Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.105 no.8 Pretoria ago. 2015
http://dx.doi.org/10.7196/SAMJNEW.8065
CONTINUING MEDICAL EDUCATION
REVIEW
An approach to the clinical assessment and management of syncope in adults
N A B NtusiI; C B I CocciaII; B J CupidoIII; A ChinIV
IFCP (SA), DPhil. Division of Cardiology, Department of Medicine, Faculty of Health Sciences, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
IIMB ChB. Division of Cardiology, Department of Medicine, Faculty of Health Sciences, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
IIIFCP (SA). Division of Cardiology, Department of Medicine, Faculty of Health Sciences, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
IVFCP (SA), MPhil. Division of Cardiology, Department of Medicine, Faculty of Health Sciences, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
ABSTRACT
Syncope, defined as a brief loss of consciousness due to an abrupt fall in cerebral perfusion, remains a frequent reason for medical presentation. The goals of the clinical assessment of a patient with syncope are twofold: (i) to identify the precise cause in order to implement a mechanism-specific and effective therapeutic strategy; and (ii) to quantify the risk to the patient, which depends on the underlying disease, rather than the mechanism of the syncope. Hence, a structured approach to the patient with syncope is required. History-taking remains the most important aspect of the clinical assessment. The classification of syncope is based on the underlying pathophysiological mechanism causing the event, and includes cardiac, orthostatic and reflex (neurally mediated) mechanisms. Reflex syncope can be categorised into vasovagal syncope (from emotional or orthostatic stress), situational syncope (due to specific situational stressors), carotid sinus syncope (from pressure on the carotid sinus, e.g. shaving or a tight collar), and atypical reflex syncope (episodes of syncope or reflex syncope that cannot be attributed to a specific trigger or syncope with an atypical presentation). Cardiovascular causes of syncope may be structural (mechanical) or electrical. Orthostatic hypotension is caused by an abnormal drop in systolic blood pressure upon standing, and is defined as a decrease of >20 mmHg in systolic blood pressure or a reflex tachycardia of >20 beats/minute within 3 minutes of standing. The main causes of orthostatic hypotension are autonomic nervous system failure and hypovolaemia. Patients with life-threatening causes of syncope should be managed urgently and appropriately. In patients with reflex or orthostatic syncope it is important to address any exacerbating medication and provide general measures to increase blood pressure, such as physical counter-pressure manoeuvres. Where heart disease is found to be the cause of the syncope, a specialist opinion is warranted and where possible the problem should be corrected. It is important to remember that in any patient presenting with syncope the main objectives of management are to prolong survival, limit physical injuries and prevent recurrences. This can only be done if a patient is appropriately assessed at presentation, investigated as clinically indicated, and subsequently referred to a cardiologist for appropriate management.
Syncope refers to a brief loss of consciousness (LOC) due to an abrupt fall in cerebral perfusion. It remains a frequent reason for medical presentation and accounts for a large proportion of emergency department and outpatient clinic visits. While there are no population-based epidemiological studies of syncope in South Africa, it accounts for up to 3% of hospital admissions in western countries. There are many causes of syncope (discussed below) - some benign and others more serious. The goals of the clinical assessment of a patient with syncope are twofold: (i) to identify the precise cause in order to implement a mechanism-specific and effective therapeutic strategy; and (ii) to quantify the risk of recurrence or death, which depends on the underlying disease rather than the mechanism of the syncope. Hence, a structured approach to the patient with syncope is required. History-taking is the most important aspect of the clinical assessment. The patient's history guides both appropriate selection of investigations and best management strategy.
Definition of syncope
Syncope is a transient loss of consciousness (T-LOC) caused by transient global hypoperfusion of both cerebral hemispheres or focal hypoperfusion of the reticular activating system. Cerebral hypoperfusion may be secondary to decreased cardiac output, peripheral vascular resistance or a combination of both. Four cardinal clinical features characterise the syncopal episode: (i) it is transient; (ii) it has a rapid onset; (iii) it has a short duration (lasting seconds to several minutes); and (iv) there is spontaneous complete recovery requiring no resuscitative efforts.[1] Appropriate orientation and behaviour is restored after the syncopal episode and there is complete return of pre-existing neurological function. Retrograde amnesia may occur in older adults. Syncopal patients may have brief, involuntary clonic movements, but do not report tongue biting or incontinence.
T-LOC encompasses all disorders characterised by self-limited LOC, irrespective of mechanism. Other causes of T-LOC include trauma, epileptic seizures and psychogenic LOC. Syncope is differentiated from other causes of T-LOC by its mechanism of global cerebral hypoperfusion.
Presyncope indicates symptoms and signs that occur before LOC in syncope. It is often used interchangeably with 'dizziness' and 'light-headedness' to describe a situation in which the individual thinks he or she may have a blackout, but consciousness is maintained.
Is the cause of the syncopal episode life threatening?
The primary responsibility of the emergency department doctor or general practitioner is to ensure that a life-threatening cause of syncope is excluded. The four main life-threatening causes of syncope are: (i) cardiac syncope (arrhythmia related or structural); (ii) massive haemorrhage with haemodynamic instability; (iii) pulmonary embolism; and (iv) subarachnoid haemorrhage (which should be suspected if a patient presents with syncope after a headache).
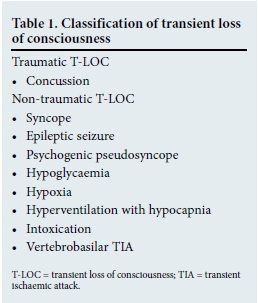
Classification of transient loss of consciousness
T-LOC is divided into traumatic and nontraumatic forms. T-LOC related to trauma is usually the result of concussion. Nontraumatic causes of T-LOC include syncope, epileptic seizures, intoxication, vertebrobasilar transient ischaemic attack (TIA) and metabolic disorders, such as hypoglycaemia, hypoxia and hyperventilation with hypocapnia (Table 1). Other disorders without LOC may also be incorrectly diagnosed as syncope; these include cataplexy, drop attacks, falls, psychogenic pseudosyncope and a TIA of vertebrobasilar origin.[1] Differentiating syncope from seizure and TIA is not always easy, and Table 2 provides useful pointers.

Classification of syncope
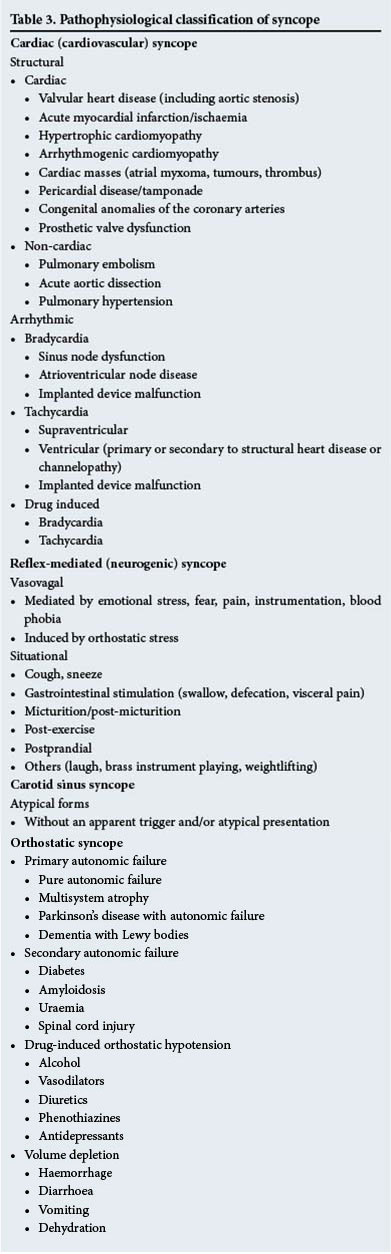
The classification of syncope is based on the underlying pathophysiological mechanism causing the event, emphasising collections of disparate disorders with a common presentation but different risk profiles (Fig. 1). Syncope is classified into cardiac syncope, orthostatic hypotension (OH) and reflex (neurally mediated) mechanisms.[2] Reflex syncope is the most frequent cause of syncope in any setting and is particularly common in young females. The most common cause of syncope is cardiac related. OH is rare in patients <40 years of age, whereas it is prevalent in older patients (Table 3). Of note, 5 - 15% of syncopal episodes are medication related (from orthostasis or cardiotoxicity).
Reflex syncope
Cardiovascular reflexes play an important role in maintaining blood pressure (BP) in normal individuals, but can cause a significant decrease in BP with subsequent syncope in those with an inappropriate response. The syncope may be due to a vasodepressor or cardio-inhibitory type of reflex - the former causing a loss of vasoconstriction and the latter resulting in significant bradycardia or asystole.[1] Reflex syncope can be further categorised into vasovagal syncope (from emotional or orthostatic stress); situational syncope (due to specific situational stressors such as micturition, vomiting and defecation); carotid sinus syncope (from pressure on the carotid sinus, e.g. shaving or a tight collar); and atypical reflex syncope (episodes of syncope or reflex syncope that cannot be attributed to a specific trigger or syncope with an atypical presentation).
Cardiac syncope
Cardiovascular causes of syncope may be structural (mechanical) or electrical.[3] Structural heart disease results in global cerebral hypoperfusion by decreasing the cardiac output and subsequently the systemic BP. Syncope occurs when the circulatory demands outweigh the ability of the heart to maintain an adequate cardiac output. In conditions with a fixed ventricular outflow obstruction it is not only the decreased cardiac output that plays a role, but also a reflex vasodilation or orthostatic hypotension. The main causes of structural syncope are highlighted in Table 3 and include acute myocardial infarction/ ischaemia, hypertrophic cardiomyopathy (HCM), arrhythmogenic cardiomyopathy, valvular heart disease (e.g. aortic stenosis and mitral stenosis) and pericardial disease. Arrhythmias causing syncope can be either brady- or tachyarrhythmias, and may be acquired or caused by congenital defects. Acquired bradyarrhythmias include sick sinus syndrome, which causes pauses due to sinus arrest and a subsequent fall in cardiac output. The atrioventricular (AV) blocks causing syncope include Mobitz I and II AV block, high-degree AV blocks (2:1 AV block and greater) and complete AV block - the mechanism being either ventricular asystole (i.e. an absent escape rhythm) or torsades des pointes due to prolongation of the QT interval. For many cardiovascular causes of syncope the pathogenesis is multifactorial, e.g. in HCM, where the syncope may be secondary to outflow obstruction, ventricular or atrial arrhythmias or neurally mediated mechanisms.
Orthostatic hypotension
OH is due to an abnormal drop in systolic BP upon standing, and is defined as a decrease of >20 mmHg in systolic BP or a reflex tachycardia of >20 beats/minute within 3 minutes of standing.[2] The main causes of OH are autonomic nervous system (ANS) failure and hypovolaemia. Other causes are illustrated in Table 3. In older patients, especially those with diabetes, mild autonomic neuropathy is common and may easily be aggravated by diuretic treatment, medication prescribed for hypertension or tricyclic antidepressants. Vasodilator therapy or diuretics that were recently added as treatment are common precipitants of new-onset OH and syncope in the elderly.
Prognosis of syncope
The prognosis of syncope relates to: (i) the risk of death and life-threatening events; and (ii) the risk of recurrence of the syncope and physical injury.[1,3] The prognosis depends on the underlying cause of the syncope. Higher mortality is associated with life-threatening cardiac causes of syncope. Furthermore, there is a high morbidity in patients with a risk of recurrence of syncope and subsequent physical injury.[4]
Structural heart disease and primary cardiovascular electrical disease are major risk factors for sudden cardiac death (SCD) in syncope. OH results in a twofold higher risk of mortality in syncope. Mortality is often related to the severity of the underlying disease rather than to syncope per se. However, young persons without structural or electrical heart disease have an excellent prognosis.[5] In up to one-third of adults there is recurrent syncope within 3 years of follow-up. Psychiatric disease and age <45 years predict higher rates of pseudosyncope. Major injury, including fractures and motor vehicle accidents, is reported in 6% of patients with syncope. Minor and soft-tissue injuries occur in 12% of patients. Morbidity is particularly high in the elderly. Moreover, recurrent syncope may have serious effects on the quality of life.[1]
Clinical evaluation of syncope
History and examination
As syncope is a symptom or clinical presentation of an underlying disorder, attempting to establish the cause is essential and relies heavily on the history and physical examination. On history, the diagnosis of syncope can be confirmed by asking four key questions:
• Was the LOC complete?
• Was the LOC transient, with rapid onset and short duration?
• Did the patient recover spontaneously and completely, without sequelae?
• Did the patient lose postural tone?
The answer to all these questions should be positive.
In the majority of patients the diagnosis of syncope may be confirmed based on the history alone. Obtaining a detailed history from a witness such as a partner or family member is important to describe the LOC. History-taking must be comprehensive and include details of the situation, precipitating factors, prodrome, LOC episode and postprodrome. Important aspects to glean from the history include whether the syncope is postural, exertional, situational and associated with palpitations or cardiovascular symptoms. Additionally, the clinician must take into account the use of medications, a family history of SCD, and a personal history of cardiac disease. Table 4 includes features on the history that may be useful to distinguish a cause. The history should always aim to answer three important questions:
• Was this a syncopal episode?
• If indeed syncope, what is the cause?
• Are there features suggesting high risk of cardiovascular events or death?[4]
On examination, the vital signs must be assessed, including pulse, BP, pallor and bruits, and OH must be checked. The BP needs to be measured in the supine position, followed by BP in the erect position after 3 minutes of standing. A cardiovascular examination includes evaluation of features of underlying cardiac disease, such as impaired systolic function arrhythmias and murmurs suggesting conditions such as mitral or aortic stenosis or HCM. Neurological examination focuses on ascertainment of muscle weakness, paraesthesia, cranial nerve abnormalities and peripheral neuropathy. Gastrointestinal tract (GIT) examination should exclude a GIT source of blood loss.[4]
Special investigations
An ECG is recommended in all patients who present with syncope, checking for evidence of abnormal rhythm, prolonged intervals (PR, QRS, and QTc), severe bradycardia, pre-excitation, myocardial infarction, low voltage in standard limb leads suggestive of effusion, and abnormal conduction. The ECG plays a crucial role in diagnosing arrhythmia, ischaemia, pulmonary embolism, and HCM (Table 5).

Additional assessments may be performed, but must be directed based on the findings of the initial evaluation. Importantly, <2 - 3% of patients evaluated for syncope have abnormal laboratory results.[1,6] Therefore, the routine use of a broad panel of laboratory tests is not recommended and tests should only be requested when clinically indicated. Further investigations (Table 6) are usually the domain of cardiologists, as the performance and interpretation thereof require specialised training.
Echocardiography is useful in the evaluation of left ventricular systolic function and delineation of structural heart disease, including abnormal valves, chamber enlargement, hypertrophy, wall motion and pericardial disease. However, in patients with an unremarkable clinical examination, normal ECG, and no cardiac history the value of echocardiography is minimal. Transoesophageal echocardiography, cardiovascular computed tomography or cardiovascular magnetic resonance imaging may be considered for evaluation of structural heart disease when the transthoracic echocardiogram is abnormal or the index of suspicion of myocardial, valvular, pericardial or coronary artery disease is high.[2]
Tilt-table testing may be useful when there is an intermediate probability of reflex syncope or to demonstrate OH in a controlled environment. In a patient with a typical history suggestive of reflex syncope a tilt-table test is not indicated, as a negative test does not exclude reflex syncope. The sensitivity and specificity of tilt-table testing are 65% and 93%, respectively. The patient is attached to a cardiac and BP monitor, lies flat for 10 minutes and is then tilted 60 - 70° head-up and observed for 30 minutes for symptoms and signs of syncope. At 15 minutes, a sublingual nitrate is administered if no symptoms have occurred. The test is considered positive if the patient's symptoms are reproduced in the presence of hypotension, bradycardia or both. Contraindications to performing tilt-table testing include a recent myocardial infarction, stroke or tight carotid stenosis.[7]
Carotid sinus massage (CSM) to diagnose carotid sinus hyper-sensitivity (CSH) is only recommended in patients >40 years of age with syncope or unexplained falls without a clearly identified cause. CSM is positive when it causes a pause of >3 seconds in the heartbeat (cardio-inhibition) or lowering of the BP by >50 mmHg (vasodepression). Complications that may arise from the procedure are TIAs or strokes (both rare). It is therefore recommended that CSM be avoided in patients with a previous TIA or stroke or in those with carotid bruits.
ECG monitoring (telemetry, Holter monitoring and implant-able loop recorders (ILRs)) is used to detect an underlying arrhythmia when initial cardiac or neural-ly mediated syncope investigations are negative and an arrhythmia is suspected. In-hospital telemetry and 24-hour Holter monitoring have a typical, very low yield but may be considered for frequent syncopal episodes. An ILR is a very useful diagnostic tool in patients with unexplained syncope; it has a battery life of 2 - 3 years. When syncope occurs, the device can be retrospectively activated by the patient and subsequently interrogated to establish whether there were any arrhythmias at the time of the syncopal episode. Documenting no arrhythmia during a syncopal episode is very useful to exclude an arrhythmic cause of syncope.
ILRs should be considered when there is recurrent unexplained or high-risk syncope, frequent episodes affecting quality of life, recurrent and unpredictable episodes putting the patient at risk of trauma, or when syncope occurs during high-risk activity, e.g. operating machinery or driving. Occasionally, electrophysiological studies may be indicated in patients with a high index of suspicion for ventricular tachycardia, bundle branch block, or supraventricular tachycardia.
Risk stratification
The prognosis varies among the different categories of syncope and in many cases the diagnosis remains uncertain from history and examination alone. Between 20% and 50% of patients have unexplained syncope after intensive diagnostic evaluation. Therefore, risk stratification tools have been designed to assist differentiation between low- and high-risk patients. These tools aid in deciding whether a patient qualifies for hospital admission and further investigation or if they can be reassured and discharged from an emergency unit. Ultimately, it is imperative that the final decision remains that of the attending practitioner, based on his/her clinical discretion.[1,6,7]Table 7 illustrates the findings that categorise patients according to risk.
Management principles
As syncope is a symptom of disease, management depends on the underlying cause.
Establishing the diagnosis should largely be based on a thorough history and examination and the use of basic investigations, e.g. an ECG. Further investigations should only be used when clinically indicated.
Discussion of specific treatment options in individual diseases is beyond the scope of this article. Patients with life-threatening causes of syncope should be managed urgently and appropriately. In patients with reflex or orthostatic syncope it is important to address any exacerbating medication and provide general measures to increase BP, such as physical counter-pressure manoeuvres. A small proportion of patients with severe cardio-inhibitory carotid sinus hypersensitivity may require a dual-chamber pacemaker. Where heart disease is found to be the cause of the syncope a specialist opinion is warranted and where possible the problem should be corrected.
Conclusion
It is important to remember that in any patient presenting with syncope the main objectives of management are to prolong survival, limit physical injuries and prevent recurrences. This can only be done if a patient is appropriately assessed at presentation, investigated as clinically indicated, and subsequently referred to a cardiologist for appropriate management. In patients in whom the diagnosis remains uncertain, risk stratification tools can be utilised to assist in deciding whether patients need admission or further evaluation.
Funding. This review is not funded. Dr N A B Ntusi acknowledges funding from the National Research Foundation and Medical Research Council of South Africa.
References
1. Task Force for the Diagnosis and Management of Syncope; European Society of Cardiology (ESC); European Heart Rhythm Association (EHRA); Heart Failure Association (HFA); Heart Rhythm Society (HRS); Moya A, Sutton R, Ammirati F, et al. Guidelines for the diagnosis and management of syncope (version 2009). Eur Heart J 2009;30(21):2631-2671. [http://dx.doi.org/10.1093/eurheartj/ehp298] [ Links ]
2. Brignole M, Hamdan MH. New concepts in the assessment of syncope. J Am Coll Cardiol 2012;59(18):158315-158391. [http://dx.doi.org/10.1016/j.jacc.2011.1L056] [ Links ]
3. Ungar A, del Rosso A, Giada F, et al.; Evaluation of Guidelines in Syncope Study 2 Group. Eur Heart J 2010;31(16):2021-2026. [http://dx.doi.org/10.1093/eurheartj/ehq017] [ Links ]
4. Parry SW, Tan MP. An approach to the evaluation and management of syncope in adults. BMJ 2010;340:c880. [http://dx.doi.org/0.1136/bmj.c880] [ Links ]
5. Ganzeboom KS, Colman N, Reitsma JB, Shen WK, Weiling W. Prevalence and triggers of syncope in medical students. Am J Cardiol 2003;91(8):1006-1008. [http://dx.doi.org/org/10.1016/S0002-9149(03)00127-9] [ Links ]
6. Gauer RL. Evaluation of syncope. Am Fam Physician 2011;84(6):640-650. [ Links ]
7. Seger JJ. Syncope evaulation and management. Tex Heart Inst J 2005;32(2):204-206. [ Links ]
Corresponding author: N A B Ntusi (ntobeko.ntusi@gmail.com)














