Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.105 no.6 Pretoria jun. 2015
http://dx.doi.org/10.7196/SAMJ.9007
RESEARCH
Analysis of referrals and triage patterns in a South African metropolitan adult intensive care service
K GordonI; N AllortoII; R WiseIII
IMB ChB, DA (SA); Department of Anaesthetics, Inkosi Albert Luthuli Central Hospital and School of Clinical Medicine, College of Health Sciences, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
IIMB ChB, MMed (Surg), FCS (SA); Department of Surgery, Edendale Hospital, Pietermaritzburg, and School of Clinical Medicine, College of Health Sciences, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
IIIMB ChB, FCA (SA), MMed (Anaes), Cert Crit Care (SA); Department of Anaesthetics and Critical Care, Edendale Hospital, Pietermaritzburg, and School of Clinical Medicine, College of Health Sciences, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
ABSTRACT
BACKGROUND: Intensive care unit (ICU) beds are scarce resources in low- and middle-income countries. Currently there is little literature that quantifies the extent of the demand placed on these resources or examines their allocation.
OBJECTIVES: To analyse the number and nature of referrals to ICUs in the Pietermaritzburg metropolitan area, South Africa, over a 1-year period, to observe the triage process involved in selecting patients for admission.
METHODS: A retrospective review of the patients referred to ICUs at Grey's and Edendale hospitals, Pietermaritzburg, was performed over a year. The spectrum of patients was evaluated with respect to various demographics, and the current triage process was observed.
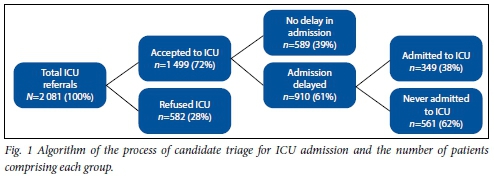
RESULTS: The Pietermaritzburg Metropolitan Critical Care service (PMCCS) received 2 081 patient referrals, 53.4% (1 111/2 081) of males and 46.6% (970/2 081) of females, with a mean patient age of 32 years. The majority of referrals were of surgical patients (39.3%, 818/2 081), followed by medical (18.9%, 393/2 081), trauma (18.6%, 387/2 081) and obstetrics and gynaecology (11.7%, 244/2 081). The chief indications for referral were the need for cardiovascular and respiratory support. Of these referrals, 72.0% (1 499/2 081) were accepted and planned for admission and 28.0% (582/2 081) were refused ICU care. Of the patients accepted, 60.7% (910/1 499) experienced delays prior to admission and 37.4% (561/1 499) were never physically admitted to the units.
CONCLUSIONS: The PMCCS receives a far greater number of patient referrals than it is able to accommodate, necessitating triage. Patient demographics reflect a young patient population referred with chiefly surgical pathology needing physiological support.
Critical care is currently faced with the challenge of resource scarcity and an exponentially increasing demand for intensive care unit (ICU) management.[1] Although this problem is fairly well represented in high-income country (HIC) research, limited literature exists to quantify the burden of critical illness in low- and middle-income countries (LMICs).[2-5] While South Africa (SA) has published data regarding national ICU resources, little is known about the demand placed on them.[6-9]
Global resource restrictions and the growing burden of critical illness necessitate daily ICU triage. This has become an essential step in facilitating efficient utilisation of available ICU facilities, enabling the largest number of patients to benefit.[1-2] However, little consensus exists in terms of how best to conduct this triage, and available international guidelines do not translate well into an LMIC context.[10-11]
Background
The Pietermaritzburg Metropolitan Critical Care service (PMCCS), located in KwaZulu-Natal Province (KZN), SA, comprises two public hospitals. Grey's Hospital is a tertiary hospital with 420-bed capacity and a six-bed ICU. Edendale Hospital, a 900-bed regional hospital, has a six-bed ICU and a three-bed high-care unit (HCU). A 1:1 nurse-to-patient ratio is employed with ICU patients and a 1:2 ratio with HCU patients. Both critical care units are closed, intensivist-led units with the same admission and discharge criteria. The same triage process is utilised by both.
Referral to these units is by formalised written request made on a standardised form. A critical care team member reviews each of the referrals in person. Patients are triaged using the Society of Critical Care Medicine (SCCM) prioritisation model, whereby they are classified according to the severity of their illness, background pathology and prognosis into groups I - IV (Table 1) then either accepted for or refused ICU care.[1] Patients refused on the basis of being too well may be re-referred should their condition deteriorate, but patients deemed too sick are not reconsidered without some form of motivation.

Refusal of admission to an ICU is made on the basis of no perceived benefit for the patient. All patients deemed to derive benefit from ICU management are accepted for admission. Frequent shortages in ICU resources result in delays in admission for some accepted patients. Patients are never refused admission because of a lack of ICU beds, but are rather accepted pending bed availability. Critical care team members review these patients on the wards and guide their management in the form of outreach care. Patients accepted for ICU care are therefore not necessarily always physically admitted to the units.
Objectives
To quantify the current demand for ICU beds in an SA metropolitan area (Pietermaritzburg metropolitan area) and appreciate this region's patient demographics and case mix. The prioritisation process employed to triage referrals was also examined, as were the setbacks encountered during the process of admission to an ICU.
Methods
A retrospective review of all of the patients referred to the ICUs at Grey's and Edendale hospitals over the course of a year was undertaken. The referral proformas generated from both hospitals from March 2013 to the end of February 2014 were used to create a database. The weekly proformas gathered specific data regarding referrals, including basic patient demographics, reason for the referral, acceptance or refusal of admission, and the reason for refusal. Accepted patients were then further divided into those admitted immediately and those who experienced a delayed admission. Reasons for delays were documented.
All patients over the age of 12 years referred to the ICUs at Grey's or Edendale hospitals were included in the study. Referred children less than 12 years of age were excluded, as both units are adult ICUs and the occasional paediatric admission therefore does not reflect the burden of paediatric ICU referrals. No patient identifiers were used. The data were collected retrospectively and therefore indicate practice in the unit. No steps or interventions were undertaken to alter this current practice. Descriptive statistics were used to describe the results.
Results
The PMCCS received a total of 2 081 referrals over a 1-year period (Fig. 1). These referrals consisted of 970 female patients (46.6%) and 1 111 males (53.4%) (Table 2). The majority were between 21 and 40 years old (mean age 32 years, range 13 - 108). General surgery was the discipline referring the most patients, with 818 requests (39.3%). Internal medicine, trauma surgery and obstetrics and gynaecology represented 18.9% (393/2 081), 18.6% (387/2 081) and 11.7% (244/2 081) of referrals, respectively (Table 2).
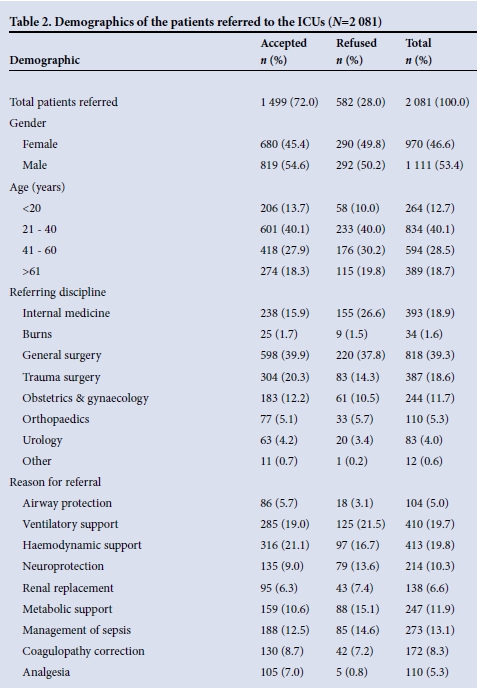
The reasons for referral were primarily for cardiovascular support (19.8%, 413/2 081) and respiratory support (19.7%, 410/2 081). Other reasons included the management of sepsis (13.1%, 273/2 081), metabolic support (11.9%, 247/2 081), neuroprotection (10.3%, 214/2 081), correction of coagulopathy (8.3%, 172/2 081), renal replacement therapy (6.6%, 138/2 081), airway protection (5.0%, 104/2 081) and epidural care and analgesia (5.3%, 110/2 081) (Table 2).
The SCCM prioritisation system indicated that the highest number of referrals (38.5%, 802/2 081) fell into category I. Category II referrals constituted 21.1% of patients (440/2 081), category III 12.3% (257/2 081), and category IV 28.0% (582/2 081) (Table 1).
Of the patients referred, 1 499 (72.0%) were accepted for admission and 582 were refused (Fig. 1). Those refused were either considered too well (53.6%, 312/582) or too severely ill (46.4%, 270/582) to benefit from ICU care. The patients accepted for admission into the unit were representative of the referrals pool. The mean age of patients accepted was 32 years, with 40.1% (601/1 499) falling into the 21 - 40-year age group. Of the patients accepted, 45.4% were females (680/1 499) and 54.6% (819/1 499) males. General surgery represented the referring discipline in 39.9% (598/1 499) of the patients accepted for admission, trauma surgery 20.3% (304/1 499), internal medicine 15.9% (238/1 499), and obstetrics and gynaecology 12.2% (183/1 499) (Table 2). The reasons for admission were primarily cardiovascular and respiratory support, in keeping with the main reasons for referral (Table 2).
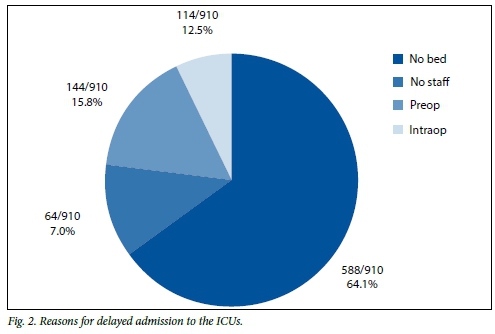
Of the patients accepted for admission, 39.3% (589/1 499) were admitted immediately and the remaining 60.7% (910/1 499) experienced a delay in admission. Delays were predominantly due to resource shortages (Fig. 2). 'No available bed' and 'no available ICU nurse' contributed to 64.6% (588/910) and 7.0% (64/910) of the delays, respectively. The remainder of the delayed admissions were due to patients undergoing surgery, who were either referred preoperatively (15.8%, 144/910) or intraoperatively (12.5%, 114/910).
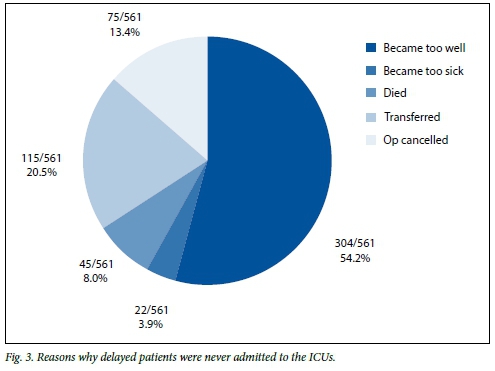
As a result of these delays, 37.4% (561/1 499) of patients accepted for ICU management were never physically admitted into the units. The reasons varied, and are illustrated in Fig. 3. They showed a degree of clinical improvement that meant that their admission was no longer warranted (54.2%, 304/561), had an elective surgical procedure cancelled (13.4%, 75/561), were transferred to another ICU outside the metropolitan area (20.5%, 115/561), deteriorated to an irreversible point (3.9%, 22/561) or died (8.0%, 45/561).
Discussion
Critical care in SA
Critical care in SA faces unique challenges. Not only must it contend with the global issue of resource constraints, but a national focus on primary healthcare has meant that development of additional infrastructure has not occurred.[6,9] Only 23% of all public hospitals are equipped with ICU facilities.[6] Furthermore, disparities in health resource distribution mean that ICUs tend to be located in urban areas, with rural areas having limited or no such facilities.[7] Patient transport services are limited, making inter-hospital transfers tenuous.[7] Disparities in quality of care between units are also recognised, with only 7% of all public sector units functioning in an ideal 'closed' capacity.[6] The well-equipped, specialist-run ICUs in academic hospitals contrast starkly with the basic units that are in operation in regional community hospitals.[8,9] Staff shortages, including shortages of critical care specialists and ICU-trained nurses, are a common problem throughout the country.[8] Guidelines such as those proposed by the American Leapfrog Group regarding gold-standard ICU staffing (critical care specialist-run, closed ICU staffed by ICU-trained nurses) therefore appear unrealistic in the SA setting.[12]
ICUs in the Pietermaritzburg metropolitan area
The Pietermaritzburg metropolitan area is located in KZN, an urbanised province where access to ICU facilities is relatively good, although the ratio of public ICU beds to population is 1:32 000.[9] KZN is a resource-poor setting when compared with international standards such as those in the USA or Germany, where 5 000 and 4 065 individuals, respectively, are served by each ICU bed.[5] Compounding the issue of scarcity is a significantly higher burden of illness and critical illness in this LMIC.[3] Unfortunately, limited evidence currently exists to confirm that the number of ICU beds in KZN is inadequate to serve the population, and data are needed to quantify the extent of the pressure placed on these limited resources.
This study indicates that the demand for ICU beds in the Pietermaritzburg metropolitan area outstrips what is currently available. The two units have 12 ICU beds and 3 HCU beds between them. Our study findings make this deficiency in resources clear - over the course of a year, 2 081 patients were referred to the units but only 938 could be accommodated and were admitted for critical care management (589/938 admitted immediately and 349/938 after a delay). Of the 1 143 patients who were not physically admitted to the units, 556 (48.6%) were considered likely to benefit from ICU management. They included 181 SCCM I patients, 198 SCCM II patients and 177 SCCM III patients. This shows an extreme disparity between need and available resources.
Patient demographics and case-mix of total referrals
Analysis of the patients referred to critical care revealed a fairly equal male-to-female ratio. This contrasts with the only other available SA data, from Chris Hani Baragwanath Academic Hospital in Johannesburg, where a preponderance of male patients was noted as a result of a heavy trauma load.[13] In contrast, our burden of illness is significantly different, general surgery accounting for the greatest number of referrals, while trauma was on par with internal medicine and obstetrics and gynaecology.
A possible explanation for the unexpectedly low number of trauma referrals may be that a relatively large subgroup of patients with severe traumatic brain injuries are often not referred for critical care and neuroprotection owing to a perceived lack of critical care resources or poor prognosis. This hypothesis needs to be explored in future studies. The ICU at Grey's Hospital also functions as a predominantly surgical ICU, a fact that may have hindered referral of medical patients to the unit. KZN has one of the highest HIV prevalence rates in the world.[14] The contribution of HIV to the burden of illness in local critical care patients has not been described, but may influence the current case mix in these units.
The main reasons for referral, a need for active physiological support in an acute setting, appear similar to those seen in other local units and in other LIMCs.[3,4,15] The mean age, which is low when compared with HIC ICUs, is to be expected in SA where average life expectancy is 59.6 years.[3-5,15] However, the wide age range illustrates that we are not immune to the international trend of a growing aged population.
Local triage process
Owing to the supply-demand mismatch of ICU resources, every patient referred undergoes ICU triage. The first step of this triage decision is to exclude and refuse inappropriate referrals - those patients deemed either too well or too ill to benefit from an ICU bed rather than one in a general ward. All the remaining patients were accepted as good candidates for ICU admission. Accepted patients are prioritised using the SCCM model according to the severity of their illness and their long-term prognosis.[1] SCCM I patients are admitted ahead of SCCM II and SCCM III patients.[1]
It is at this point of the process that the triage algorithm in its current form is flawed, as it fails to account for the scarcity of ICU resources. Many of those who are accepted will never be admitted, and if admission occurs it may be delayed, which can have a negative impact on prognosis.
Refusal of patients referred
A significant proportion of our referrals (28.0%, 582/2 081) were refused. When comparing this figure with international data, it should be borne in mind that many of the refusals in HICs are on the basis of no available bed.[1,2,16] In our study, no patient was refused on the basis of no bed, but patients were accepted for admission pending availability of a bed. This discrepancy in detail reduces the significance of comparisons between our study population and international trends. However, if we considered all the patients who were referred and not physically admitted to the units, the figure of 54.9% (1 143/2 081) is significantly higher than current international standards. Triage statistics from the USA quote a figure of 15% of referrals refused admission, while in the UK up to 21% of all patients referred are refused admission.[1,2,16]
Accepted patient demographics and case mix
The demographics of patients accepted for admission to our units are similar to those in resource-poor units in other LMICs.[3,4,15] They tend to be relatively young patients with surgical pathologies, admitted for physiological support, specifically ventilation and/or inotropic therapy. These trends support the idea that the more limited the availability of ICU beds, the more this resource must be reserved for active physiological support of severely ill patients rather than for intensive monitoring purposes.[3-5,5]
The ICU at Grey's Hospital is primarily a surgical unit, while that at Edendale Hospital caters for a mix of surgical and medical patients. It is therefore to be expected that these units will see a relatively high proportion of surgical patients. There are also a significant number of patients (5.3%) accepted for analgesic-related care (primarily epidural management), which according to hospital protocol is not carried out on the wards. Although this number appears high and may indicate a tendency on the part of anaesthetist intensivists to accept more patients for this indication, analgesic care may be necessary to prevent secondary reasons for referral, i.e. respiratory failure in patients with chest trauma. The PMCCS is staffed by a range of physician, surgical and anaesthetist intensivists, and the potential for specialty-related bias in accepting or refusing patients for admission is reduced by the application of the objective SCCM prioritisation model and interdisciplinary discussion.
Study limitations
This study had a retrospective observational design and is susceptible to bias. The proformas were completed on a weekly basis by a different investigator each week. Data collected were therefore subject to inter-individual interpretations. Although several of the patient demographics were standardised in terms of definitions, for example age, gender, referring discipline and SCCM classification, others were less well defined, with the reason for referral being the most problematic. A patient referred with septic shock and requiring inotropic therapy may, for example, have been classified as 'sepsis' or 'cardiovascular support', depending on the investigator completing the proforma. This factor rendered this category of data particularly poor. Data collection was not complete, with 4 weeks of data missing from each institution.
In addition, it should be borne in mind that many referrals may not have been made, the referring disciplines recognising the ICU bed shortages; some patients who required ICU management may therefore have never been referred.
Implications for the future
There is no international consensus on the ideal number of ICU beds per population.[16]
The currently available resources in KZN mean that only 45% of all patients referred may be accommodated in the ICUs, with delays in admission being an unfortunate reality. It is likely that a growing population will continue to outstrip critical care resources.[3] Steps need to be taken in terms of health policy to improve this situation. Further research in this field should describe the demand for critical care on a national level, and once this has been quantified, planning should address the current deficits in resources. The nature of our resource-constrained setting may make this ideal difficult to accomplish. Critics may argue that the cost of development and maintenance of critical care resources could be better spent on the provision of basic primary healthcare. However, an examination of the local patient profile defends the need for improvement in ICU services. Patients are young, with potentially reversible, acute surgical pathologies, and would benefit greatly from active physiological support. It would seem that appropriate planning and simple interventions could save many lives.[3]
In the interim, the current triage system needs to take into account the limits of our available critical care resources. The management of patients who are accepted but face delayed admission owing to shortages of resources needs to be re-evaluated. A possibility includes follow-up for future admission for the SCCM I and II patients only. Although the outreach care provided to patients who are accepted but not admitted seems beneficial, it should be recognised that this form of care places pressure on the critical care team member reviewing these patients on the wards. Such an outreach service may also potentially compromise care of patients already in the critical care units, particularly at night, when a single doctor has to oversee ICU patient care.
The impact of critical care patients who cannot be accommodated in the ICU on the other services in the hospitals also needs to be investigated. Emergency surgical patients who require postoperative critical care frequently spend extended periods in theatre awaiting an available ICU bed. This delay has a knock-on effect, generating backlogs in theatre and resulting in other emergency surgeries being delayed as the anaesthetist continues to provide critical care services to the patient who is waiting.
Conclusion
This study reveals that the PMCCS is unable to accommodate the majority of patients referred. Patient demographics reflect a slight male predominance in a young patient population referred with chiefly surgical diagnoses, typically for various forms of physiological support in the ICU. These admission trends mirror those of other resource-limited units. The experience of this unit in SA, an LMIC, is alarming when compared with that of HICs and mandates significant planning at a national level in the future.
References
1. Task Force of the American College of Critical Care Medicine, Society of Critical Care Medicine. Guidelines for ICU admission; discharge and triage. Crit Care Med 1999;27(3):633-638. [http://dx.doi.org/10.1007/s003900050275] [ Links ]
2. Scheuremann LP, White DB. The ethics and reality of rationing in medicine. Chest 2011;140(6):1625-1632. [http://dx.doi.org/10.1378/chest.11-0622] [ Links ]
3. Fowler R, Adhikari NK, Bhagwanjee S. Clinical review: Critical care in the global context - disparities in burden of illness, access and economics. Crit Care 2008;12(5):225-230. [http://dx.doi.org/10.1186/cc6984] [ Links ]
4. Murthy S, Wunsch H. Clinical review: International comparisons in critical care - lessons learned. Crit Care 2012;16(2):218-224. [http://dx.doi.org/10.1186/cc11140] [ Links ]
5. Prin M, Wunsch H. International comparisons of intensive care: Informing outcomes and improving standards. Curr Opin Crit Care 2012:18(6):700-706. [http://dx.doi.org/10.1097/MCC.0b013e32835914d5] [ Links ]
6. Scribante J, Bhagwanjee S. National audit of critical care resources in South Africa - open versus closed intensive and high care units. S Afr Med J 2007;97(12):1319-1322. [ Links ]
7. Scribante J, Bhagwanjee S. National audit of critical care resources in South Africa - transfer of critically ill patients. S Afr Med J 2007;97(12):1323-1326. [ Links ]
8. Scribante J, Bhagwanjee S. National audit of critical care resources in South Africa - nursing profile. S Afr Med J 2007;97(12):1315-1318. [ Links ]
9. Bhagwanjee S, Scribante J. National audit of critical care resources in South Africa - unit and bed distribution. S Afr Med J 2007;97(12):1311-1314. [ Links ]
10. Christian MD, Joynt GM, Hick JL, Colvin J, Danis M, Sprung CL. Critical care triage: Recommendations and standard operating procedures for ICU and hospital preparations for an influenza epidemic or ass disaster. Intensive Care Med 2010;36(Suppl 1):s55-s64. [http://dx.doi.org/10.1007/s00134-010-1765-0] [ Links ]
11. Wunsch H. A triage score for admission: A holy grail of intensive care. Crit Care Med 2012;40(1):31-33. [http://dx.doi.org/10.1097/CCM.0b013e318236eaa3] [ Links ]
12. Gasperino J. The leapfrog initiative for intensive care unit physician staffing and its impact on intensive care unit performance: A narrative review. Health Policy 2011;102(2-3):223-228. [http://dx.doi.org/10.1016/j.healthpol2011.02.005] [ Links ]
13. Mathivha LR. ICUs worldwide: An overview of critical care medicine in South Africa. Crit Care 2002;6(1):22-23. [http://dx.doi.org/10.1186/cc1449] [ Links ]
14. Statistics South Africa. Mid-year population estimates 2013. http://www.statssa.gov.za/publications/P0302/P03022013.pdf (accessed 4 May 2015). [ Links ]
15. Uche EO, Ezomike UO, Chukwu JC, Ituen MA. Intensive care unit admissions in Federal Medical Centre Umuahia south east Nigeria. Niger J Med 2012;21(1):70-73. [ Links ]
16. Wunsch H. Is there a Starling curve for intensive care? Chest 2012;141(6):1393-1399. [http://dx.doi.org/10.1378/chest.11-2819] [ Links ]
 Correspondence:
Correspondence:
K Gordon
kategordon0@gmail.com
Accepted 21 April 2015.














