Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.105 no.8 Pretoria Ago. 2015
http://dx.doi.org/10.7196/SAMJNEW.7803
FORUM
HEALTHCARE DELIVERY
Patient support interventions to improve adherence to drug-resistant tuberculosis treatment: A counselling toolkit
E MohrI; J HughesII; L SnymanIII; B BekoIV; X HarmansV; J CaldwellVI; H DuvivierVII; L WilkinsonVIII; V CoxIX
IDrug-resistant tuberculosis (DR-TB) epidemiologist at Médecins Sans Frontières (MSF) Khayelitsha, Cape Town, South Africa, obtained a Master's in Public Health from Boston University (USA), concentrating in epidemiology. Her special interests include infectious diseases, maternal and child health and developing health care systems
IIDR-TB doctor at MSF Khayelitsha, graduated MB BCh and BSc Hons (Public Health) from Cardiff University in Wales and completed a Diploma in Tropical Medicine and Hygiene (DTMH) in Liverpool
IIIDR-TB patient support manager at MSF Khayelitsha, graduated with a Diploma in General Nursing and has completed a short course in palliative nursing care
IVA DR-TB counsellor at MSF Khayelitsha, is studying for a degree in social work. Her special interests include patient-centred models of care, particularly for patients with DR-TB
VIs also a DR-TB counsellor at MSF Khayelitsha. As a former extensively drug-resistant tuberculosis patient, she is interested in the provision of structured patient support for DR-TB
VIA registered nurse with a BCur degree, is TB project manager at the Department of Health for the City of Cape Town
VIIPatient and community support advisor at MSF South Africa and Lesotho, is a clinical sexotherapist with a master's degree in Sciences of Family and Sexuality from Louvain-la-Neuve University, Belgium
VIIIProject co-ordinator of the HIV/TB Programme at MSF Khayelitsha, is a qualified attorney with a master's degree in Global Health. Her special interests include HIV and TB retention and adherence strategies, focusing on community models of care and patient support-related interventions
IXMD, current deputy field co-ordinator of the HIV/TB Programme at MSF Khayelitsha, is particularly interested in infectious diseases and recently completed an MSF mission in Liberia to provide assistance with the Ebola outbreak
ABSTRACT
In response to the growing burden of drug-resistant tuberculosis (DR-TB) in South Africa (SA), Médecins Sans Frontières (MSF), with local government health departments, piloted a decentralised model of DR-TB care in Khayelitsha, Western Cape Province, in 2007. The model takes a patient-centred approach to DR-TB treatment that is integrated into existing TB and HIV primary care programmes. One essential component of the model is individual and family counselling to support adherence to and completion of treatment. The structured and standardised adherence support sessions have been compiled into a DR-TB counselling toolkit. This is a comprehensive guide that focuses on DR-TB treatment literacy, adherence strategies to encourage retention in care, and provision of support throughout the patient's long treatment journey. Along with other strategies to promote completion of treatment, implementation of a strong patient support component of DR-TB treatment is considered essential to reduce rates of loss from treatment among DR-TB patients. We describe our experience from the implementation of this counselling model in a high DR-TB burden setting in Khayelitsha, Cape Town, SA.
Drug-resistant tuberculosis (DR-TB), defined as TB with at least rifampicin resistance, is increasing in prevalence and incidence worldwide.[1] South Africa (SA) has reported some of the highest numbers of DR-TB cases globally: in 2012 alone there were 14 161 laboratory-notified cases of multidrug-resistant TB (MDR-TB) and 1 545 cases of extensively drug-resistant TB (XDR-TB).[2] Regimens available for DR-TB are expensive, toxic, and require a minimum treatment duration of 20 months. In addition, currently available medications often cause multiple side-effects that impact on patients' ability to maintain their usual daily activities.[3] The burden of treatment regimens contributes to poor DR-TB programme outcomes, including high rates of loss from treatment (LFT) and stagnant treatment success rates. A study conducted in the Western Cape Province, SA, found an LFT rate of 27%, which is comparable to LFT rates observed in other DR-TB treatment cohorts in SA.[4] National Department of Health (NDoH) data from 2012 reflect a 40% treatment success rate for MDR-TB and less than 20% treatment success for XDR-TB.'21 It is imperative that strategies to provide structured patient support are developed and implemented to promote retention in care.
Setting
Khayelitsha, a township in the Western Cape, is home to approximately 500 000 people and has one of the highest rates of HIV and TB among subdistricts in the country. It was determined that there were 989 cases of DR-TB diagnosed in Khayelitsha from 2003 through 2010, 200 of which were diagnosed in 2010. In response to the growing burden of DR-TB in Khayelitsha, Médecins Sans Frontières (MSF) collaborated with City of Cape Town Department of Health (CCTDoH) and provincial health services in 2007 to pilot a decentralised model of care in which primary healthcare clinicians initiate and manage treatment of patients diagnosed with DR-TB at Khayelitsha-based clinics. The prevailing model of care for DR-TB previously involved centralisation of treatment to 45 specialised hospitals in SA, which hindered the ability to provide longitudinal support to DR-TB patients and their families in their local community. In contrast, decentralisation to primary care enabled patient support to form a major component of the overall model of care.[5] Two dedicated lay DR-TB counsellors were employed to provide education and support to DR-TB patients managed at 11 primary care clinics in the subdistrict. Since 2011 the model has been managed by the CCTDoH, and various aspects of the model have been adopted and implemented across other subdistricts in the Western Cape. In 2012, MSF, together with the CCTDoH, developed a more structured, standardised, patient-centered approach to counselling DR-TB patients, placing equal emphasis on treatment literacy and adherence support.
Objective
A policy of decentralised management of DR-TB in SA was endorsed by the NDoH in 2011. Although welcomed for its prioritisation of decentralisation nationally, it lacks specific information on how to provide structured patient support and counselling despite its recommendation to provide these services to patients. The DR-TB counselling toolkit aims to provide guidance on how to provide patient support to promote adherence to difficult treatment regimens, to encourage retention in care, and to increase the likelihood of successful treatment outcomes.
The intervention
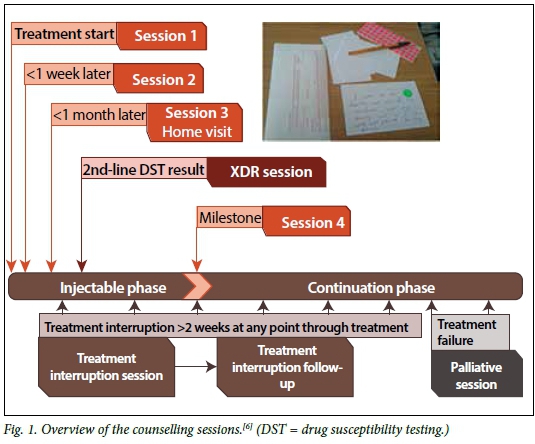
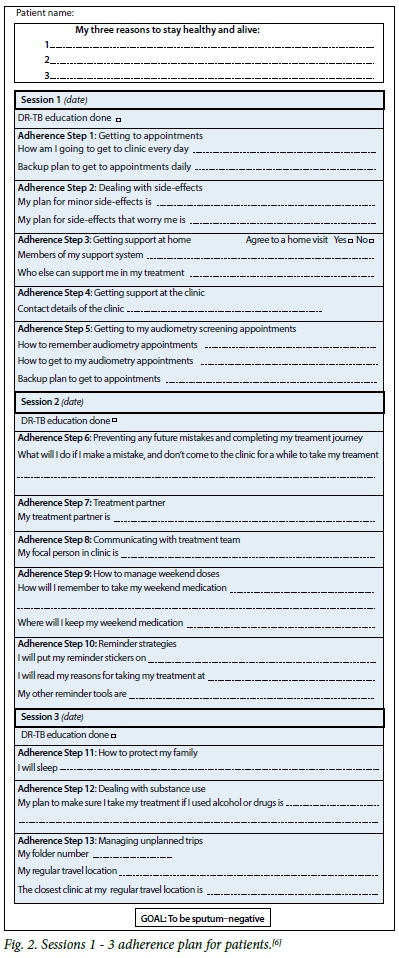
The counselling toolkit is a comprehensive guide that provides patients with support throughout the duration of their treatment. It aims to encourage patients to take ownership of their treatment. Specific counselling session plans have been included in the toolkit that provide structured scripts of simple key points to convey to patients, and steps they should follow to overcome commonly experienced barriers to adherence. The initial four sessions are conducted during the intensive phase of treatment (the first three should be conducted within the first 4 weeks of treatment initiation, one of which must be a home visit), with the goals of treatment literacy, stepwise adherence planning, family involvement, contact tracing and infection control advice. In addition to these initial sessions, counselling sessions can occur at any time during treatment to address treatment interruption, the diagnosis of XDR-TB, and treatment failure and palliative care. These additional sessions are particularly important, as they provide detailed scripts for lay counsellors or professional healthcare workers to address very sensitive topics with patients and their families should treatment not yield a successful outcome. Recognising the importance of quality assurance, a counsellor competency assessment for supervisors has also been included in the toolkit.[6]Fig. 1 provides a summary of the timing of the various DR-TB sessions in relation to the patient's journey towards DR-TB treatment completion. Table 1 provides an overview of the contents of the various counselling sessions provided by the DR-TB counsellor to the patient.
While challenges in the implementation of this patient support model can be anticipated, including human resource needs for skilled lay counsellors and their supervision, the structured nature of the approach supports formalised training and monitoring of counsellors and their supervisors. It is further possible to implement counselling sessions in a phased manner to slowly build capacity towards implementing the more specialised XDR-TB and palliative care sessions.
The infrastructure required for the implementation of this toolkit includes four essential components: DR-TB counselling session guides for both the counsellors and their supervisors; adherence plans for patients (Fig. 2); DR-TB flipcharts to use as supportive educational tools during counselling sessions; and a structured training programme for counsellors that contains the tools and exercises necessary to ensure standardised quality of counselling provided to patients.
Conclusions
The counselling toolkit was presented at the 4th Annual South African Tuberculosis Conference held in Durban, SA, on 10 - 13 June 2014. At the conclusion of the conference, the counselling model was recognised for clinical excellence by the organising committee, reinforcing the importance of including a structured patient support component during decentralisation of DR-TB care to primary care level. The DR-TB counsellor is a critical member of the team providing care to patients with DR-TB. It is essential that all DR-TB clinicians, nurses, and counsellors work together to ensure comprehensive support for patients with DR-TB. This support is as essential as the pills patients are required to take every day, and must continue throughout the long DR-TB treatment journey.
Author contributions and funding. EM wrote the article, JH, LS, JC, LW, HD, and VC devised the counselling sessions and toolkit, BB and XH implemented the counselling sessions, and JC, HD, LW and VC assisted with the revision of the article. All the authors reviewed and approved the final article. The counselling toolkit was funded by MSF.
Ethics approval statement. Since this was a retrospective description of the counselling toolkit which involved no data analyses, no ethical approval was needed.
Acknowledgements. We thank the CCTDoH, the Western Cape Province, the National Health Laboratory Service, Khayelitsha clinic staff, the DR-TB counsellors, and most importantly, our patients suffering from DR-TB and HIV in Khayelitsha.
References
1. World Health Organization. Companion Handbook to the WHO Guidelines for the Programmatic Management of Drug-resistant Tuberculosis, 2014. http://apps.who.int/iris/bitstream/10665/130918/1/9789241548809_eng.pdf (accessed 1 August 2014). [ Links ]
2. Ndjeka N. Multi-Drug Resistant Tuberculosis: Strategic Overview on MDR-TB Care in South Africa. National Department of Health, 2014. https://www.msf.org.za/sites/msf.org.za/files/Publications/Strategic_overview_of_MDR_TB_RSA.pdf (accessed 1 January 2015). [ Links ]
3. Calligaro G, Dheda K. Drug-resistant tuberculosis. CME 2013;31(9):344-346. http://www.cmej.org.za/index.php/cmej/article/view/2853/3188 (accessed 1 August 2014). [ Links ]
4. Kendall EA, Theron D, Franke MF, et al. Alcohol, hospital discharge, and socioeconomic risk factors for default from multidrug resistant tuberculosis treatment in rural South Africa: A retrospective cohort study. PLoS One 2013;8(12):e83480. [http://dx.doi.org/10.1371/journal.pone.0083480] [ Links ]
5. Médecins Sans Frontières. Scaling-up diagnosis and treatment of drug-resistant tuberculosis in Khayelitsha, South Africa, 2011. http://www.msfaccess.org/sites/default/files/MSF_assets/TB/Docs/TB_report_ScalingUpDxTxKhaye_ ENG_2011.pdf (accessed 1 August 2014). [ Links ]
6. Médecins Sans Frontières. Patient support interventions to improve adherence to drug resistant tuberculosis treatment: Counselling toolkit, 2014. http://samumsf.org/documents/2014/06/khayelitsha_dr-tb-pt-support.pdf (accessed 1 August 2014). [ Links ]
Accepted 30 May 2015
Corresponding author: E Mohr (msfocb-khayelitsha-drtb-epi@brussels.msf.org)














