Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.105 n.5 Pretoria May. 2015
http://dx.doi.org/10.7196/SAMJ.7686
RESEARCH
Self-monitoring of blood glucose measurements and glycaemic control in a managed care paediatric type 1 diabetes practice
B DaveyI; D G SegalII
IBA Hons (Biokinetics); Wits University Donald Gordon Medical Centre, Johannesburg, South Africa
IIMB BCh, FAAP, FACE; Wits University Donald Gordon Medical Centre, Johannesburg, South Africa
ABSTRACT
BACKGROUND: Intensive diabetes management requires intensive insulin treatment and self-monitoring of blood glucose (SMBG) measurements to obtain immediate information on the status of the blood glucose level and to obtain data for pattern analysis on which meal planning, insulin and lifestyle adjustments can be made. The value and optimal frequency of SMBGs are often questioned
OBJECTIVES: To document the relationship between SMBG frequency and glycaemic control in a managed care paediatric type 1 diabetes practice
METHODS: A retrospective analysis was performed on 141 managed care paediatric and adolescent patients over a 1-year period from 1 February 2010 to 30 January 2011. The patients were stratified according to their insulin regimen. The frequency of SMBG was analysed and glycaemic control measured by glycated haemoglobin (HbA1c
RESULTS: A highly significant decrease (p<0.0001) in HbA1c was found when moving from two injections per day to three- and five-injection regimens. The average HbA1c and its variability reduced as the diabetes regimen became more intensive. A highly significant decrease (p<0.001) in HbA1c levels was detected as the frequency of SMBG increased, with an average decrease of 0.19% in HbA1c per unit increase in the number of SMBG measurements performed per day. The modal frequency of five SMBG measurements per day was required to achieve the American Diabetes Association and International Society for Pediatric and Adolescent Diabetes guideline recommended target HbA1c of <7.5% for a paediatric population
CONCLUSION: A beneficial relationship exists between frequency of SMBG and lower HbA1c in paediatric patients with type 1 diabetes
The Diabetes Control and Complications Trial (DCCT) showed that intensive diabetes treatment designed to achieve near-normoglycaemia substantially reduced the risk of progression and delayed the development of complications in patients with type 1 diabetes when compared with a conventional treatment approach.[1] The Epidemiology of Diabetes Interventions and Complications (EDIC) trial, a follow-on trial from the DCCT and 'clinical experience', highlighted the difficulty of achieving and maintaining near-normoglycaemia in practice.[2] The challenge for healthcare professionals is to devise strategies that help patients to achieve and maintain glycaemic targets safely. Self-monitoring of blood glucose (SMBG) measurements and glycated haemoglobin (HbA1c) have become integral components of intensive diabetes management.[3,4] It is accepted that SMBG can improve compliance with recommendations on diet and exercise and assist with modification of insulin regimens, but some still question its value.[5]
There has been recent debate on the utility of SMBG in Washington State, USA, where the state attempted to limit the number of test strips supplied to do SMBG testing to one test per day in children.[5] However, after consideration it was decided that patients under 18 years of age with type 1 diabetes would be allowed funding for unlimited self-monitoring of blood sugars. This highlights the need for studies on the effectiveness of SMBG in a paediatric population with type 1 diabetes.
Evidence supporting SMBG would need to find a negative correlation between HbA1c and testing frequency. We analysed the relationship between insulin regimen, frequency of SMBG and glycaemic control measured by HbA1c in 141 paediatric and adolescent patients on our diabetes managed care programme.[6]
Methods
Rationale for selection of the study population
The advantage of using this managed care practice was the ability to quantify frequency of SMBG and blood glucose control accurately. Blood glucose test strip dispensing in the practice was tightly linked to the actual frequency of SMBG obtained from individual patients' meter downloads at each visit, and the number of test strips dispensed per year was accurately recorded for each patient. A similar process was followed for insulin use, so that a very accurate estimate of daily insulin use could be obtained. Glycaemic control was measured by means of 3-monthly HbA1c level over the 1-year study period. Care was delivered by the same team over the observation period, the study population remained stable with no turnover of patients in the group, and all supplies were obtained from a single source.
A total of 141 patients aged 2 - 18 years with type 1 diabetes were included in the retrospective analysis from 1 February 2010 to 30 January 2011. To exclude the effect of the 'honeymoon period', only patients who had been diagnosed for >1 year were included. Patients were stratified according to the number of injections they received per day in their treatment regimen. Patients receiving premixed insulin twice daily were classified as being on a two injections per day regimen; if a lunchtime injection of bolus insulin was added they were classified as being on three injections per day. The remainder of the patients were receiving basal insulin at breakfast and dinner or bedtime and bolus insulin at major meals, and were classified as being on five injections per day. No patients were receiving four injections per day. Patients on continuous subcutaneous insulin infusion (CSII) therapy were classified separately. The number of SMBG measurements per day was analysed, as well as total daily dose of insulin and injection regimen. The mean of each patient's HbA1c over the study period was calculated from the average of their 3-monthly tests. All tests were performed on the same DCA Vantage Analyzer (Siemens Medical Solutions Diagnostics, USA).
Results
A total of 141 patients (74 male) were studied. The mean age was 11.7 years (range 2 - 18), the mean duration of diabetes was 4.7 years (range 1 - 12), and the mean amount of insulin used was 0.95 U/kg/d (range 0.3 - 1.47). Nine patients were receiving two injections per day (6.3%), 19 three injections per day (13.5%), 49 five or more injections per day (34.8%), and 64 CSII (45.4%).
Injection regimen
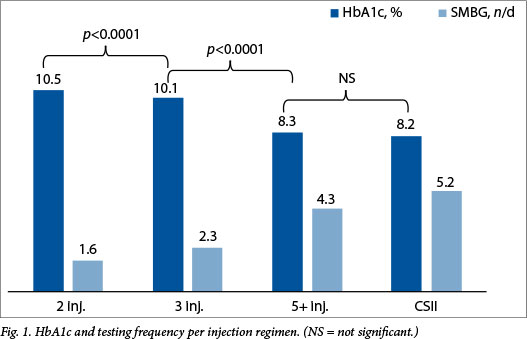
There was a highly significant decrease (p<0.0001) in HbA1c levels when comparing patients receiving two, three and five injections per day, but the difference in HbA1c levels between five injections per day and CSII was not significant (Fig. 1). The HbA1c standard deviations also differed significantly (p<0.0001) across the four groups, displaying the same pattern as the averages (Table 1). The HbA1c decreased as the number of injections per day increased.
Frequency of testing per day
There was a highly significant decrease (p<0.001) in HbA1c levels as the frequency of testing increased, with an estimated average decrease of 0.34% per unit increase in the number of SMBG measurements per day (Fig. 2). Using analysis of covariance to correct for the simultaneous effect of the injection regimen, the average decrease in HbA1c was 0.19% per unit increase in SMBG measurements per day (p<0.001). Those on the two injections per day regimen performed on average 1.6 SMBG measurements per day, those on the three-injection regimen 2.3 per day, those on five injections 4.3 per day, and those on CSII 5.2 per day. In our cohort, patients achieving an American Diabetes Association and International Society for Pediatric and Adolescent Diabetes target HbA1c level of <7.5% (International Federation of Clinical Chemistry 58 mmol/mol)[15] had a modal testing frequency of five tests per day, ranging from one to nine SMBG tests per day.

Discussion
The goal of SMBG is to obtain useful information with which to maintain and manage overall glucose status, with an ultimate goal of achieving 'normoglycaemia' and preventing the long-term complications associated with poor glycaemic control. There are two main reasons for obtaining blood glucose data. The first is to obtain immediate information on the status of the blood glucose level, so that hypoglycaemia and hyperglycaemia can be minimised through timely and meaningful interventions. The second is to obtain data for pattern analysis according to which meals can be planned, insulin dosages calculated and lifestyle adjustments made.
Certain fundamental behaviours are associated with better glycaemic control,[7] such as the frequency of SMBG measurement,[8] frequency of insulin injections,[1] absence of insulin omission,[9] adherence to meal planning[10] and patient-initiated dose adjustments.[11,12] These behaviours are the responsibility of each patient and caregiver, with non-adherence resulting in poor diabetic control.
SMBG is a painful, costly and onerous task that has become part and parcel of modern-day diabetes management. Numerous testing regimens exist, with little evidence to suggest superiority of one over another. To be beneficial, SMBG needs to be a 'value add' to the patient and the medical team. Often patients are not empowered to analyse their SMBG data or to adjust their insulin dosages. This disempowerment may lead to apathy, depression, and conflict within the family. Such patients see minimal benefit from testing, leading to a decline in actual testing frequency, and perhaps even data corruption and embellishment, so that an accurate picture of their glycaemic control becomes impossible to obtain.[13]
To the healthcare professional, accurate SMBG data are a valuable aid to the clinical assessment on the basis of which treatment adjustments can be recommended. Other studies support a correlation between frequency of testing and HbA1c reduction.[8,14] Our study supports these findings, showing a 0.19% improvement in HbA1c per unit increase in the number of SMBG measurements performed per day after correcting for the injection regimen.
One of the limitations of this study is the interdependence of testing frequency and injection regimen. Both the injection regimen and testing frequency influenced the HbA1c. However, analysis of covariance continued to show that testing frequency had a highly significant negative effect on the HbA1c in this study (p=0.0002).
Patients receiving fixed dosages of premixed insulin (i.e two- or three-injection regimen) often perform fewer SMBG measurements. There are two possible explanations for this: patients who volunteer for less intensive regimens such as fixed-dosage premixed insulin also opt to perform fewer SMBG tests per day; and fewer SMBG measurements are required in the day-to-day management of glucose control on this two- or three-injection regimen than on a more intensive regimen of five injections per day.
On more intensive regimens, in particular on CSII therapy, patients are preselected according to their ability to perform multiple SMBG measurements a day, and are required to do so to verify the integrity of the pump function in terms of insulin delivery. The only group in which the testing frequency is less influenced by the injection regimen is the five injections per day group. Sub-analysis of this group using regression analysis still found a significant negative correlation between frequency of SMBG measurement and HbA1c (p=0.001).
SMBG provides data in the form of an output variable that is a summation of a number of input variables such as insulin dose, insulin type, carbohydrate load and exercise. An increase in testing frequency allows for multiple hypotheses to be tested. The cycle of testing and modification of the input variables strives through each iteration to achieve predictable and desirable glycaemic outcomes. Finding the perfect testing frequency and intensity is a subject of ongoing research.
Overall, the study revealed a positive inverse relationship between frequency of SMBG measurements per day and HbA1c after correcting for the insulin regimen.
Conclusion
SMBG is essential for monitoring daily glycaemic control and for detecting and acutely managing hyper- and hypoglycaemic episodes. It also provides data for pattern analysis that can be used to reinforce positive behaviours and reduce negative ones. SMBG analysis assists in meal planning and dosage adjustment, and in so doing minimises glycaemic variability and allows patients to obtain recommended HbA1c targets. A clear beneficial relationship exists between the frequency of SMBG measurements performed per day and a lower HbA1c in paediatric patients with type 1 diabetes. While a tailored approach is required for each patient, restricted access to SMBG test strips should not be allowed to handicap a patient's diabetes control efforts.
References
1. Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329(14):977-986. [http://dx.doi.org/10.1056/NEJM199309303291401] [ Links ]
2. Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Research Group. Modern-day clinical course of type 1 diabetes mellitus after 30 years' duration. Arch Intern Med 2009;169(14):1307-1316. [http://dx.doi.org/10.1001/archinternmed.2009.193] [ Links ]
3. Hansen MV, Pedersen-Bjergaard U, Hellers SR, et al. Frequency and motives of blood glucose self-monitoring in type 1 diabetes. Diabetes Res Clin Pract 2009;85(2):183-188. [http://dx.doi.org/10.1016/j.diabres.2009.04.022] [ Links ]
4. Karter AJ, Ackerson LM, Darbinian JA, et al. Self-monitoring of blood glucose levels and glycemic control: The Northern California Kaiser Permanente Diabetes Registry. Am J Med 2001;111(1):1-9. [http://dx.doi.org/10.1016/S0002-9343(01)00742-2] [ Links ]
5. Washington State Health Care Authority. HTA program, glucose monitoring, self-monitoring in patients under 18 years of age. Health Technol Assess 2011;1-53. http://www.hta.hca.wa.gov/documents/glucose_monitoring_draft.pdf (accessed 25 May 2011). [ Links ]
6. Distiller LA, Brown MA, Joffe BI, Kramer BD. Striving for the impossible dream: A community-based multi-practice collaborative model of diabetes management. Diabet Med 2010;27(2):197-202. [http:// dx.doi.org/10.1111/j.1464-5491.2009.02907.x] [ Links ]
7. Miller VA, Drotar D. Decision-making competence and adherence to treatment in adolescents with diabetes. J Pediatr Psychol 2007;32(2):178-188. [http://dx.doi.org/10.1093/jpepsy/jsj122] [ Links ]
8. Ziegler R, Heidtmann B, Hilgard D, Hofer S, Rosenbauer J, Holl R; DPV-Wiss-Initiative. Frequency of SBGM correlates with HbA1c and acute complications in children and adolescents with type 1 diabetes. Pediatr Diabetes 2011;12(1):11-17. [http://dx.doi.org/10.1111/j.1399-5448.2010.00650.x] [ Links ]
9. Peyrot M, Rubin RR, Kruger DF, Travis LB. Correlates of insulin injection omission. Diabetes Care 2010;33(2):240-245. [http://dx.doi.org/10.2337/dc09-1348] [ Links ]
10. Pastors JG, Warshaw H, Daly A, Franz M, Kulkarni K. The evidence for the effectiveness of medical nutrition therapy in diabetes management. Diabetes Care 2002;25(3):608-613. [http://dx.doi.org/10.2337/diacare.25.3.608] [ Links ]
11. Heller S, DAFNE Study Group. Training in flexible, intensive insulin management to enable dietary freedom in people with type 1 diabetes: Dose adjustment for normal eating (DAFNE) randomised controlled trial. BMJ 2002;325:746. [http://dx.doi.org/10.1136/bmj.325.7367.746] [ Links ]
12. Anderson RM, Funnell MM, Butler PM, Arnold MS, Fitzgerald JT, Feste CC. Patient empowerment: Results of a randomized controlled trial. Diabetes Care 1995;18(7):943-949. [http://dx.doi.org/10.2337/diacare.18.7.943] [ Links ]
13. Gonder-Frederick LA, Julian DM, Cox DJ, Clarke WL, Carter WR. Self-measurement of blood glucose: Accuracy of self-reported data and adherence to recommended regimen. Diabetes Care 1988;11(7):579-585. [http://dx.doi.org/10.2337/diacare.1L7.579] [ Links ]
14. Schutt M, Kern W, Krause U, et al.; DPV Initiative. Is the frequency of self-monitoring of blood glucose related to long-term metabolic control? Multicenter analysis including 24,500 patients from 191 centers in Germany and Austria. Exp Clin Endocrinol Diabetes 2006;114(7):384-388. [http://dx.doi.org/10.1055/s-2006-924152] [ Links ]
15. IDF-ISPAD Diabetes in Childhood and Adolescence Guidelines. 2011. http://www.ispad.org/sites/default/files/resources/files/idf-ispad (accessed 25 May 2011). [ Links ]
 Correspondence:
Correspondence:
D Segal
david@endo.co.za
Accepted 18 March 2015














