Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.105 no.1 Pretoria Jan. 2015
http://dx.doi.org/10.7196/SAMJ.9103
CONTINUING MEDICAL EDUCATION
ARTICLE
Epidemiology of IgE-mediated food allergy
C L Gray; E Goddard; S Karabus; M Kriel; A C Lang; A I Manjra; S M Risenga; A J Terblanche; D A van der Spuy; M E Levin; for the South African Food Allergy Working Group (SAFAWG)
All authors' degrees, affiliations and conflict of interest statements can be found online at http://dx.doi.org/10.7196/SAMJ.9201
ABSTRACT
Despite the large number of foods that may cause immunoglobulin E (IgE)-mediated reactions, most prevalence studies have focused on the most common allergenic foods, i.e. cow's milk, hen's egg, peanut, tree nut, wheat, soya, fish and shellfish. Food allergy peaks during the first two years of life, and then diminishes towards late childhood as tolerance to several foods develops. Based on meta-analyses and large population-based studies, the true prevalence of food allergy varies from 1% to >10%, depending on the geographical area and age of the patient. The prevalence of food allergy in South Africa (SA) is currently being studied. The prevalence of IgE-mediated food allergy in SA children with moderate-to-severe atopic dermatitis is 40%; however, this represents a high-risk population for food allergy. Preliminary data from the South African Food Sensitisation and Food Allergy (SAFFA) study, which is investigating food allergy in an unselected cohort of 1 - 3-year olds, show a prevalence of 11.6% sensitisation to common foods. Food allergy was most common to egg (1.4%) and peanut (1.1%). Food allergy appears to be the most common trigger of anaphylactic reactions in the community, especially in children, in whom food is responsible for >85% of such reactions. In adults, shellfish and nut, and in children, peanut, tree nut, milk and egg, are the most common triggers of food-induced anaphylaxis.
True food allergy is less prevalent than commonly perceived. Up to 34% of individuals or parents think that they or a family member has a food allergy and 22% avoid particular foods because the food may possibly contain an allergen. However, only 1 - 6% of persons test positive on full evaluation, which may include double-blind placebo-controlled food challenges.[1-4]
Epidemiology of IgE-mediated food allergy
The prevalence of food allergy varies significantly based on geographical region, allergens tested, diagnostic criteria, population age and concurrent atopic conditions.[5] Variations in food allergy definitions and inconsistencies in study design make studies on food allergy prevalence difficult to compare. Self-reporting significantly overestimates food allergy prevalence up to 10-fold;[4] hence, objective measurements are necessary to establish a true food allergy diagnosis. Similarly, sensitisation to foods is much higher than clinically relevant allergies; therefore, sensitisation should always be combined with more objective information to prove allergies. Food challenge testing is the optimal way of proving food allergy, albeit labour and cost intensive. Recent large population-based studies, such as the EuroPrevall study in Europe[6] and HealthNuts study in Australia,[7] have used food challenge testing and can be considered flagship studies of food allergy prevalence.
Prevalence of food allergy
Despite the large number of foods that can cause immunoglobulin E (IgE)-mediated reactions, most prevalence studies have focused on the most common allergenic foods, i.e. cow's milk, hen's egg, peanut, tree nut, wheat, soya, fish and shellfish.'81
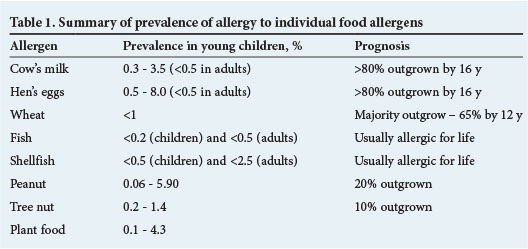
Food allergy peaks during the first two years of life, and then diminishes towards late childhood as tolerance to several foods develops over time. Based on meta-analyses and large population-based studies, the true prevalence of food allergy varies from 1% to >10%, depending on the geographical area and age of the patient.[9-19] Allergy prevalence to the most common allergenic foods is summarised in Table 1.
The prevalence of food allergy in South Africa (SA) is currently being studied. An unselected population of 211 Xhosa high-school students showed an overall sensitisation to foods of 5%.[20,21] Preliminary data from the South African Food Sensitisation and Food Allergy (SAFFA) study,[22] which is investigating food allergy in an unselected cohort of 1 - 3-year-olds, show a prevalence of skin-prick tests of >1 mm (11.6%), >3 mm (9.9%) and >7 mm (4.2%) to all foods tested. Challenge-proven food allergy to any food is 1.8% after the preliminary analysis; recruitment is ongoing.
Increase in food allergy
Many studies have suggested a true rise in the prevalence of true food allergies over the past 10 - 20 years,[23-25] but further confirmation is required. This probable increase in food allergy requires urgent further investigation as it may be due to modifiable environmental factors.[26,27] Not only genetic factors, but also several environmental factors, have been proposed as influencing the risk for food allergy,[28] such as timing of allergen exposure, microbial exposure, and dietary antioxidant consumption.[29-31]
Allergies to specific foods
Cow's milk
Cow's milk protein allergy (CMPA) peaks in the first year of life. Based on several studies, its documented prevalence is 0.3 - 3.5% in young children (<5 years of age),[22,32-36] <1% in older children, and <0.5% in adults.[22,37,38]
Studies have indicated a generally good prognosis for CMPA, with 45 - 56% outgrowing the allergy by the age of 1 year, 60 - 76% by age 2, 85 - 90% by age 3, and 97% by age 15.[38,39]Acquisition of tolerance is faster in those with:
- initial specific IgE <2 kU/L
- delayed v. IgE-mediated reactions
- absence of asthma or allergic rhinitis.[40,41]
Egg allergy is more prevalent in children than in adults, and is usually IgE mediated. The estimated prevalence is 0.5 - 5.0% in early childhood,'42,431 decreasing significantly to <0.5% in older children and adults.[43,44] The prevalence of egg allergy in the preliminary data on 1 - 3-year-old SA children is 1.4%.[22]
Previous studies have demonstrated a good prognosis for egg allergy, with around 50% of egg allergic children outgrowing the condition by the age of 3 years, and 66% by the age of 5 years.[44,45]
Factors associated with persistence of egg allergy include:
- high initial egg specific IgE
- multiple food allergies
- multiple atopic conditions
- ovomucoid sensitivity
- slow decrease in specific IgE to egg white over time.[45]
Wheat
Wheat allergy is self-reported in about 4.5% of the population,[46] but confirmed in <1%.[42,43,46,47] It can manifest in both IgE-mediated and non-IgE-mediated symptoms. The natural history of wheat allergy is less well studied, but the majority of patients tend to become tolerant by adolescence.[47] A study from the USA showed the development of tolerance in 29% by 4 years, 56% by 8 years, and 65% by 12 years.[48]
Fish and shellfish
Fish allergy is one of the few allergies that may be more common in adults than in children. A wide variety of fish and shellfish species have been implicated, depending on availability and consumption patterns. Large USA-based studies have shown a prevalence of fish allergy in <0.2% of children and <0.5% of adults,[49,50] and shellfish allergy in <0.5% of children and <2.5% of adults.[49,50] Seafood allergy is lifelong in the majority of cases.
Peanut
The prevalence of peanut allergy varies significantly between geographical regions: in the EuroPrevall study, the overall prevalence of peanut allergy was 2.6%,[51,52] with wide variation between countries from 0.06% to 5.9%.[53] Prevalence of peanut allergy is about 0.8% in the population in the USA.[54] In an SA study of Xhosa high-school students, 1.9% were sensitised to peanut but none reported allergic symptoms.'551 Experience from our food allergy clinics in SA, and figures on peanut allergy in eczema patients, suggests that peanut allergy in SA may now be higher than previously anticipated.[56] The prevalence of peanut allergy in the preliminary data on 1 - 3-year-old SA children is 1.1%.[22]
Peanut allergy usually starts in early childhood and only a small proportion (20%) of patients outgrow it.[57,58] Negative skin-prick tests or a low level of peanut specific IgE makes outgrowing the allergy more likely.
The prevalence of tree nut allergy in the USA is approximately 0.5%.[54] The prevalence among European children in the EuroPrevall study varied from 0.2% to 1.4%.[59,60] The prevalence may be higher in adolescents and adults, as allergy to tree nuts may occur for the first time in adult life.
Allergy to tree nuts is outgrown in only about 10% of children, predominantly in those with low specific IgE <5 kU/L.[61]
Plant food
Allergic symptoms to various fruits and vegetables may be true allergies or caused by cross-reactivity (pollen fruit syndrome). In a recent systemic review (EuroPrevall study), the prevalence of perceived allergy to any fruits varied between 0.4% and 11.5%, and challenge-proven food allergy to fruits was 0.1 - 4.3%.[62]
Food-related anaphylaxis and fatalities
Food allergy appears to be the most common trigger of anaphylaxis in the community. One-third to half of anaphylactic episodes can be attributed to food;[63,64] this proportion seems to be higher in children, in whom food is responsible for >85% of anaphylactic reactions.[65] In adults, shellfish and nut are the most common triggers of food-induced anaphylaxis, and in children, peanut, tree nut, milk and egg.[66] The prevalence of food-induced anaphylaxis is difficult to estimate owing to methodological differences in acquiring data; however, there is evidence that food-induced anaphylaxis is increasing.[67]
Food allergy and comorbid conditions
Food allergic patients are significantly more likely than non-allergic patients to have concomitant atopic conditions. In patients with food allergy, studies have shown that:'681
- 35 - 71% have evidence of atopic dermatitis
- 33 - 40% have evidence of allergic rhinitis
- 34 - 49% have evidence of asthma.
The prevalence of IgE-mediated food allergy in patients with moderate-to-severe atopic dermatitis is 30 - 40%, based on studies in Europe, the USA,[69-72] and, more recently, SA.[56]
References
1. Sloan AE, Powers ME. A perspective on popular perceptions of adverse reactions to foods. J Allergy Clin Immunol 1986;78:127-133. [http://dx.doi.org/10.1016/0091-6749(86)90002-3] [ Links ]
2. Venter C, Pereira B, Grundy J, Clayton CB, Arshad SH, Dean T. Prevalence of sensitization reported and objectively assessed food hypersensitivity amongst six-year-old children: A population-based study. Pediatr Allergy Immunol 2006;17(5):356-363. [http://dx.doi.org/10.1111/j.1399-3038.2006.00428.x] [ Links ]
3. Venter C, Pereira B, Voigt K, et al. Prevalence and cumulative incidence of food hypersensitivity in the first 3 years of life. Allergy 2008;63(3):354-359. [http://dx.doi.org/10.1111/j.1398-9995.2007.01570.x] [ Links ]
4. Bock S. Prospective appraisal of complaints of adverse reactions to foods in children during the first 3 years of life. Pediatrics 1987;79:683-688. [ Links ]
5. Sicherer S. Epidemiology of food allergy. J Allergy Clin Immunol 2011;127:594-602. [http://dx.doi.org/10.1016/j.jaci.2010.11.044] [ Links ]
6. Rona RJ, Keil T, Summers C, et al. The prevalence of food allergy: A meta-analysis. J Allergy Clin Immunol 2007;120:638-646. [http://dx.doi.org/10.1016/j.jaci.2007.05.026] [ Links ]
7. Osborne NJ, Koplin JJ, Martin PE, et al. Prevalence of challenge-proven IgE-mediated food allergy using population-based sampling and predetermined challenge criteria in infants. J Allergy Clin Immunol 2011;127:668-676. [http://dx.doi.org/10.1016/j.jaci.2011.01.039] [ Links ]
8. Gray C, du Toit G. Food allergy. In: Green RJ, Motala C, Potter PC, eds. ALLSA Handbook of Practical Allergy. 3rd ed Cape Town: Allergy Society of South Africa, 2010:64-101. [http://dx.doi.org/10.1016/B0-12-227055-X/00509-5] [ Links ]
9. EAACI Food Allergy and Anaphylaxis Guidelines: Diagnosis and management of food allergy. http://www.eaaci.org/resources/food-allergy-and-anapyhlaxis-guidelines.html (accessed 11 November 2014). [ Links ]
10. Schnabel E, Sausenthaler S, Schaaf B, et al. Prospective association between food sensitization and food allergy: Results of the LISA birth cohort study. Clin Exp Allergy 2010;40:450-457. [http://dx.doi.org/10.1111/j.1365-2222.2009.03400.x] [ Links ]
11. Liu HA, Jaramillo R, Sicherer SH, et al. National prevalence and risk factors for food allergy and relationship to asthma: Results from the National Health and Nutrition Examination Survey 20052006. J Allergy Clin Immunol 2010;126:798-806. [http://dx.doi.org/10.1016/j.jaci.2010.07.026] [ Links ]
12. Branum AM, Lukas SL. Food allergy among children in the United States. Pediatrics 2009;124:1549-1555. http://dx.doi.org/10.1542/peds.2009-1210] [ Links ]
13. Venter C, Pereira B, Voigt K, et al. Prevalence and cumulative incidence of food hypersensitivity in the first 3 years of life. Allergy 2008;63:354-359. [http://dx.doi.org/10.1111/j.1398-9995.2007.01570.x] [ Links ]
14. Eller E, Kjaer HF, Host A, et al. Food allergy and food sensitization in early childhood: Results from the DARC cohort. Allergy 2009;64:1023-1029. [http://dx.doi.org/10.1111/j.1398-9995.2009.01952.x] [ Links ]
15. Osterballe M, Mortz CG, Hansen TK, et al. The prevalence of food hypersensitivity in young adults. Pediatr Allergy Immunol 2009;20:686-692. [http://dx.doi.org/10.1111/j.1399-3038.2008.00842.x] [ Links ]
16. Chen J, Hu Y, Allen KJ, Ho MH, Li H. The prevalence of food allergy in infants in Chongqing, China. Pediatr Allergy Immunol 2011;22(4):356-360. [http://dx.doi.org/10.1111/j.1399-3038.2011.01139.x] [ Links ]
17. Chen J, Liao Y, Zhang HZ, Zhao H, Chen J, Li HQ. [Prevalence of food allergy in children under 2 years of age in three cities in China] [Article in Chinese] Zhonghua Er Ke Za Zhi 2012;50(1):5-9. [ Links ]
18. Santadusit S, Atthapaisalsarudee S, Vichyanond P. Prevalence of adverse food reactions and food allergy among Thai children. J Med Assoc Thai 2005;88(Suppl 8):S27-32. [ Links ]
19. Dalal I, Binson I, Reifen R, et al Food allergy is a matter of geography after all: Sesame as a major cause of severe IgE-mediated food allergic reactions among infants and young children in Israel. Allergy 2002;57:362-365. [http://dx.doi.org/10.1034/j.1398-9995.2002.1s3412.x] [ Links ]
20. Levin ME, Le Souëf PN, Motala C. Total IgE in urban Black South African teenagers: The influence of atopy and helminth infection. Pediatr Allergy Immunol 2008;19:449-454. [ahttp://dx.doi.org/10.1111/j.1399-3038.2007.00663.x. [ Links ]]
21. Levin ME, Muloiwa R, Motala C. Associations between asthma and bronchial hyperresponsiveness with allergy and atopy phenotypes in urban Black South African teenagers. S Afr Med J 2011;101:472-476. [ Links ]
22. Botha M, Basera W, Gray C, et al The prevalence of IgE mediated food sensitisation and food allergy in unselected 12-36 month old urban South African children. Current Allergy & Clinical Immunology 2014;3:230. [ Links ]
23. Rudders SA, Banerji A, Vassallo MF, et al. Trends in pediatric emergency department visits for food-induced anaphylaxis. J Allergy Clin Immunol 2010;126:385-388. [http://dx.doi.org/10.1016/j.jaci.2010.05.018] [ Links ]
24. Grundy J, Matthews S, Bateman B, et al. Rising prevalence of allergy to peanut in children: Data from two sequential cohorts. J Allergy Clin Immunol 2002;110:784-789. [http://dx.doi.org/10.1067/mai.2002.128802] [ Links ]
25. Venter C, Hasan AS, Grundy J, et al. Time trends in the prevalence of peanut allergy: Three cohorts of children from the same geographical location in the UK. Allergy 2010;65:103-108. [http://dx.doi.org/10.1111/j.1398-9995.2009.02176.x] [ Links ]
26. Prescott S, Allen KA. Food allergy: Riding the second wave of the allergy epidemic. Pediatr Allergy Immunol 2011;22:155-160. [http://dx.doi.org/10.1111/j.1399-3038.2011.01145.x] [ Links ]
27. Gray C, Kung S. Food allergy in South Africa: Joining the food allergy epidemic? Current Allergy & Clinical Immunology 2012;25:24-29. [ Links ]
28. Lack G. Epidemiologic risks for food allergy. J Allergy Clin Immunol 2008;121:1331-1336. [http://dx.doi.org/10.1016/j.jaci.2008.04.032] [ Links ]
29. Koplin JJ, Osborne NJ, Wake M, et al. Can early introduction of egg prevent egg allergy in infants? A population-based study. J Allergy Clin Immunol 2010;126:807-813. [http://dx.doi.org/10.1016/j.jaci.2010.07.028] [ Links ]
30. Snijders BE, Thijs C, van Ree R, van den Brandt PA. Age at first introduction of cow milk products and other food products in relation to infant atopic manifestations in the first 2 years of life: The KOALA Birth Cohort Study. Pediatrics 2008;122:e115-e122. [http://dx.doi.org/10.1542/peds.2007-1651] [ Links ]
31. Vassallo MF, Camargo CA. Potential mechanisms for the hypothesized link between sunshine, vitamin D, and food allergy in children. J Allergy Clin Immunol 2010;126:217-222. [http://dx.doi.org/10.1016/j.jaci.2010.06.011] [ Links ]
32. Hu Y, Chen J, Li H. Comparison of food allergy prevalence among Chinese infants in Chongqing, 2009 versus 1999. Pediatr Int 2010;52:820-82. [http://dx.doi.org/10.1111/j.1442-200X.2010.03166.x] [ Links ]
33. Sampson HA. Update on food allergy. J Allergy Clin Immunol 2004;113:805-819. [http://dx.doi.org/10.1016/j.jaci.2004.03.014] [ Links ]
34. Rance F, Grandmottet X, Grandjean H. Prevalence and main characteristics of schoolchildren diagnosed with food allergies in France. Clin Exp Allergy 2005;35:167-172. [http://dx.doi.org/10.1111/j.1365-2222.2005.02162.x] [ Links ]
35. Eggesbo M, Botten G, Halvorsen R, et al. The prevalence of CMA/CMPI in young children: The validity of parentally perceived reactions in a population-based study. Allergy 2001;56:393-402. [http://dx.doi.org/10.1034/j.1398-9995.2001.056005393.x] [ Links ]
36. Pereira B, Venter C, Grundy J, et al. Prevalence of sensitization to food allergens, reported adverse reaction to foods, food avoidance, and food hypersensitivity among teenagers. J Allergy Clin Immunol 2005;116:884-892. [http://dx.doi.org/10.1016/j.jaci.2005.05.047] [ Links ]
37. Osterballe M, Hansen TK, Mortz CG, et al. The prevalence of food hypersensitivity in an unselected population of children and adults. Pediatr Allergy Immunol 2005;16:567-573. [http://dx.doi.org/10.1111/j.1399-3038.2005.00251.x] [ Links ]
38. Host A, Jacobsen HP, Halken S, et al. The natural history of cow's milk protein allergy/intolerance. Eur J Clin Nutr 1995;49(Suppl 1):S13-S18. [ Links ]
39. Host A, Halken S. A prospective study of cow milk allergy in Danish infants during the first 3 years of life. Clinical course in relation to clinical and immunological type of hypersensitivity reaction. Allergy 1990;45:587-596. [http://dx.doi.org/10.1111/j.1398-9995.1990.tb00944.x] [ Links ]
40. Skripak JM, Matsui EE, Mudd K, et al The natural history of IgE-mediated cow's milk allergy. J Allergy Clin Immunol 2007;120:1172-1177. [http://dx.doi.org/10.1016/j.jaci.2007.08.023] [ Links ]
41. Vanto T, Helppila S, Juntunen-Backman K, et al. Prediction of the development of tolerance to milk in children with cow's milk hypersensitivity. J Pediatr 2004;144:218-222. [http://dx.doi.org/10.1016/j.jpeds.2003.10.063] [ Links ]
42. Hill DJ, Hosking CS, Zhie CY, et al. The frequency of food allergy in Australia and Asia. Environ Toxicol Pharmacol 1997;4:101-110. [http://dx.doi.org/10.1016/S1382-6689(97)10049-7] [ Links ]
43. Woods RK, Stoney RM, Raven J, et al. Reported adverse food reactions overestimate true food allergy in the community. Eur J Clin Nutr 2002;56:31-36. [http://dx.doi.org/10.1038/sj.ejcn.1601306] [ Links ]
44. Eggesbo M, Botten G, Halvorsen R, et al. The prevalence of allergy to egg: A population-based study in young children. Allergy 2001;56:403-411. [http://dx.doi.org/10.1034/j.1398-9995.2001.056005403.x] [ Links ]
45. Tey D, Heine RG. Egg allergy in childhood: An update. Curr Opin Allergy Clin Immunol 2009;9:244-250. [http://dx.doi.org/10.1097/ACI.0b013e32832b1f00] [ Links ]
46. Kember Associates. Results of a Consumer Survey into Attitudes towards Bread, Nutrition and Allergy/Intolerance. London: NABIM, 2009. [ Links ]
47. Kotaniemi-Syrjanen A, Palosuo K, Jartti T, et al. The prognosis of wheat hypersensitivity in children. Pediatr Allergy Immunol 2010;21:e421-e428. [http://dx.doi.org/10.1111/j.1399-3038.2009.00946.x] [ Links ]
48. Keet CA, Matsui EC, Dhillon G, et al. The natural history of wheat allergy. Ann Allergy Asthma Immunol 2009;102:410-415. [http://dx.doi.org/10.1016/j.jaci.2007.12.934] [ Links ]
49. Sicherer SH, Munoz-Furlong A, Sampson HA. Prevalence of seafood allergy in the United States determined by a random telephone survey. J Allergy Clin Immunol 2004;114:159-165. [http://dx.doi.org/10.1016/j.jaci.2004.04.018] [ Links ]
50. Ben-Shoshan M, Harrington DW, Soller L, et al. A population-based study on peanut, tree nut, fish, shellfish, and sesame allergy prevalence in Canada. J Allergy Clin Immunol 2010;125:1327-1335. [http://dx.doi.org/10.1016/j.jaci.2010.03.015] [ Links ]
51. Burney P, Summers C, Chinn S, et al. Prevalence and distribution of sensitization to foods in the European Community Respiratory Health Survey: A EuroPrevall analysis. Allergy 2010;65:1182-1188. [http://dx.doi.org/10.1111/j.1398-9995.2010.02346.x] [ Links ]
52. Venter C, Arshad SH. Epidemiology of food allergy. Pediatr Clin N Am 2011;58: 327-349. [http://dx.doi.org/10.1016/j.pcl.2011.02.011] [ Links ]
53. Marklund B, Ahlstedt S, Nordstrom G, et al. Health-related quality of life among adolescents with allergy-like conditions - with emphasis on food hypersensitivity. Health Qual Life Outcomes 2004;2:65. [ Links ]
54. Sicherer SH, Munoz-Furlong A, Godbold JH, et al. US prevalence of self-reported peanut, tree nut, and sesame allergy: 11-year follow-up. J Allergy Clin Immunol 2010;125:1322-1326. [http://dx.doi.org/10.1016/j.jaci.2010.03.029] [ Links ]
55. Du Toit G, Levin M, Motala C, et al. Peanut allergy and peanut-specific IgG4 characteristics among Xhosa children in Cape Town. J Allergy Clin Immunol 2007;119(1):S196. [http://dx.doi.org/10.1016/j.jaci.2006.12.136] [ Links ]
56. Gray CL, Levin ME, Zar HJ, et al. Food allergy in South African children with atopic dermatitis. Paediatr Allergy Immunol 2014;25:572-579. [http://dx.doi.org/10.1111/pai.12270] [ Links ]
57. Savage JH, Limb SL, Brereton NH, et al. The natural history of peanut allergy: Extending our knowledge beyond childhood. J Allergy Clin Immunol 2007;120:717-719. [http://dx.doi.org/10.1016/j.jaci.2007.07.027] [ Links ]
58. Fleischer DM. The natural history of peanut and tree nut allergy. Curr Allergy Asthma Rep 2007;7:175-181. [http://dx.doi.org/10.1007/s11882-007-0018-y] [ Links ]
59. Venter C, Pereira B, Grundy J, et al. Incidence of parentally reported and clinically diagnosed food hypersensitivity in the first year of life. J Allergy Clin Immunol 2006;117:1118-1124. [http://dx.doi.org/10.1016/j.jaci.2005.12.1352] [ Links ]
60. Penard-Morand C, Raherison C, Kopferschmitt C, et al. Prevalence of food allergy and its relationship to asthma and allergic rhinitis in schoolchildren. Allergy 2005;60:1165-1171. [http://dx.doi.org/10.1111/j.1398-9995.2005.00860.x] [ Links ]
61. Fleischer DM, Conover-Walker MK, Matsui EC, et al. The natural history of tree nut allergy. J Allergy Clin Immunol 2005;116:1087-1093. [http://dx.doi.org/10.1016/j.jaci.2004.12.980] [ Links ]
62. Zuidmeer L, Goldhahn K, Rona RJ, et al. The prevalence of plant food allergies: A systematic review. J Allergy Clin Immunol 2008;121:1210-1218. [http://dx.doi.org/10.1016/j.jaci.2008.02.019] [ Links ]
63. Simons FE, Sampson HA. Anaphylaxis epidemic: Fact or fiction? J Allergy Clin Immunol 2008;122:1166-1168. [http://dx.doi.org/10.1016/j.jaci.2008.10.019] [ Links ]
64. Decker WW, Campbell RL, Manivannan V, et al. The etiology and incidence of anaphylaxis in Rochester, Minnesota: A report from the Rochester Epidemiology Project. J Allergy Clin Immunol 2008;122:1161-1165. [http://dx.doi.org/10.1016/j.jaci.2008.09.043] [ Links ]
65. De Silva IL, Mehr SS, Tey D, Tang ML. Paediatric anaphylaxis: A 5 year retrospective review. Allergy 2008;63:1071-1076. [http://dx.doi.org/10.1111/j.1398-9995.2008.01719.x] [ Links ]
66. Ross MP, Ferguson M, Street D, Klontz K, Schroeder T, Luccioli S. Analysis of food-allergic and anaphylactic events in the National Electronic Injury Surveillance System. J Allergy Clin Immunol 2008;121:166-171. [http://dx.doi.org/10.1016/j.jaci.2007.10.012] [ Links ]
67. Liew WK, Williamson E, Tang ML. Anaphylaxis fatalities and admissions in Australia. J Allergy Clin Immunol 2009;123:434-442. [http://dx.doi.org/10.1016/j.jaci.2008.10.049] [ Links ]
68. Branum AM, Lukacs SL. Food allergy among children in the United States. Pediatrics 2009;124:1549-1555. [http://dx.doi.org/10.1542/peds.2009-1210] [ Links ]
69. Gray C. Allergies in eczema. Current Allergy & Clinical Immunology 2011;24(3):185-191. [ Links ]
70. Burks AW, James JM, Hiegel A, et al. Atopic dermatitis and food hypersensitivity reactions. J Pediatr 1998;132(1):132-136. [http://dx.doi.org/10.1016/S0022-3476(98)70498-6] [ Links ]
71. Eigenmann PA, Sicherer SH, Borkowski TA, et al. Prevalence of IgE-mediated food allergy among children with atopic dermatitis. Pediatrics 1998;101(3):e8. [http://dx.doi.org/10.1542/peds.101.3.e8] [ Links ]
72. Eigenmann PA, Calza A-M. Diagnosis of IgE-mediated food allergy among Swiss children with atopic dermatitis. Pediatr Allergy Immunol 2000;11:95-100. [http://dx.doi.org/10.1034/j.1399-3038.2000.00071.x] [ Links ]
 Correspondence:
Correspondence:
C Gray
claudiagray.paediatrics@gmail.com














