Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.105 n.8 Pretoria Aug. 2015
http://dx.doi.org/10.7196/SAMJNEW.8039
CONTINUING MEDICAL EDUCATION
ARTICLE
E B Lee-PanI; L TuckerII
IMB ChB, MMed (Neurology). Division of Neurology, Department of Medicine, Faculty of Health Sciences, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
IIMB ChB, MSc, FCP (Neurology) (SA), PhD. Division of Neurology, Department of Medicine, Faculty of Health Sciences, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
ABSTRACT
The key to understanding and managing epilepsy is to decide whether seizures are genetic/idiopathic or caused by focal brain pathology. The classification of seizures was modified in 2010 after many variations of the original 1981 system and inconclusive debate. Major changes included abandoning many entrenched words and complete rejection of the Focal subsystem. While most of the reasoning is rational, the focal system is described in a long list of terms; general clinicians are therefore faced with a more challenging task than that required for understanding the old classification system. Some of the difficulties include using common words with non-intuitive neurological definitions, ambiguous words and the tendency to merge seizure categorisation with epilepsy. This article highlights some of the fundamental principles in trying to categorise seizures and offers a simplified way of using descriptive words to structure the organisation of Focal seizures. Focal seizures are broken down to A, B and C - an easy-to-remember schema for general clinicians, patients and carers. Words such as Aura' and 'Blank stare' are strategically used to represent old seizure types and how they may be linked in the same patient. Awareness or the lack thereof is explained and how the same patient may have different seizure types and combinations of these. There is less change in the Generalised seizures category, but these are often confused with Focal seizures. Absences are confused with blank stares, while Generalised Tonic-Clonic seizures (GTCSs) are confused with 'Focal-onset evolving rapidly to GTCSs'. Diagrams to illustrate the concepts of Generalised and Focal are included, as well as tables to demonstrate the differences between seizures that appear similar and points to consider in separating them. Focal seizures may mimic almost any human behaviour. Sorting and grouping the symptoms of Focal seizures with awareness (auras) is covered, along with sorting both the former and those without awareness seizures (As and Bs) by brain lobes. Distinguishing between Generalised and Focal seizures is not merely an academic exercise. It assists in determining the aetiology and has a material impact on the choice of management. Appropriate management of seizures starts with identifying the various seizure types. Time will tell whether or not this new descriptive approach to organisation of seizures makes the task easier and more effective.
A new organisation of epileptic seizures
(Note: because of the difficulty of using neurologically defined English words, these have been capitalised, e.g. Absence' is a neurologically defined word, whereas 'absence' is a normal English word. Where old terms are being replaced with new ones, both may be used together for clarity. Older discouraged terms are in square brackets. While descriptive words may change, the correct concepts need to be communicated accurately.)
The key to understanding and managing epilepsy is to decide whether the seizures are genetic [idiopathic] or caused by focal brain pathology. Unfortunately, the clinical description (semiology) of a seizure often fails to inform the clinician of this distinction and may be misleading. For example, a 60-year-old man presenting for the first time with a sudden Generalised Tonic-Clonic Seizure (GTCS), should be viewed as suffering from a possible Focal-onset seizure with secondary generalisation rather than a genetically predisposed Generalised seizure type, and an underlying structural intracranial lesion should be excluded.
How best to distinguish and classify different seizure types has challenged the world's top epileptologists for decades and, after many years of heated debate and unsatisfactory variations, the most recent classification, as well as many well-used terms, was finally abandoned in 2010, leaving a partial vacuum. The new organisation of seizures suggests that Focal seizures be described rather than pigeonholed.
Generalised seizures
Ambiguities with regard to terminology and confusion concerning neurological definitions of commonly used terms were largely responsible for the abovementioned decision. Conceptually, for instance, the word 'Generalised', e.g. a Generalised seizure, implies a disorder in which the entire cortex instantly becomes epileptiform (Fig. 1). Thus, a patient may be functioning entirely normally and, within a fraction of a second, epileptic activity may cause abrupt mass dysfunction of numerous neuronal systems throughout the brain, including memory and awareness. This virtually instantaneous shutdown of memory means that the patient will have no recall of anything that is 'happening or about to happen, i.e. no recollection of the seizure onset (i.e. no aura) and amnesia for the duration of the seizure. The two most common types of Generalised seizures are Absence seizures and GTCSs. These are both descriptive rather than aetiological terms, and have previously been termed 'idiopathic'. As used in epilepsy, idiopathic does not simply mean an 'unknown' aetiology, but implies 'in and of itself' (i.e. presumed genetic). Apart from abandoning the term idiopathic, there have been few significant recent changes in Generalised seizure categorisation.

Focal seizures
Compared with Generalised seizures, Focal seizures (the term 'Partial' has been formally abandoned) mostly occur after previous focal brain injury (e.g. meningitis as a baby or a significant head injury) or occasionally with an active lesion (e.g. tumour, parasite or abscess).
With retained awareness
Categorising Focal seizures has always been problematic, and one must keep in mind that individual patients may suffer from more than one Focal seizure type. When a Focal seizure starts, only that discrete region of the cortex is involved and rendered dysfunctional. For instance, if only a portion of the primary motor cortex is affected by epileptic activity, the patient may experience clonic jerking confined to the contralateral arm, while memory and awareness remain intact. Thus, the patient is able to experience and recall the manifestations of the focal seizure. This subjective recall of focal seizure activity may be regarded as an aura or warning of imminent extension to loss of awareness and/ or secondarily GTCSs.
With altered awareness
The focal epileptic activity described above may either remain confined or spread 'deeper' into the brain, rendering the patient 'unaware. When regions of the brain that mediate awareness are affected, but the seizure has no generalised tonic-clonic manifestations, it was previously termed a 'Focal Complex Seizure' or a 'Complex Partial Seizure, Complex indicating altered awareness or consciousness. The semiology of Focal Complex seizures may include a 'blank stare', a 'motor arrest' (sudden freezing), stereotyped non- or semi-purposeful movements, 'fidgeting' and 'lip-smacking'. These are often termed automatisms and usually take the form of simple, repetitive actions as described, but may occasionally be more complex, such as repetitive recitation of a phrase or walking in circles (post-ictal confusion is common after these seizures and may also be responsible for some behavioural components).
Evolving to GTCSs [secondarily GTCSs]
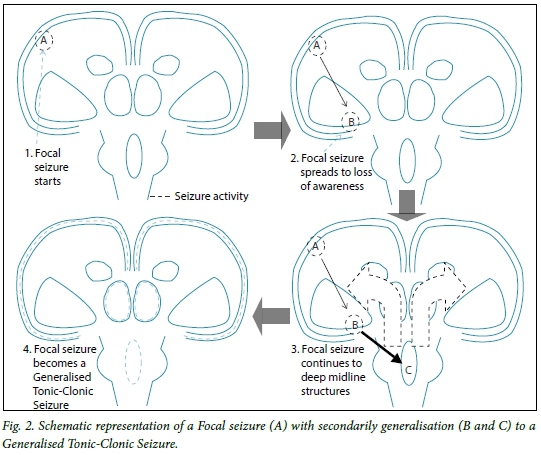
Ultimately, if the seizure spreads deep into the reticulothalamic circuits and then projects upwards to affect the entire brain, the patient will experience secondarily generalised tonic-clonic activity (Fig. 2). However, if the epileptic focus is situated in a clinically 'silent' area of the cortex, or if the spread from focus to generalisation is rapid, the patient may not experience or recall an aura. This means that it may be extremely difficult to distinguish Generalised seizures from Focal-onset seizures with rapid secondarily generalisation, as in the example at the beginning of the article. Post-ictal confusion is common after GTCSs and some patients may be transiently confused or psychotic.
Distinguishing between Generalised and Focal seizures is not merely an academic exercise. It assists in determining the aetiology and impacts materially on the choice of management.
Simplifying Focal seizures
The new descriptive categorisation of Focal seizures may sound simple and rational, but the current lack of clearly defined unambiguous terms and absence of an acceptable classification structure are problematic and make teaching difficult for healthcare professionals. Furthermore, patients and their carers need to categorise seizures to diarise them correctly. Understandably, most general clinicians are reluctant to invest the time necessary to adopt new complex classifications, as they deal with seizures infrequently. As a compromise, we use the descriptive words aura and blank stare instead of Focal Simple and Focal Complex seizures, respectively. By abbreviating this further to A (aura) and B (blank stare) and adding C (for secondarily GTCS), a clinically useful A->B->C mnemonic is available for patients and medical staff (Table 1). This also satisfies the current recommendation of describing the semiology.

For Generalised seizures, a similar A and C mnemonic represents A for Absence and C for GTCS, with a gap in between for all the other, much less common, Generalised seizure subtypes. Of these, 'myoclonic' is probably the next most common subtype. Some Generalised seizure subtypes are seen mostly in children, e.g. an atonic seizure.
Separating the description of a seizure from its cause is intuitively difficult. For instance, although the concept of Generalised seizures is strongly linked to a presumed genetic [idiopathic] aetiology, Generalised seizures may also occur owing to underlying non-genetic metabolic disorders. Similarly, certain focal-onset seizures subtypes are presumed to have a genetic basis. Consequently, this review is necessarily simplistic and covers the more commonly encountered and more easily separated seizure types.
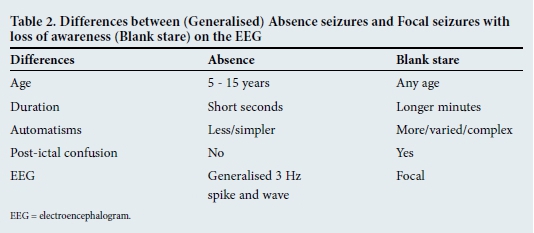
Pragmatically, it may be useful to tabulate some differences between clinically similar, yet physiologically and aetiologically distinct, seizure types. For instance, Generalised Absence seizures are often confused with Focal [Complex] blank stare seizures as both involve altered awareness. However, Absences only very rarely occur in adults, especially for the first time, while onset of Focal [Complex] blank stare seizures may occur at any age (Table 2). The two kinds of GTCSs are compared in Table 3.

To complicate matters, as is the case with Focal seizures, some patients with [idiopathic] Generalised seizures may experience more than one seizure type; most commonly Absence seizures and GTCSs. However, these generalised seizure types occur independently - even at different times in a patient's life. Patients with juvenile myoclonic epilepsy may have three seizure types (myoclonic, Absence and GTCSs). These may occur independently, but some patients feel their myoclonus 'warns' them of an impending GTCS. This does not imply a focal onset, but indicates that the concept of instantaneous loss of awareness in Generalised seizure types is not always the case, as these patients are fully aware of their myoclonus.
The 'hallmark' of Focal complex/blank stare-type seizures is their consistent stereotypy, irrespective of whether the clinical manifestations of the seizure are subtle (e.g. fidgeting or lip-smacking) or dramatic (e.g. overt bizarre behaviour), their electrical and clinical evolutions are consistently locked - every detail happens in the same way and order every time.
Grouping Focal seizure symptoms
Focal seizures are of special interest to all clinicians, as they may closely mimic almost any non-epileptiform paroxysmal event. With this in mind, it is useful to group the Focal seizures with retained awareness and memory (i.e. auras) into four categories: motor, sensory, autonomic or psychic.
The motor category may seem simple to identify but may range from unilateral tonic and clonic elements to a wide range of more complex actions. Sensory symptoms also have a wide spectrum involving all sensory modalities, from primary sensations such as paraesthesia, pain and even rarely numbness, to the special senses such as smell, taste, vision and hearing. Autonomic seizure symptoms may also be quite varied, but most commonly involve gastrointestinal symptoms best described as 'a rising epigastric sensation'. These epigastric auras may remain confined to the abdominal area. Psychic symptoms are less common and often the most difficult to recognise as a seizure. Examples include an unexplained feeling of inappropriate intense fear or 'impending doom' or the more common déja vu. Whatever the seizure symptom, its episodicity, clinical context and stereotypy help to identify it as a seizure.
One may also group Focal seizures according to the lobe in which the seizure occurs, whether or not they involve loss of awareness (auras and blank stares). This is because the nature of the Focal seizure onset (i.e. the semiology of the aura) is often closely linked to the anatomical site of the seizure focus. Statistically, the majority of focal seizures have their onset in the temporal lobe. The next most common site is the frontal lobe, while the parietal and occipital lobes have a much lower propensity to cause Focal seizures. This regional propensity for Focal seizure onset is reflected electrophysiologically. A potentially epileptic spike (i.e. electrical discharge) identified in the temporal lobe on an electroencephalogram (EEG) is much more likely to be associated with seizures than an identical spike in the occipital lobe. Apart from being the most frequent type, temporal lobe auras may also involve a wide range of symptom types - from autonomic to psychic, but also sensory, such as olfactory, gustatory, visual illusions, hallucinations and even vertigo. Once awareness is impaired, temporal lobe seizures are also involved in the blank stare or motor freeze, oral automatisms (i.e. lip smacking) and aphasia. Electrical seizures do not recognise lobe boundaries; hence, there may be some overlap.
Frontal lobe seizures host a wide variety of complex motor actions as well as strange alterations of awareness and 'bizarre behaviour', often with little or no post-ictal confusion. It is not uncommon for patients with frontal lobe seizures to be referred for psychiatric assessment before the ictal nature of their symptoms is recognised. The recent discovery of an association between some strange seizures (e.g. brachiodystonic) and autoantibodies (e.g. against the NMDA (N-methyl-D-aspartate) or AMPA (α-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid) receptors is important, because this has resulted in the recognition of encephalitides, some of which are paraneoplastic, and most of which are treatable with immunosuppression if identified in the early stages. The seizures associated with these autoimmune encephalitides are generally immune to standard anti-epileptic drugs.
Appropriate management of seizures starts with identifying the various seizure types. Time will tell whether or not the new descriptive approach to organisation of seizures makes this task easier and more effective.
Corresponding author: E B Lee-Pan (eddy.leepan@uct.ac.za)














