATION
ARTICLE
K BatemanI; C RogersII; E MeyerIII
IMB ChB, FCP Neurol (SA).Division of Neurology, Department of Medicine, Faculty of Health Sciences, Groote Schuur Hospital and University of Cape Town, South Africa
IIMSc (Audiology). Division of Communication Sciences and Disorders (Audiology), Department of Health and Rehabilitation Sciences, Faculty of Health Sciences, Groote Schuur Hospital and University of Cape Town, South Africa
IIIMB ChB, FCS (ORL). Division of Otolaryngology, Department of Surgery, Faculty of Health Sciences, Groote Schuur Hospital and University of Cape Town, South Africa
ABSTRACT
There can be few physicians so dedicated to their art that they do not experience a slight decline in spirits when they learn that their patient's complaint is giddiness. This frequently means that after exhaustive enquiry it will still not be entirely clear what it is that the patient feels wrong and even less so why he feels it. (W B Mathews)[1]
Contrary to this prevalent view, in recent years advances in the diagnosis and management of common vestibular disorders have made the clinical evaluation of the dizzy patient more rewarding. An accurate diagnosis may be possible in the majority of patients presenting with acute vertigo when a directed history is taken and an examination is performed. Specific and effective treatments are available for many patients. This article describes the clinical evaluation of a patient with acute vertigo, and highlights selected common and important conditions.
Vertigo, the illusion of movement, is usually due to peripheral vestibular disease of the end-organ or nerve. Acute vertigo or dizziness in isolation is usually benign. Despite recent consensus definitions of potential vestibular symptoms, such as vertigo, dysequilibrium and presyncope, it can be difficult to tease out a clear history of vertigo in a patient presenting with dizziness.[1] However, it is important to make a specific diagnosis to appropriately manage serious underlying conditions such as stroke and common conditions such as benign paroxysmal positional vertigo (BPPV), which respond well to immediate treatment. It is possible to make an accurate diagnosis in most patients and the history is the main tool. The clinical evaluation must answer the following questions: Firstly, is it vertigo? Secondly, is the lesion central (i.e. involving the parts of the central nervous system concerned with balance and vision) or peripheral (involving the vestibular nerve or apparatus of the inner ear)? Thirdly, does the patient require urgent brain imaging? We discuss the clinical approach to a patient with acute vertigo, and thereafter highlight selected common or important causes of vertigo, outlining management strategies.
Clinical approach to a patient with acute vertigo
Is it vertigo?
Vertigo has been defined as the sensation of motion when no motion is occurring.[2] The conventional diagnostic approach to vertigo or dizziness focuses on the nature of the symptom, whether vertigo, presyncope (impending faint), dysequilibrium (unsteadiness with eyes open), or nonspecific dizziness, to direct efforts towards investigating for vestibular (if vertigo), cardiac (if presyncope), neurological (if dysequilibrium), psychiatric or metabolic causes. However, 'dizziness' or 'vertigo' are used by patients for a range of subjective experiences that may not imply vertigo. Therefore, it is important to ask the patient to describe in detail the different sensations they experience, without asking leading questions. Is it rotatory/spinning (merry-go-round), rocking (as on a boat) or linear (like falling)? A rotational component to vertigo makes it highly likely that there is a disorder of the semicircular canals or their central pathways. It can be helpful to ask a patient if the problem is 'in their legs or in their head' (spinal cord/cerebellar v. vestibular causes) or if they feel 'as if they are about to faint' (presyncope).[3]
Recent studies, however, have shown that the timing (especially duration) and triggers of symptoms of dizziness may be more helpful in diagnosing the underlying disorder than the quality of the symptoms.[4] Determining whether vertigo is episodic or persisting, or provoked by positional changes, is very helpful for the diagnosis. Paroxysmal positional vertigo may be due to BPPV or, rarely, central positional causes. Recurrent spontaneous attacks of vertigo over several years are often due to migrainous vertigo or Meniere's disease. Acute persisting vertigo may be caused by vestibular neuritis or posterior fossa stroke. Very frequent short-lived spells of dizziness or imbalance might be due to vestibular paroxysmia or superior canal dehiscence syndrome. Postural imbalance without other neurological symptoms may, for example, commonly be secondary to chronic subjective dizziness or bilateral vestibulopathy following gentamicin toxicity.[5] More details of the timing of symptoms, possible triggers, associated features, and a broader differential diagnosis of acute vertigo are set out in Fig. 1. A complete medical history is essential, as many medications used to treat seizures, depression, anxiety and pain may affect the vestibular system.
Is the lesion central or peripheral?
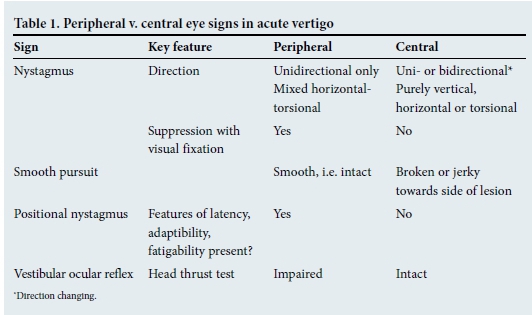
Once a history of the timing and triggers has narrowed down the differential diagnosis, careful examination should focus on dividing central from peripheral causes. Unidirectional nystagmus, where the direction of nystagmus is unchanged by change in direction of gaze (slow phase towards the dysfunctional labyrinth), is typical of peripheral vestibular disease, and will be most evident when looking in the direction of the fast phase. Unidirectional nystagmus may infrequently be seen in central vestibular lesions involving the brainstem; however, accompanying neurological signs make localisation fairly straightforward. The ability to suppress nystagmus in the light (i.e. with visual fixation) suggests intact central mechanisms.[3] The vestibular ocular reflex is impaired in peripheral vestibular disorders, and thus the head impulse (or head thrust) test will be abnormal. This test is fairly easy to perform, and is particularly useful to confirm peripheral dysfunction.[6]Smooth pursuit movements of the eyes are intact in peripheral vestibular syndromes, although the assessment may be difficult owing to the presence of marked nystagmus. With central causes of vertigo, pursuit movements of the eyes are typically broken or jerky. Positional nystagmus (triggered by rapid changes to the head position) is commonly seen and may be due to either peripheral (BPPV) or central causes. However, when caused by BPPV, it has characteristic features of latency, adaptibility, and fatigability (discussed below) that are not present in central disease. The Dix-Hallpike test should be performed on all dizzy patients, whether symptomatic or not. Table 1 summarises the key eye features of peripheral v. central vertigo.
A neurological examination should be performed, looking carefully for brainstem and cerebellar signs. Posterior fossa strokes may rarely cause isolated (central) vertigo, and infarction of the labyrinth may even more rarely mimic a peripheral vestibular disorder with vertigo and deafness (discussed below). Cardiac and aural examinations (usually including an audiogram) are necessary in this setting.
Does the patient require brain imaging?
Brain imaging is required in cases of acute vertigo, with one or more of the following:[3]
• new-onset (especially occipital) headache
• any central neurological symptoms or signs (including central nystagmus)
• acute hearing loss
• an intact head impulse test.
Common causes of acute vertigo
• Benign paroxysmal positional vertigo
BPPV is the most common cause of acute vertigo and has a characteristic history and examination. It is, however, frequently missed, because the patient does not spontaneously describe the position-induced nature of the vertigo or the attending doctor fails to perform a Dix-Hallpike test.
Patients typically have brief attacks of rotatory vertigo that are triggered by movements such as lying down or rolling over in bed, extending the neck, e.g. when inserting eye drops or reaching for an item on a shelf, or when flexing and extending the neck on bending over to lift and hang washing. Each episode lasts only seconds; however, it is not unusual for patients to complain of persisting symptoms of disturbed gait, blurred vision or 'wooziness', which may be misleading. Episodes of vertigo usually occur in clusters over a few weeks to months and then remit - only to return weeks, months or years later.
Examination reveals rotatory-linear nystagmus provoked by rapid changes to head position during the diagnostic positioning test - the Dix-Hallpike manoeuvre (Fig. 2). The nystagmus has a short latency (2 - 15 seconds), builds to a maximum, lasts <40 seconds, and is fatigable (wears off after repeated tests). The Dix-Hallpike test should be performed routinely in all patients who complain of dizziness (up to one-third of patients with BPPV may not give a typical history). In nearly all patients there are no other demonstrable clinical signs of auditory or vestibular dysfunction.
The cause of BPPV is mechanical, owing to the movement of loose otoconial particles within one semicircular canal, most often the posterior one. Particle positioning manoeuvres are therefore the mainstay of diagnosis (Dix-Hallpike test) and treatment (Epley or Semont manoeuvres). Video tutorials of these procedures are readily found on the internet, and the manoeuvres are very successful, safe and easy to administer.[7,8] One treatment with the Epley or Semont manoeuvre is often sufficient, as complete recovery is reported in 50 - 70% of patients.[9] Patients should be informed that the procedure is a treatment and not a cure, and that relapse is common, occurring in up to one-third of patients over the next 5 years. Education lessens patient anxiety and subsequent episodes can be retreated successfully.
• Vestibular neuritis
Vestibular neuritis presents with a subacute onset over hours of incapacitating vertigo, nausea and vomiting because of unilateral loss of vestibular function. Thought to be caused by the herpes simplex virus, it has been variably called 'vestibular neuronitis/neuritis' or 'labyrinthitis'. However, as evidence for viral infection is limited, some prefer the term 'acute idiopathic unilateral peripheral vestibulopathy'.[6] Unlike BPPV, spinning vertigo persists for hours to days. The sense of movement is present even with the eyes closed and is worsened by head movement; yet, it is not fully suppressed by keeping the head motionless.
On examination, typical unidirectional nystagmus is seen, as described above. The head impulse test is invariably abnormal. With the eyes open, the patient is unsteady but can stand without support.[6] Importantly, hearing is normal and no other neurological signs are present.
Management consists of supportive treatment (intravenous fluids, anti-emetics) and a vestibular suppressant, such as prochlorperazine or diazepam (preferably not for longer than a few days). The patient should be encouraged to mobilise as soon as possible to improve clinical recovery, which is largely achieved via central compensation.[10] Steroids appear to hasten complete recovery of the caloric function on testing, but no clinical or long-term benefits have been shown to justify their use in this setting.[11] Antiviral agents have not been proven to work.[12]
In most patients the symptoms resolve over weeks, but a feeling of dysequilibrium and dizziness with sudden head movement may last for months. Patients who have residual symptoms at 6 weeks may benefit from vestibular rehabilitation therapy. Although vestibular neuritis tends not to recur, it may be followed by BPPV (in 5%), which may prove more difficult to treat than usual.[13,14] If hearing loss is present, the likely diagnosis is labyrinthitis, and patients should be referred for specialist ear, nose and throat evaluation.
• Cerebellar stroke
In a patient with a first-ever attack of acute spontaneous vertigo persisting for several hours, the main differential diagnosis of acute vestibular neuronitis is cerebellar infarction. There are several clues to the diagnosis. First, the onset is hyperacute in stroke, whereas vestibular neuronitis usually develops over hours (rarely minutes). Second, if the head impulse test is positive, the patient has vestibular neuritis; if it is negative, the patient may have a cerebellar infarct. Third, vertigo ascribed to a cerebellar infarction may reveal nystagmus that is bilateral (i.e. direction changing), or vertical, or does not suppress well on fixation, suggesting a central cause. Patients have a sense of self-movement, even when their eyes are closed, and while this may worsen with head movement, it is not fully suppressed by keeping the head completely still. Last, a patient with cerebellar infarction often cannot stand without support, whereas one with acute vestibular neuronitis usually can. Cerebellar infarction is important to diagnose, as life-threatening posterior fossa brain swelling may ensue, needing emergency surgical decompression.
Recurrent short-lived vertiginous episodes are rarely caused by vertebrobasilar ischaemia, and if they occur almost always have additional brainstem symptoms or signs. Acute peripheral vertigo with a positive head impulse test and deafness may even more rarely be caused by vertebrobasilar ischaemia (specifically, infarction of the labyrinth); these patients require brain imaging if they lack a typical history of Meniere's disease.
• Vestibular migraine
Migrainous vertigo is an increasingly recognised cause of vertigo. As in the case of classic migraine, it is a clinical diagnosis according to consensus definitions.[15] Patients may be dizzy for minutes, hours or even days, with a range in their symptoms from mild dysequilibrium or motion intolerance to severe spinning sensations. When the vertigo occurs concurrent with a migraine, the diagnosis is fairly straightforward. However, migraineurs may quite often have episodes of vertigo, with or without other features of migraine such as photo-or phonophobia, in the absence of headache. Adding complexity to the diagnosis, some patients may have symptoms or signs - including nystagmus - that suggest central dysfunction. Consequently, brain imaging may be necessary in patients with a first presentation of acute migrainous vertigo. Standard antimigraine prophylactic drugs (e.g. sodium valproate, propranolol and amitriptyline) are used with good success, although robust evidence for the specific treatment of migrainous vertigo is lacking.[16]
• Ménière's disease
Patients with repeated attacks of spontaneous vertigo, each lasting >1 hour, are likely to have either vestibular migraine or Meniere's disease, but the latter is probably overdiagnosed with this presentation. A sense of pressure or fullness in the ipsilateral ear usually precedes the onset of vertigo by a few minutes. Vertigo lasts 20 minutes to a few hours (<24), and may or may not be accompanied by low-frequency ipsilateral tinnitus and fluctuating hearing loss that may persist for several days. Fatigue is common after the episodes. Attacks occur intermittently over years, and after the first few attacks vestibular and auditory function return to normal. Some patients remit spontaneously. However, in those who have ongoing attacks of vertigo, permanent loss of function may initially only be detected by audiogram or caloric testing. Over time, this may become clinically evident, with the added misery of tinnitus and hearing loss with unpleasant sound distortion persisting between attacks.
The diagnosis of Ménière's disease rests primarily on a meticulous history. Audiograms are useful, particularly when serial tests are performed, to document the low frequency and fluctuating hearing loss over time. Video nystagmography-caloric testing can confirm unilateral loss of vestibular function (usually incomplete), but this is nonspecific. Imaging is generally not helpful. However, when the history of vertigo is not typical, then unilateral tinnitus and moderate to severe hearing loss require magnetic resonance imaging of the internal auditory meatus to exclude a vestibular schwannoma.[2] Bilateral hearing loss should prompt referral to a specialist.
There are no proven treatments to prevent the progressive inner-ear damage that is presumed to be due to episodic endolymphatic hypertension. Symptomatic relief may be obtained with the use of vestibular suppressants, which may be administered rectally when nausea is severe. Betahistine (16 mg 3 times daily) or a low-salt diet, either alone or with a diuretic, is frequently used as prophylaxis, but remains unproven.[17] Betahistine given in higher doses (48 mg 3 times daily) may be more effective.[18,19] When intense attacks are frequent, more invasive procedures such as instillation of gentamicin or steroids via intratympanic injection or a grommet may be considered or, very rarely, vestibular nerve section or labyrinthectomy. Surgery on the endolymphatic sac is of questionable value.[20] However, all of these procedures treat symptoms of vertigo without preserving hearing or vestibular function.
Conclusion
When faced with a patient with vertigo, focus on the timing and triggers of symptoms, particularly if episodic, persisting or provoked by positional head changes. It is important to discriminate between central and peripheral causes by a careful, directed examination, including a Dix-Hallpike test which, if positive (signifying BPPV), may result in specific treatment with the Epley manoeuvre. An audiogram is particularly useful in a patient with vertigo; if normal in the setting of episodic vertigo, one might consider migraine rather than Meniere's disease. In the first-ever attack of acute spontaneous vertigo, a normal head impulse test raises concern of a cerebellar infarct. Although specific management of vertigo depends on the aetiology, all patients with vertigo benefit from vestibular rehabilitation exercises where the emphasis is on movement. Vestibular suppressants should be avoided in the long term as they may impede recovery.
References
1. Halmagyi G, Cremer P. Assessment and treatment of dizziness. J Neurol Neurosurg Psychiatry 2000;68(2):129-134. [ Links ]
2. Lempert T. Recurrent spontaneous attacks of dizziness. Continuum (Minneap Minn) 2012;18(5):1086-1101. [http://dx.doi.org/10.1212/01.CON.0000421620.10783.ac] [ Links ]
3. Seemungal BM, Bronstein AM. A practical approach to acute vertigo. Pract Neurol 2008;8:211-221. [http://dx.doi.org/10.1136/jnnp.2008.154799] [ Links ]
4. Newman-Toker DE. Symptoms and signs of neuro-otologic disorders. Continuum (Minneap Minn) 2012;18(5):1016-1040. [http://dx.doi.org/10.1212/01.CON.0000421618.33654.8a] [ Links ]
5. Brandt T, Strupp M, Dieterich M. Five keys for diagnosing most vertigo, dizziness, and imbalance syndromes: An expert opinion. J Neurol 2014;261(1):229-231. [http://dx.doi.org/10.1007/s00415-013-7190-x] [ Links ]
6. Halmagyi GM. Diagnosis and management of vertigo. Clin Med 2005;5(2):159-165. [ Links ]
7. Hilton M, Pinder D. The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database Syst Rev 2004;(2):CD003162. [ Links ]
8. Hilton M, Pinder D. The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database Syst Rev 2014;(12):CD003162. [ Links ]
9. Brandt T. How to do it: Exercise away vertigo. Pract Neurol 2001;1(1):36-41. [ Links ]
10. Goudakos JK, Markou KD, Psillas G, Vital V, Tsaligopoulos M. Corticosteroids and vestibular exercises in vestibular neuritis. Single-blind randomized clinical trial. JAMA Otolaryngol Head Neck Surg 2014;140(5):434-340. [ Links ]
11. Fishman JM, Burgess C, Waddell A. Corticosteroids for the treatment of idiopathic acute vestibular dysfunction (vestibular neuritis). Cochrane Database Syst Rev 2011;(5):CD008607. [ Links ]
12. Strupp M, Zingler VC, Arbusow V, et al. Methylprednisolone, valacyclovir, or the combination for vestibular neuritis. N Engl J Med 2004;351(4):354-361. [ Links ]
13. Huppert D, Strupp M, Theil D, Glaser M, Brandt T. Low recurrence rate of vestibular neuritis: A long- term follow-up. Neurology 2006;67(10):1870-1871. [ Links ]
14. Balatsouras DG, Koukoutsis G, Ganelis P, et al. Benign paroxysmal positional vertigo secondary to vestibular neuritis. Eur Arch Otorhinolaryngol 2014;271(5):919-924. [http://dx.doi.org/10.1007/s00405-013-2484-2] [ Links ]
15. Lempert T, Olesen J, Furman J, et al. Vestibular migraine: Diagnostic criteria. J Vestib Res 2012;22(4):167-172. [http://dx.doi.org/10.3233/VES-2012-0453] [ Links ]
16. Obermann M, Strupp M. Current treatment options in vestibular migraine. Front Neurol 2014;5:1-5. [http://dx.doi.org/10.3389/fneur.2014.00257] [ Links ]
17. Gordon A. Meniere's disease. Lancet 2006;367:984. [ Links ]
18. James AL, Burton MJ. Betahistine for Meniere's disease or syndrome. Cochrane Database Syst Rev 2001;(1):CD001873. [ Links ]
19. Strupp M, Krause E, Lezius F, Canis M, Ihler F, Gürkov R. Betahistine for Meniere's disease. Audiological Medicine 2012;10(4):167-170. [ Links ]
20. Thomsen J, Kerr A, Bretlau P, Olsson J, Tos M. Endolymphatic sac surgery: Why we do not do it. The non-specific effect of sac surgery. Clin Otolaryngol Allied Sci 1996;21(3):208-211. [ Links ]
Corresponding author: K Bateman (kathleen.bateman@uct.ac.za)














