Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.105 n.1 Pretoria Jan. 2015
http://dx.doi.org/10.7196/SAMJ.9099
CONTINUING MEDICAL EDUCATION
ARTICLE
Severe food allergy and anaphylaxis: Treatment, risk assessment and risk reduction
S M Risenga; M Kriel; S Karabus; A I Manjra; C L Gray; E Goddard; A C Lang; A J Terblanche; D A van der Spuy; M E Levin; for the South African Food Allergy Working Group (SAFAWG)
All authors' degrees, affiliations and conflict of interest statements can be found online at http://dx.doi.org/10.7196/SAMJ.9201
ABSTRACT
An anaphylactic reaction may be fatal if not recognised and managed appropriately with rapid treatment. Key steps in the management of anaphylaxis include eliminating additional exposure to the allergen, basic life-support measures and prompt intramuscular administration of adrenaline 0.01 mg/kg (maximum 0.5 mL). Adjunctive measures include nebulised bronchodilators for lower-airway obstruction, nebulised adrenaline for stridor, antihistamines and corticosteroids. Patients with an anaphylactic reaction should be admitted to a medical facility so that possible biphasic reactions may be observed and risk-reduction strategies initiated or reviewed after recovery from the acute episode. Factors associated with increased risk of severe reactions include co-existing asthma (and poor asthma control), previous severe reactions, delayed administration of adrenaline, adolescents and young adults, reaction to trace amounts of foods, use of non-selective ß-blockers and patients who live far from medical care. Risk-reduction measures include providing education with regard to food allergy and a written emergency treatment plan on allergen avoidance, early symptom recognition and appropriate emergency treatment. Risk assessment allows stratification with provision of injectable adrenaline (preferably via an auto-injector) if necessary. Patients with ambulatory adrenaline should be provided with written instructions regarding the indications for and method of administration of this drug and trained in its administration. Patients and their caregivers should be instructed about how to avoid foods to which the former are allergic and provided with alternatives. Permission must be given to inform all relevant caregivers of the diagnosis of food allergy. The patient must always wear a MedicAlert necklace or bracelet and be encouraged to join an appropriate patient support organisation.
Management of acute allergic reactions to food
There are no recommended medications for the prevention of immunoglobulin E (IgE)-mediated, non-IgE-mediated or mixed food-induced allergic reactions.[1,2] Medication may, however, be used to treat both severe and non-severe allergic reactions. While treating mild-to-moderate food allergic reactions, the patient should be closely monitored for any signs or symptoms of an anaphylactic reaction.
Anaphylaxis may be fatal if not recognised and managed appropriately with rapid treatment. The drug of choice for the treatment of an anaphylactic reaction is intramuscular adrenaline, with other drugs given as adjuctive therapy.[3,4] In cases of suboptimal response to the initial dose of adrenaline, or with progression of symptoms, a repeat dose should be given.[5] Basic cardiopulmonary resuscitation should be initiated and maintained to support the airway, oxygenation and circulation. The following steps should be instituted in the initial management of anaphylaxis:
- eliminate additional exposure to the allergen
- administer intramuscular injection(s) of adrenaline
- call for help
- place the patient in a recumbent position, with lower limbs elevated, and do not allow the patient to stand up quickly
- give supplemental oxygen
- administer intravenous fluid in cases of hypotension or incomplete response to intramuscular adrenaline
- administer adjunctive therapy (antihistamines and corticosteroids)
- admit the patient for close observation for biphasic reactions
- instigate or review risk-reduction strategies after an anaphylactic episode.
Adrenaline is the drug of choice as first-line management of anaphylaxis. There are no absolute contraindications to treatment with adrenaline.[4,6] It should be administered intramuscularly (not subcutaneously) at a dose of 0.01 mg.kg-1 (0.01 mL/kg of 'neat' adrenaline; maximum 0.5 mL) in the mid-anterolateral thigh to achieve peak tissue and plasma concentrations rapidly.[1]
Adrenaline auto-injectors (e.g. EpiPen) are more convenient options than ampoules and syringes, which may be difficult to use quickly or accurately - especially by parents or patients in emergency situations. EpiPen injectors are available containing fixed doses of 0.15 mg and 0.30 mg adrenaline.[7]
H1 antihistamines may be used to decrease skin symptoms (itch, flush and urticaria) and nasal symptoms (rhinorrhoea and congestion) and are therefore beneficial in children and adults with non-life-threatening manifestations of food allergy. H1 antihistamines cannot prevent or treat life-threatening manifestations of anaphylaxis.[8] They are, however, used as adjunctive therapy to adrenaline. Less-sedating oral second-generation antihistamines are preferred to sedating firstgeneration antihistamines.[9] Intravenous antihistamines should be used if oral medication is not tolerated or contraindicated.
Corticosteroids are often used in anaphylaxis, but they have a delayed mechanism of action and are not useful during an acute episode. However, their anti-inflammatory properties may make them suitable as adjunctive therapy to reduce the risk of biphasic reactions.[1,5]
The initial pharmacological management of anaphylaxis is given in Table 1.

Co-factors for reactions
A number ofco-factors may augment or amplify the severity of allergic reactions.[12] Given their importance in eliciting anaphylaxis, these co-factors need to be included in diagnostic measures and management. They include the following:
- Physical exercise. Food-dependent exercise-induced anaphylaxis may occur if exercise and consumption of a certain food occur within 4 hours of each other. The implicated food is usually well tolerated when the patient does not exercise.
- Medication includes non-steroidal anti-inflammatory drugs, such as aspirin, ibuprofen and opiates.[13]
- Alcohol.[14]
- Fever and infectious diseases.[15]
- High-pollen season. In oral allergy syndrome, symptoms may be heightened during pollen season.
Although an anaphylactic reaction seems to be triggered by a sole allergen in most cases, exposure to a single allergen is sometimes not enough to trigger an episode. Concomitant exposure to a combination of allergens, infections, physical exercise, psychological stress, alcohol and/or concomitant medication are necessary to provoke a reaction, i.e. summation anaphylaxis.
Risk factors associated with the severity of allergic reactions to foods
The severity of allergic reactions to food allergens is multifactorial and variable. The severity of any reaction cannot be accurately predicted by the degree of the severity of any previous reaction, or by the size of the wheal of a skin-prick test or level of specific IgE.
Factors associated with increased risk, as shown in epidemiological studies,[16-24] include co-existing asthma (and poor asthma control), previous severe reactions, delayed administration of adrenaline, adolescents and young adults, reaction to trace amounts of foods, use of non-selective ß-blockers and patients in remote areas far from medical care. Self-injectable adrenaline is under-used, even when available, and incorrect administration may also be an important factor, particularly when administered by needle and syringe rather than by an auto-injector.[4]
Risk reduction[25]
The following factors should be considered in reducing the risk of an allergic reaction:
- Education with regard to food allergy and provision of a written emergency treatment plan on allergen avoidance, early symptom recognition and appropriate emergency treatment.
- Risk assessment and stratification with provision of injectable adrenaline (preferably via an auto-injector) if necessary. Training and provision of written instructions with regard to the indications for and method of administration of adrenaline.
- Follow-up with a primary care physician. Primary caregivers, nurses and doctors should be adequately trained and receive education to identify and treat allergic reactions to food early.
- Referral to an allergist if first presentation or unknown cause. More complicated food allergic patients should be referred to medical professionals competent in the diagnosis and management of food allergy.
- Management of patients with severe, complex or multiple food allergies by a multidisciplinary team, including dieticians and medical professionals.
- Early allergy testing in patients with food allergy symptoms. Interpretation of food allergy tests by a practitioner skilled in food allergy and with access to food challenge testing for cases of inconclusive results.
- Patients and caregivers should be educated about foods that should be avoided and available alternatives.
- Patients should be instructed to read labels. Clear guidelines should be set for labelling foodstuffs, including products that should be clearly linked to the name of an allergen to avoid confusion.
- Permission should be obtained to communicate the diagnosis of food allergy to all relevant caregivers, including schoolteachers. The patient must always wear a MedicAlert necklace or bracelet.
- Patients should be encouraged to join an appropriate patient support organisation.
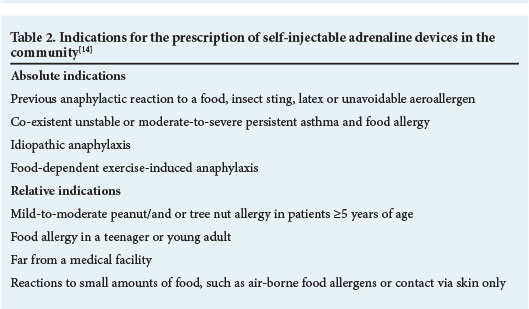
Indications for the prescription of self-injectable adrenaline devices in the community are given in Table 2.
Food allergy education
Strict avoidance of allergens
- Strict avoidance of allergens is the cornerstone of allergy management, although it is not curative and leaves patients at risk for accidental exposure.
- Only foods to which the patient is allergic should be avoided.
- Patients should receive education about label reading and medical terminology related to the identification of allergens.
- Patients should receive instruction with regard to cross-reactive allergens.
- It is advisable to involve a dietician in formulating a nutritionally adequate, allergen-free diet, especially in cases of multiple food allergy.
- Information on how to minimise cross-contact of foods with an allergen during meal preparation and serving can help to prevent accidental ingestion and reactions.
- Education on high-risk accidental ingestion, especially of foods prepared away from home (e.g. eating out, visiting friends' homes, or attending parties).
Early recognition of allergic reactions and anaphylaxis
- A written emergency plan should be given to the patient; their caregivers should be notified about the food allergy and given a copy of the plan. Plans are available at http://www.allergysa.org.
- The emergency plan should contain an image clearly differentiating between mild reactions and reactions requiring the use of adrenaline.
- Antihistamines are used for the management of non-severe allergic reactions.
- When only antihistamines are used for the treatment of acute allergic reactions, patients should be monitored should they develop more severe symptoms.
- As soon as a patient has an anaphylactic reaction, they should be placed in the supine position with lower extremities elevated; they should not stand up and move as this has been reported to increase the risk of severe anaphylaxis or sudden death.
- Adrenaline should be administered for all reactions that exceed the threshold in the action plan. If the patient or caregiver is considering using adrenaline, it is usually safer to give it immediately rather than to wait until definitive signs or symptoms appear.
- A MedicAlert bracelet or necklace should be provided to all patients at risk of anaphylaxis.
Provision of an emergency kit, including self-injectable adrenaline and intravenous antihistamine
- Adrenaline is the mainstay of treating anaphylaxis.
- Giving adrenaline via an auto-injector is preferable to administering it via a needle and syringe.
Provision of instructions on when to go to a medical facility
- Patients should be informed when to go to a medical facility if they are experiencing symptoms of an anaphylactic reaction.
- For patients with a history of severe allergic reactions, adrenaline should be administered at the onset of mild symptoms; then they should proceed to an emergency facility.
- Patients experiencing an anaphylactic episode should be observed in a medical facility for at least 12 - 24 hours because of the risk of biphasic reactions.
Educate patients about long-term ongoing management
- Long-term management must include at least an annual medical review to assess accidental ingestion, reactions, or both, nutritional adequacy of their diet, approaches to allergen avoidance and need for retesting for resolution of food allergy.
- At each visit, risk assessment for asthma, re-education about early recognition and emergency treatment plans should be reviewed.
References
1. Burks AW, Tang M, Sicherer S, et al. ICON: Food allergy. J Allergy Clin Immunol 2012;129(4):906-920. [http://dx.doi.org/10.1016/j.jaci.2012.02.001] [ Links ]
2. Longo G, Berti I, Burks AW, Krauss B, Barbi E. IgE-mediated food allergy in children. Lancet 2013;382(9905):1656-1664. [http://dx.doi.org/10.1016/S0140-6736(13)60309-8] [ Links ]
3. Muraro A, Roberts G, Clark A, et al. The management of anaphylaxis in childhood: Position paper of the European Academy of Allergology and Clinical Immunology. Allergy 2007;62:857-871. [http://dx.doi.org/10.1111/j.1398-9995.2007.01421.x] [ Links ]
4. Levin ME. Adrenaline for anaphylaxis: What is the evidence? Current Allergy & Clinical Immunology 2012;25(3):117-122. [ Links ]
5. Boyce JA, Assa'ad A, Burks AW, et al. Guidelines for the diagnosis and management of food allergy in the United States. J Allergy Clin Immunol 2010;126(suppl):S1-S58. [http://dx.doi.org/10.1016/j.jaci.2010.10.008] [ Links ]
6. Leung DYM, Sampson HA, Geha R, Szefler SJ. Pediatric Allergy: Principles and Practice. Philadelphia: Elsevier Saunders, 2010. [ Links ]
7. Green RJ, Motala C, Potter PC. ALLSA Handbook of Practical Allergy. 3rd ed. Cape Town: Allergy Society of South Africa, 2010. [http://dx.doi.org/10.1016/B0-12-227055-X/00509-5] [ Links ]
8. Cianferoni A, Muraro A. Food-induced anaphylaxis. Immunol Allergy Clin North Am 2012;32(1):165-195. [http://dx.doi.org/10.1016/j.iac.2011.10.002] [ Links ]
9. Park JH, Godbold JH, Chung D, Sampson HA, Wang J. Comparison of cetirizine and diphenhydramine in the treatment of acute food-induced allergic reactions. J Allergy Clin Immunol 2011;128(5):1127-1128. [http://dx.doi.org/10.1016/j.jaci.2011.08.026] [ Links ]
10. Sicherer SH, Simons FE; American Academy of Pediatrics. Self-injectable epinephrine for first-aid management of anaphylaxis. Pediatrics 2007;119(3):638-646. [http://dx.doi.org/10.1542/peds.2006-3689] [ Links ]
11. Simons FE, Gu X, Silver NA, Simons KJ. EpiPen Jr versus EpiPen in young children weighing 15 to 30 kg at risk for anaphylaxis. J Allergy Clin Immunol 2002;109(1):171-175. [http://dx.doi.org/10.1067/mai.2002.120758] [ Links ]
12. Wolbing F, Fischer J, Kaesler S. About the role and underlying mechanism of cofactors in anaphylaxis. Allergy 2013;68(9):1085-1092. [http://dx.doi.org/10.1111/all.12193] [ Links ]
13. Wolbing F, Biedermann T. Augmentation to anaphylaxis: The role of aspirin and physical exercise as co-factors. Acta Derm Venereol 2012;92:451-454. [http://dx.doi.org/10.1111/all12193] [ Links ]
14. European Academy of Allergy and Clinical Immunology (EAACI). EAACI Food Allergy and Anaphylaxis Guidelines: Diagnosis and management of food allergy. http://www.eaaci.org/resources/food-allergy-and-anapyhlaxis-guidelines.html (accessed 17 November 2014). [ Links ]
15. Mazur N, Patterson R, Perlman D. A case of idiopathic anaphylaxis associated with respiratory infections. Ann Allergy Asthma Immunol 1997;79:546-548. [http://dx.doi.org/10.1016/S1081-1206(10)63064-5] [ Links ]
16. Pumphrey RS. Lessons for management of anaphylaxis from a study of fatal reactions. Clin Exp Allergy 2000;30(8):1144-1150. [ Links ]
17. Pumphrey RS, Gowland MH. Further fatal allergic reactions to food in the United Kingdom, 1999-2006. J Allergy Clin Immunol 2007;119(4):1018-1019. [http://dx.doi.org/10.1046/j.1365-2222.2000.00864.x] [ Links ]
18. Colver AF, Nevantaus H, Macdougall CF, Cant AJ. Severe food-allergic reactions in children across the UK and Ireland, 1998-2000. Acta Paediatr 2005;94(6):689-695. [http://dx.doi.org/10.1080/08035250510031566] [ Links ]
19. Uguz A, Lack G, Pumphrey R, et al. Allergic reactions in the community: A questionnaire survey of members of the anaphylaxis campaign. Clin Exp Allergy 2005;35(6):746-750. [http://dx.doi.org/10.1111/j.1365-2222.2005.02257.x] [ Links ]
20. Bock SA, Muñoz-Furlong A, Sampson HA. Fatalities due to anaphylactic reactions to foods. J Allergy Clin Immunol 2001;107(1):191-193. [http://dx.doi.org/10.1067/mai.2001.112031] [ Links ]
21. Bock SA, Muñoz-Furlong A, Sampson HA. Further fatalities caused by anaphylactic reactions to food, 2001-2006. J Allergy Clin Immunol 2007;119(4):1016-1018. [http://dx.doi.org/10.1016/j.jaci.2006.12.622] [ Links ]
22. Sampson HA, Mendelson L, Rosen JP. Fatal and near-fatal anaphylactic reactions to food in children and adolescents. N Engl J Med 1992;327(6):380-384. [http://dx.doi.org/10.1056/NEJM199208063270603] [ Links ]
23. Gold MS, Sainsbury R. First aid anaphylaxis management in children who were prescribed an epinephrine autoinjector device (EpiPen). J Allergy Clin Immunol 2000;106:171-176. [http://dx.doi.org/10.1067/mai.2000.106041] [ Links ]
24. Liew WK, Williamson E, Tang ML. Anaphylaxis fatalities and admissions in Australia. J Allergy Clin Immunol 2009;123(2):434-442. [http://dx.doi.org/10.1016/j.jaci.2008.10.049] [ Links ]
25. Levin ME. How to prevent and treat an allergic crisis. Continuing Medical Education 2013;31(1):8-10. [ Links ]
 Correspondence:
Correspondence:
M Levin
michael.levin@uct.ac.za














