Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.105 n.5 Pretoria May. 2015
http://dx.doi.org/10.7196/SAMJ.8996
FORUM
ISSUES IN PUBLIC HEALTH
The simple bread tag - a menace to society?
R KarroI; P GoussardII; J LoockIII; R GieIV
IMB ChB, FCORL (SA), is currently a specialist in private practice and holds a sessional post in state practice. At the time of writing the article he was a senior registrar in the Department of Otorhinolaryngology, Tygerberg Hospital and Faculty of Health Sciences, Stellenbosch University, Cape Town, South Africa. Dr
IIMB ChB, MMed, Cert Pulmonol Paed (SA), PhD, is a senior specialist in the Paediatric Pulmonology Unit, Department of Child Health and Paediatrics, Tygerberg Hospital and Faculty of Health Sciences, Stellenbosch University. Prof
IIIMB ChB, FCS (SA) ORL, is Head of Otorhinolaryngology, Tygerberg Hospital and Faculty of Health Sciences, Stellenbosch University
IVMB ChB, MMed (Paed), FCPaed (SA), is Head of Paediatric Pulmonology, Department of Child Health and Paediatrics, Tygerberg Hospital and Faculty of Health Sciences, Stellenbosch University
ABSTRACT
Foreign bodies (FBs) are potentially life-threatening when inhaled by a child, depending on where they lodge. Symptoms can range from acute upper airway obstruction to mild, vague respiratory complaints. Between 80% and 90% of inhaled FBs occlude the bronchi, while the larynx is a less common site. The commonest inhaled paediatric FBs are organic, e.g. seeds or nuts. Plastic FBs are less common and more difficult to diagnose. They are generally radiolucent on lateral neck radiographs and are often clear and thin. We report three cases of an unusual plastic laryngeal FB, the bread tag. Plastic bread tags were first reported in the medical literature as an ingested gastrointestinal FB in 1975. Since then, over 20 cases of gastrointestinal complications have been described. We report what is to our knowledge the first paediatric case of an inhaled bread tag, and also the first case series, briefly discuss the symptoms and options for removal of laryngeal FBs, and highlight the dangers of the apparently harmless bread tag. Images of the bread tags in situ and after their removal are included.
Foreign bodies (FBs) are potentially life-threatening when inhaled by a child, depending on where they lodge. Symptoms can range from acute upper airway obstruction (UAO) to mild, vague respiratory complaints.
An inhaled FB is one of the most common causes of accidental death in children under 1 year of age. The risk of inhalation remains high up to the age of 3 years.[1] The increased incidence of inhalation in this age group is due to the young child's inherent curiosity in exploring the environment orally, faster respiratory rate and work of breathing, and under-developed teeth.
The commonest inhaled paediatric FBs are organic, e.g. seeds or nuts. Plastic FBs are less common and more difficult to diagnose. They are generally radiolucent on a chest radiograph and are often clear and thin. These features also contribute to plastic FBs being missed on flexible nasopharyngoscopy and direct laryngoscopy.[2] The majority (80 -90%) of inhaled FBs occlude the bronchi, while the larynx is a less common site.[2]
Three children presented at Tygerberg Children's Hospital, Cape Town, South Africa, between January 2011 and June 2012 with an unusual yet ubiquitous plastic laryngeal FB: the common bread tag.
Case series
Case 1
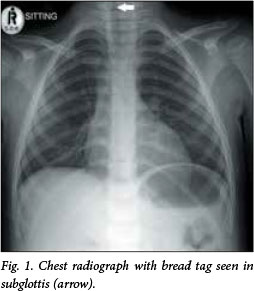
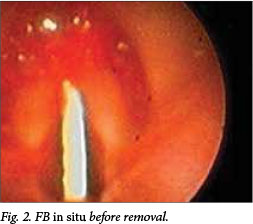
The first patient was a 4-year-old girl brought in by her mother, who had seen her ingesting a bread tag earlier that day. She had obvious dysphonia and inspiratory stridor but no respiratory distress. The chest radiograph showed features highly suggestive of an FB in the subglottis (Fig. 1), and flexible nasendoscopy revealed the bread tag lodged sagittally between the vocal cords with surrounding oedema (Fig. 2). An urgent procedure was done to remove the bread tag under general anaesthesia via a combination of flexible and rigid bronchoscopy. This proved to be challenging, as the bread tag was broken in half (Fig. 3) and its sharp points were embedded in the subglottic mucosa. Following removal, the child was kept intubated overnight. Upon extubation, she had no further stridor and was subsequently discharged without any respiratory sequelae.

Case 2
The second patient was a 15-month-old boy referred to our unit with a 5-day history of UAO non-responsive to medical management. He was initially seen at a day hospital with UAO, nebulised and sent home. Two days later he returned with worsening symptoms. According to his mother, the symptoms had been of sudden onset. There was no history of choking or coughing.
He had a previous history of mild asthma, controlled on metered-dose inhalers.
On arrival, he was not acutely distressed and looked deceptively well. His oxygen saturation was 94%, although he had inspiratory and expiratory stridor, a sternal tug and a pulsus paradoxus. A chest radiograph showed what looked like an FB in the subglottis and some segmental collapse of the right upper zone. Flexible bronchoscopy carried out as an urgent procedure revealed an incomplete bread tag (Fig. 4) wedged firmly between the vocal cords. This was removed with the flexible bronchoscope and the child was monitored overnight in the high-care unit while receiving three doses of dexamethasone. The following day he was well and was discharged.

Case 3
The third patient was an 8-month-old girl who was referred to our unit from a district hospital, with a history of the grandmother having found the child with a piece of plastic in her mouth: 'She suddenly swallowed it, choked and became blue.' After being shaken the child started to breathe again, but subsequently developed noisy breathing. On arrival, she was not distressed but had obvious inspiratory stridor. Flexible bronchoscopy was performed as an urgent procedure, and an intact bread tag was found lodged in the subglottis. It proved too difficult to remove in one piece, so it was pushed down into the right main bronchus and then removed piecemeal via a combination of rigid and flexible bronchoscopy. The child was given a single dose of intravenous dexamethasone 4 mg and monitored in the paediatric intensive care unit overnight. By the following day the stridor had resolved, and she was discharged a day later.
The bread tag
Plastic bread tags, otherwise known as occlupanids (from the Latin occlu, to close, and pan, bread), were developed by Floyd G Paxton, founder of Kwik Lok, USA, in 1952.[3] They have the obvious advantage of being easily reusable. They were first reported in the medical literature as an ingested gastrointestinal FB in 1975.[3] Since then over 20 cases of gastrointestinal complications have been described, ranging from bowel obstruction to perforation,[3] with at least three reported deaths.[4] Rosow et al.[5] reported the first case of an inhaled bread tag, which lodged in the subglottis of an adult. We have reported what is to our knowledge the first paediatric case of an inhaled bread tag, and also the first case series.
Laryngeal FBs
In a retrospective study by Bloom et al.[2] of 185 aspirated FBs, nine (5%) were found to be laryngeal. A laryngeal FB can either lodge at the glottic level or wedge in the subglottis. The subglottis, being the narrowest part of the paediatric larynx, is classically where these laryngeal FBs lie. The unique feature of a subglottic FB is that it is usually small enough to fit through the vocal cords, but often has sharp edges that embed in the subglottic mucosa.[6] The confined subglottic space adds to the difficulty of removal and the development of ensuing oedema.
Symptoms oflaryngeal FBs differ from other tracheobronchial FB aspirations, and they are often more difficult to diagnose. Laryngeal FBs can be separated into two categories: large, conforming items that obstruct the laryngeal inlet causing immediate respiratory distress, and sharp, thin, aerodynamic FBs causing partial obstruction.[2] Partial laryngeal obstruction can cause variable and sometimes subtle symptoms mimicking other causes of upper airway obstruction. These symptoms include dysphonia, cough, stridor, wheeze and dyspnoea. Additionally, thin laryngeal FBs are frequently radiolucent on a chest radiograph without the typical lung features of unilateral air trapping or mediastinal shift, making diagnosis with standard imaging difficult.[2] General practitioners and emergency room doctors need to have a high index of suspicion in the face of a nonspecific history and a normal plain radiograph.
How are they removed?
In two of our three cases, the bread tag was broken in half exposing the clasping teeth, which impacted in the subglottic mucosa. This made removal difficult and traumatic. Virtually all inhaled FBs can be extracted via bronchoscopy, with success rates of over 98%.[7] Rigid bronchoscopy is the standard technique for removal, but flexible bronchoscopy, often the technique used to remove an FB in an awake adult, is becoming increasingly used. In children it is generally used for the initial diagnostic procedure and thereafter may be used for the removal, depending on the individual circumstance and expertise. It is considered to be less traumatic than rigid bronchoscopy and can be particularly useful for retrieving FBs lodged more distally in the tracheobronchial tree. Rigid bronchoscopes are advantageous in that they are bigger in diameter, allowing larger FB removal, aspiration of thick secretions and better patient ventilation.[7] Rigid endoscopes also have excellent optical visualisation and a wider array of ancillary instrumentation.[8] Generally, teams should be trained in both rigid and flexible bronchoscopy. In our three patients a combination of both techniques was used, but in the third case the rigid endoscope proved to be most useful for removing the larger intact bread tag.
The dangers of breadtags
The dangers of bread tags have been highlighted by previous authors. Some have suggested redesigning them to make them less hazardous, for example enlarging them, thereby minimising the chance of their being swallowed,[4] removing the sharp edges, or manufacturing them out of a radio-opaque material.[7] Others have called for complete cessation of their manufacture.[9-11]
Bread tags are often made of brightly coloured plastic and are therefore attractive to young children. They appear harmless, and most parents, and indeed most doctors, are probably unaware that they are dangerous.[10] We agree with those who call for complete elimination of bread tags and replacing them with a safer option.[10,11]
While bread tags are still in circulation, we advise that they should be removed from the bread packet as soon as they are brought into the home and stored safely out of reach of young children. Alternatively, they can be donated to a worthy cause such as 'bread tags for wheelchairs',[12] a local non-profit organisation that raises funds from recycling the bread tags to buy wheelchairs for those who cannot afford them.
Conclusion
We hope that this series of three cases of laryngeal obstruction by an apparently harmless household object, the plastic bread tag, will draw the attention of the medical fraternity and indeed the public to the potential menace that these ubiquitous items represent. These tags should be redesigned in a safer format, or removed from use.
References
1. Cohen S, Avital A, Godfrey S, et al. Suspected foreign body inhalation in children: What are the indications for bronchoscopy? J Pediatr 2009;155(2):276-280. [http://dx.doi.org/10.1016/j.jpeds.2009.02.040] [ Links ]
2. Bloom DC, Christenson TE, Manning SC, et al Plastic laryngeal FBs in children: A diagnostic challenge. Int J Pediatr Otorhinolaryngol 2005;69(5):657-662. [http://dx.doi.org/10.1016/j.ijporl2004.12.006] [ Links ]
3. Lehmer LM, Ragsdale BD, Daniel J, et al. Plastic bag clip discovered in partial colectomy accompanying proposal for phylogenic plastic bag clip classification. BMJ Case Rep 2011, published online 5 September 2011. [http://dx.doi.org/10.1136/bcr.02.2011.3869] [ Links ]
4. Sutton G. Hidden dangers of sliced bread. BMJ 1984;28:1995. [http://dx.doi.org/10.1136/bmj.288.6435.1995-b] [ Links ]
5. Rosow DE, Chen S. Office removal of a subglottic bread clip. Case Rep Otolaryngol Volume 2013 (2013), Article ID 480676, 3 pages. [http://dx.doi.org/10.1155/2013/480676] [ Links ]
6. Halvorson DJ, Merritt RM, Mann C, Porubsky ES. Management of subglottic foreign bodies. Ann Otol Rhinol Laryngol 1996;105(7):541-544. [http://dx.doi.org/10.1177/000348949610500709] [ Links ]
7. Rodrigues AJ, Oliveira EQ, Scordamaglio PR, et al. Flexible bronchoscopy as the first-choice method of removing foreign bodies from the airways of adults. J Bras Pneumol 2012;38(3):315-320. [http://dx.doi.org/10.1590/S1806-37132012000300006] [ Links ]
8. Swanson KL, Prakash UBS, Midthun DE. Flexible bronchoscopic management of airway foreign bodies in children. Chest 2002;121(5):1695-700. [http://dx.doi.org/10.1378/chest.12L5.1695] [ Links ]
9. Beer TW. Fatalities from bread tag ingestion. Med J Aust 2002;176(10):506. [ Links ]
10. Ellul J, Hodgkinson PD. Problems with a plastic bread bag clip. Arch Emerg Med 1987;6(2):156-157. [http://dx.doi.org/10.1136/emj.6.2.156] [ Links ]
11. Tang A, Kong AB, Walsh D, Verma R. Small bowel perforation due to a plastic bread bag clip: The case for clip redesign. Aust NZ J Surg 2005;75(5):360-362. [http://dx.doi.org/10.1111/j.1445-2197.2005.03356.x] [ Links ]
12. http://www.breadtagsforwheelchairs.co.za (accessed 7 April 2015). [ Links ]
 Correspondence:
Correspondence:
R Karro
rkarro@iname.com
Accepted 18 March 2015














