Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.105 no.2 Pretoria feb. 2015
http://dx.doi.org/10.7196/samj.9269
CONTINUING MEDICAL EDUCATION
CASE REPORT
Schistosomiasis misdiagnosed as abdominal tuberculosis
S N BotesI; S B IbirogbaII; D KahnIII
IMB ChB;Surgical Unit, Rob Ferreira Hospital, Nelspruit, South Africa
IIFCS (SA), MMed;Department of Surgery, Faculty of Health Sciences, Groote Schuur Hospital and University of Cape Town, South Africa
IIIMB ChB, FCS (SA), ChM; Department of Surgery, Faculty of Health Sciences, Groote Schuur Hospital and University of Cape Town, South Africa
ABSTRACT
Schistosomiasis (also termed bilharzia, after the tropical disease specialist Theodor Bilharz) is a waterborne parasitic infection. It was first described in the appendix in 1909, but despite awareness of the disease for more than a century, few data on its exact incidence are available.
Schistosomiasis is a waterborne parasitic infection.[1] Few data on its exact incidence are available.[2] We report a case of a missed diagnosis of the disease.
Case report
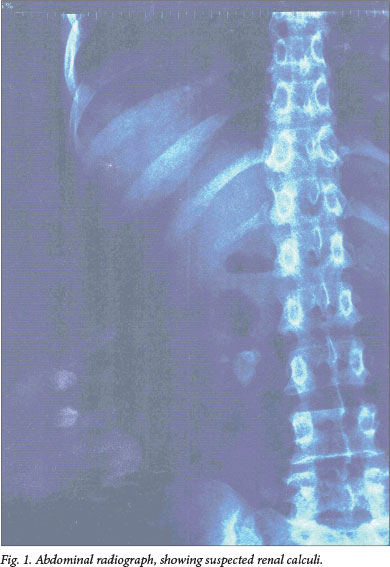
A 36-year-old woman presented to her general practitioner on 2 March 2012, complaining of a 2-week history of abdominal pain. Clinically, she had a right iliac fossa (RIF) mass, which was confirmed on an ultrasound scan. She was seen at the outpatient clinic at Rob Ferreira Hospital (RFH), Nelspruit, South Africa (SA), on 5 March 2012. A pregnancy test was negative. The patient was found to be HIV-positive, with a CD4 count of 23 cells/μΚ She was apyrexial, with a white cell count (WCC) of 6.84 x 109/L and a C-reactive protein (CRP) level of 118 mg/L. A urine dipstick test showed nitrites 3+, leucocytes 2+, blood - positive, and protein - positive. Urine culture subsequently revealed Proteus mirabilis, which was sensitive to ampicillin. An abdominal radiograph showed possible renal calculi (Fig. 1). The patient was scheduled for an ultrasound scan of the abdominal mass at the outpatient clinic and follow-up visits at the urology and gynaecology clinics.
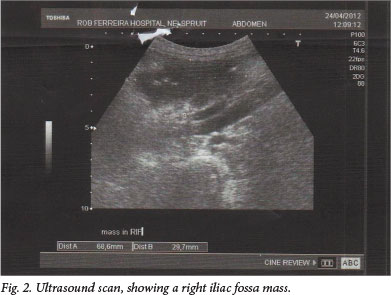
An ultrasound scan on 24 April 2012 at RFH revealed a large mass of para-aortic lymph nodes, with a poorly circumscribed RIF mass of 69 x 30 mm (Fig. 2). The liver and spleen were normal and no renal calculi were seen. The gynaecology team ruled out pelvic inflammatory disease. The Surgery Unit requested a computed tomography (CT) scan of the abdomen and a sputum specimen for tuberculosis (TB) diagnosis (no record of the latter could, however, be found).
The CT scan confirmed the mass in the region of the ileo-caecal junction, with narrowing of the caecum. The CRP was now 311 mg/L, erythrocyte sedimentation rate (ESR) 125 mm/h, and WCC 14.12 x 109/L. The patient was not acutely ill and was scheduled for a colonoscopy on 11 May 2012.
On 1 May 2012 the patient presented again, complaining of chronic diarrhoea. She had also started antiretroviral therapy. She had night sweats and a temperature of 39.20C. She required two units of blood and was deemed unfit for colonoscopy. Based on the clinical signs and symptoms, high ESR, radiograph and RIF mass with multiple abdominal lymph nodes, the patient was diagnosed with abdominal TB on 2 May 2012 and started on TB treatment.
She returned on 6 June 2012 for a colonoscopy, which confirmed the caecal mass. A biopsy was taken, a rigid sigmoidoscopy was performed for a grade 3 haemorrhoid, and another biopsy was taken. Neither of these biopsy results are available. At this stage, her CD4 count was 101 cells^L. She completed her TB treatment, but was lost to follow-up.
On 17 June 2013 she presented to the RFH casualty department with an acute abdomen and generalised peritonitis. She had a CRP of 205 mg/L, a WCC of 7.89 x 109/L, and an ESR of 65 mm/h. On 19 June 2013 the patient underwent an emergency laparotomy, which revealed a perforated jejenum and terminal ileum. A limited right hemicolectomy was performed, and an ileostomy was made. On 27 June 2013 the histology report confirmed schistosomiasis (Schistosoma haematobium). The patient was started on praziquantel, and discharged on day 13 after the laparotomy.
She made a good recovery and her ileostomy was reversed on 26 November 2013; during this procedure her bowel appeared macroscopically normal.
Discussion
RFH is the referral hospital for the Lowveld region of SA. Not only is schistosomiasis endemic in the area, but we also treat numerous patients from neighbouring countries, i.e. Mozambique and Swaziland, which results in an increased number of patients with tropical diseases being treated at our hospital.
Schistosomiasis is a waterborne trematode infection that spreads through direct contact with the human skin. It is one of the most common parasitic infections, and occurs in well-defined geographical areas. This pattern is, however, changing owing to migration across borders.[2] Despite advances in the treatment of schistosomiasis, there is evidence of its spread to new geographical areas and resistance to praziquantel.[3]
Different subtypes of schistosomiasis affect different systems, mainly the genito-urinary tract (S. haematobium), gastrointestinal tract (GIT), and the liver (S. mansoni and S. japonicum). Symptoms are caused by the host's immune response to the antigens secreted by the schistosoma eggs, leading to a granulomatous reaction.[4] a definitive diagnosis of schistosomiasis is made by observing the eggs in either urine or stool. Sometimes up to three specimens might be required. Rectal or bladder biopsy is the most sensitive test, but also more invasive. Antibody testing is useful in certain cases, but limited because of persistence after parasitic cure.[5] In our study, urine was sent for microscopy, culture and sensitivity, but no schistosoma were identified. Stool samples were not sent in order to exclude schistosomiasis. The biopsy that was done during the colonoscopy could have been of great benefit, but the patient was initially lost to follow-up, and the results could not be found in our records.
Symptoms experienced by the host with GIT involvement include colicky abdominal pain, either in the hypogastrium or RIF. Diarrhoea alternating with constipation and occult or frank blood in the stool are also seen.[6] Our patient experienced both colicky RIF pain and diarrhoea. No comment was made about blood in her stool.
The diagnosis of TB of the abdomen was never confirmed, and was based on the clinical findings, raised ESR, low CD4 count, and radiological findings (even though the ultrasound scan was not convincing of TB of the abdomen). The diagnosis of schistosomiasis was, however, confirmed on histological examination, and the patient showed significant improvement after a course of praziquantel. It is therefore assumed that the original diagnosis was incorrect, and that the patient suffered from abdominal schistosomiasis.
The incidence of this disease at RFH is unknown, but as the Lowveld region of SA is an endemic area, schistosomiasis should always be considered in the differential diagnosis of a patient with a chronic, vague abdominal mass.
References
1. Ross AGP, Bartley PB, Sleigh AC, et al Schistosomiasis. N Engl J Med 2002;346(16):1212-1220. [ Links ]
2. Madavo C, Hurriez H. Schistosomiasis of the appendix. J R Soc Med 2006;99:473. [ Links ]
3. Patz J, Graczyk T, Geller N, et al. Effects of environmental change on emerging parasitic disease. Int J Parasitol 2000;30:1395-1405. [http://dx.doi.org/10.1016/S0020-7519(00)00141-7] [ Links ]
4. Boros DL, Warren KS. Delayed hypersensitivity-type granuloma formation and dermal reaction induced and elicited by a soluble factor isolated from S. mansoni eggs. J Exp Med 1970;132:488-507. [http://dx.doi.org/10.1084/jem.132.3.488] [ Links ]
5. Tsang VC, Wilkins PP. Immunodiagnosis of schistosomiasis. Immunol Invest 1997;60:960-966. [ Links ]
6. Chen MC, Wang SC, Chang PY, et al Granulomatous disease of the large intestine secondary to Schistosome infestation: A study of 229 cases. Chin Med J (Engl) 1978;4:371-378. [ Links ]
 Correspondence:
Correspondence:
S N Botes
snbotes@gmail.com














