Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.104 no.12 Pretoria Dez. 2014
http://dx.doi.org/10.7196/SAMJ.9110
CONTINUING MEDICAL EDUCATION
ARTICLE
Focus on adolescents with HIV and AIDS
L FairlieI; N SipamboII; C FickIII; H MoultrieIV
IMB ChB, DCH (UK), FCPaed (SA), MMed; Wits Reproductive Health and HIV Institute (WRHI), University of the Witwatersrand, Johannesburg, South Africa
IIMB BCh, FCPaed (SA); Wits Reproductive Health and HIV Institute (WRHI), University of the Witwatersrand, Johannesburg, South Africa; Department of Paediatrics, Chris Hani Baragwanath Hospital, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIIMB BCh, Dip HIV Man; Wits Reproductive Health and HIV Institute (WRHI), University of the Witwatersrand, Johannesburg, South Africa
IVMB BCh, MSc;Wits Reproductive Health and HIV Institute (WRHI), University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
Adolescents living with HIV, including those infected perinatally and non-perinatally, bear a disproportionate burden of the HIV epidemic in South Africa. This article discusses HIV management in adolescents including the following aspects: (i) burden of HIV disease, modes of HIV acquisition and implications for management; (ii) initiation of combination antiretroviral therapy (ART), outcomes and complications of ART in adolescents, including virological failure and switching regimens; (iii) adherence in adolescence, including factors that may contribute to poor adherence and advice to improve adherence; (iv) issues particular to adolescents, including sexual and reproductive health needs, disclosure to adolescents and by adolescents, and transition to adult care. This article aims to provide insights based on the literature and experience to assist the clinician to navigate the difficulties of managing HIV in adolescence and achieving successful transition to adult care.
Epidemiology
There are few routine data on the health of South African (SA) adolescents (defined by the World Health Organization (WHO) as aged 10 - 19 years), partly a result of the age bands used in the District Health Information System. This is cause for concern. Many of the determinants of adult ill health, such as harmful alcohol use, tobacco use, unhealthy diet, and lack of physical activity, have their origins in adolescence. Critically, female adolescents bear a disproportionate burden of the HIV epidemic in SA. In 2012, the estimated HIV prevalence (range) in 15 - 24-year-old SA women and men was 13.9% (12.9 -16.8%) and 3.9% (2.5 - 5.7%), respectively,[1] equating to ~720 000 adolescents and young people living with HIV.[2] The population of adolescents living with HIV in SA is comprised of adolescents with perinatal HIV infection (PHIV) who have moved into adolescence (PHIA) and those who acquired HIV at an older age through sexual activity, intravenous drug use or other less common modes of transmission (non-PHIV).
The prevention of mother-to-child-transmission programme (PMTCT) in SA has led to a massive reduction in perinatal HIV infections in the last decade. As a result, combined with high coverage and early initiation of combination antiretroviral therapy (ART) with concomitant reductions in morbidity and mortality, the SA population of children with perinatally acquired HIV is rapidly moving into adolescence, with adolescents possibly already forming the bulk of paediatric HIV patients.[3] Some PHIA will have been diagnosed with HIV and started on ART early in childhood, with some already on secondor third-line ART by the time they reach adolescence. Other PHIA who are diagnosed in late childhood or in early to mid-adolescence are often severely immunocompromised and urgently require ART at the time of diagnosis, though up to half may be asymptomatic.[4] These late presenters represent ongoing missed diagnostic opportunities, the result of numerous factors beyond the scope of this article, but which include poor record keeping contributing to subtle chronic symptoms not being appropriately identified or investigated by healthcare workers despite numerous clinic visits, and the lack of child- or youth-friendly services hampering accessibility.
The prevention and diagnosis of HIV infection acquired in adolescence continues to require urgent attention. Nearly a quarter (24%) of all new HIV infections in SA in 2012 occurred in 15 - 24-year-olds, with the incidence in women in this age group almost 4 times greater than that in men (2.5% v. 0.6%).[2] Adolescents living with HIV acquired during adolescence are likely to have early-stage disease, higher CD4+ counts, and fewer opportunistic infections, and are less likely to meet current criteria for initiation of ART than PHIA. An exception is pregnant adolescents, who would qualify for ART regardless of CD4+ count and time of infection. Measures to address HIV testing and access to care in children and adolescents are imperative.
Combination ART and monitoring
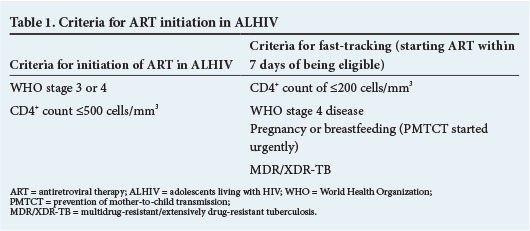
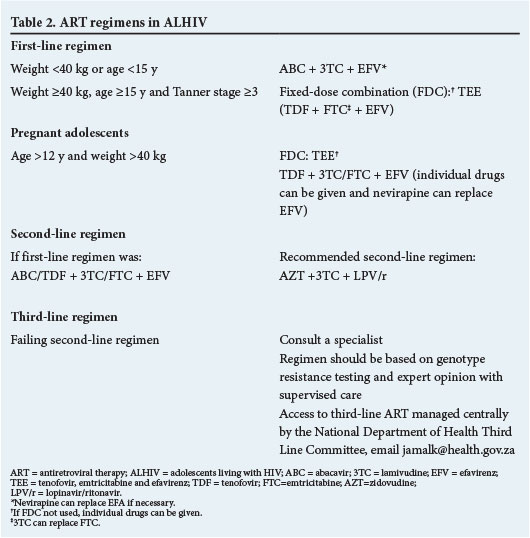
Table 1 tabulates the indications for ART initiation in adolescents. Table 2 describes first-, second- and third-line regimens currently used in adolescents.
Monitoring of clinical, immunological and virological indicators on ART for adolescents is the same as for children. In addition, given the high risks of poor adherence and virological failure in this group, 6-monthly viral load (VL) testing should be considered.
Outcomes on ART
Longitudinal cohorts, mainly from well-resourced settings, report good clinical health with weight, height and body mass index approximating population norms.[5] Reductions in mortality rates of up to 76% in PHIV children and adolescents receiving ART have been reported in well-resourced settings.[6] All-cause mortality rates are similar when adolescents (9-19 years) and young adults receiving ART (20 -29 years) are compared in reports from sub-Saharan Africa.[7,8] Immunologically, cohorts from resource-rich and resource-limited settings demonstrate robust CD4+ improvement on ART, sustained to at least 5 years of follow-up.[6,8] Adolescents, however, generally have lower virological suppression rates (HIV VL <400 copies/mL) on ART compared with adults. Suppression rates range between 27% and 78% in longitudinal cohorts with low rates in both PHIV and non-PHIV adolescents in sub-Saharan Africa.[8-10] Table 3 describes challenges with ART that are unique to adolescents.[11]
Adherence
Adolescence is a period of physical, sexual, emotional and psychological change associated with developing autonomy, increased impulsivity and risk taking, increased peer influence and potentially reduced parental oversight. Poor adherence in adolescence has been described in many chronic conditions including diabetes, asthma, cystic fibrosis and HIV. Poor adherence may be related to a number of factors including: simple lifestyle barriers such as forgetting or struggling to fit ART into a busy school and extramural schedule; medication-related factors such as complex twice-daily regimens with high pill burdens; drug-drug interactions, and side-effects; patient-related factors such as treatment fatigue, lack of disclosure to the adolescent and by the adolescent to others, fear of stigma, unresolved psychosocial problems or substance abuse; and socioeconomic constraints limiting access to the clinic.
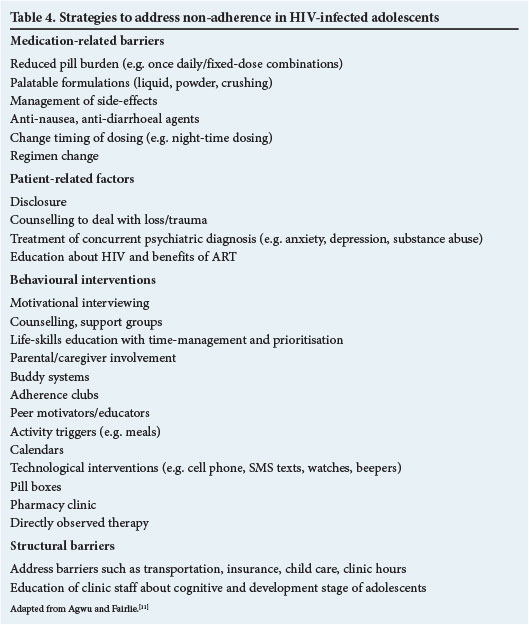
Since both adherence and barriers may change over time, it is necessary to assess adherence and modifiable barriers at each visit and, together with the adolescent, tailor interventions to support adherence (Table 4). At each visit the following adherence reinforcements are necessary: identify and resolve any confusion with the regimen; manage any emerging drug side-effects; enquire about changes in lifestyle and need for adjustments; and provide ongoing psychosocial counselling and management of new or unresolved issues. A multidisciplinary approach including social workers, nurse, mental health professionals and counsellors may be required where available.
Approach to an adolescent with virological failure
An elevated HIV VL is the most sensitive, though not necessarily specific, measure of non-adherence in HIV-infected patients as individuals with significant non-adherence will have detectable VLs. However, highly adherent individuals may have elevated VLs as a result of drug resistance, inappropriate regimens, drug interactions or incorrect doses. VL blips are defined as an unexplained VL between 50 and 1 000 copies/mL with VL suppression on repeat sampling, and are of limited clinical significance. Virological failure is defined as a VL >1 000 copies/mL on two consecutive assays taken at least 1 month apart from a patient on ART for at least 6 months. Virological failure precedes immunological failure which, in turn, usually precedes clinical failure, and allows early detection of adherence problems potentially prior to development of resistance mutations. Table 5 outlines management of adolescents with virological failure.
Not all adolescents with virological failure will have developed resistance. Resistance is more likely in regimens containing nevirapine, efavirenz and lamivudine as single mutations confer high-level resistance to these drugs. Since cross-resistance between nevirapine and efavirenz and other non-nucleoside reverse-transcriptase inhibitor (NNRTI) drugs occurs, adolescents failing an NNRTI-based regimen need to be switched to the standard second-line regimen as soon as possible to prevent accumulation of additional NRTI and/ or NNRTI resistance mutations that may compromise NRTIs and second-generation NNRTIs like etravirine that could be used in later regimens.[12] Adolescents can safely be switched to the second-line regimen without HIV drug-resistance testing (DRT) (if not available), as the resistance mutations are largely predictable if early switch occurs.[12] Adolescents with virological failure on a protease inhibitor (PI)-based regimen can continue intensive adherence counselling for longer periods to try to achieve virological suppression, as PIs have a high resistance barrier and are associated with less accumulation of NRTI resistance mutations even with high VLs >30 000 copies/mL.[12] Most patients with virological failure on a boosted PI will resuppress on this regimen with optimal adherence.
Where possible, it may be appropriate to have a specific clinic day with multidisciplinary team support for adolescents with adherence problems, virological failure and resistance.
In some cases virological failure secondary to poor adherence may prove intractable despite adherence interventions, and the resultant immunological and clinical failure could constitute a relative emergency. In such instances a period of inpatient directly observed therapy should be considered to stabilise the adolescent, identify critical clinical, psychosocial and mental health issues, and provide intensive interventions.[13] This should only be done in a multidisciplinary team setting in consultation with the adolescent and caregiver.
Indications for HIV DRT
The following are suggested criteria for DRT in adolescents: failing an NNRTI-based regimen for more than 1 year (although should ideally have been switched to a PI-based regimen earlier); or failing a boosted PI-based regimen (especially with a history of rifampicin-based tuberculosis (TB) co-treatment). To optimise results, DRT should be done only if VL >1 000 copies/mL; and if the adolescent has received ART for at least the past 4 weeks. Unfortunately it may not be possible to ensure adherence, and thus drug pressure, at the time of DRT if the adolescent claims adherence to be good. This will limit the interpretability of DRT as the resistant viral subpopulation may not be at adequate levels required for the DRT. The current DRT and all previous DRTs need to be combined with the treatment history to guide new regimen choices in treatment-experienced adolescents.
Drug-drug interactions
Table 6 summarises the most important drug-drug interactions in children and adolescents. It is advisable to consult an up-to-date medicines formulary and available online resources (www.hivdrug-interactions.org) prior to the prescription of any new agent where there is uncertainty about potential drug interactions.
ART side-effects and toxicities
Table 7 highlights the most significant side-effects and toxicities in adolescents. The clinician needs to be aware of the risks of using tenofovir in adolescents <15 years of age and <40 kg weight, with a low glomerular filtration rate (GFR) and Tanner staging of <3. Gynaecomastia, which is common in pubertal adolescent males in general, may be associated with efavirenz; careful management to avoid psychological distress and subsequent adherence problems is required.
Disclosure to adolescents
In order to fulfil their developing autonomy adolescents require accurate information regarding their health, including their HIV status. WHO recommends that disclosure occurs before 12 years of age, but this needs to be applied to each individual contexts-Consideration of the maturity and level of insight is essential. A child who enquires about their treatment and their health indicates a desire for further information and a need to start the disclosure process. Disclosure should be complete long before sexual activity begins. Disclosure may result in improved adherence, acceptance of the diagnosis and improved clinical outcomes.[15] Moreover, disclosure of maternal HIV status to the child may strengthen the relationship and build trust between mother and child.[16]
Caregivers need supportive counselling in order to prepare them for the disclosure process. Disclosure is not a once-off event, but a process, built on a foundation of health education, aiming to teach the child about maintaining their health, understanding their condition and beginning to take ownership of their own healthcare. Disclosure is never urgent, and is best done by the caregiver after adequate preparation. Many tools are available for facilitating disclosure, including talking books, picture books and comic books, some aimed at educating the adolescent, others guiding the caregiver. Adolescents also require support in connection with disclosing to sexual partners, friends, parents or any other individual, if and when this becomes desirable.
Transition to adult care
Transition of adolescents from child-focused care to adult-focused care may involve physical transfer to a different clinical space or may be a developmental shift with the adolescent moving from a supported to an independent, autonomous role within the same clinic. Regardless, planning to ensure safe and successful transition is required, as transition may be accompanied by significant anxiety and may result in disruption of care. All adolescents who transition to adult care must have undergone a disclosure process with ongoing support, information and reassurance.[17] Full communication to the adult-care practitioner, of all previous medical, sexual and reproductive health and psychosocial history, is essential. Ongoing attention to sexual and reproductive health needs, particularly access to contraception, is important for the transitioning adolescent.
In settings receiving these transitioning youth, familiarity with the complexities of managing HIV-infected youth from a medical and psychosocial perspective, a multidisciplinary team with co-ordination of all aspects of care, and appropriate linkage to other services including sexual and reproductive health services, psychological and psychiatric care are required.[17]
In conclusion, although many adolescents living with HIV have good outcomes on ART, adolescence is a high-risk period for non-adherence and associated virological failure. Clinicians need to be aware of adolescent-associated problems, and mechanisms to assist this population with a successful transition to adult care.
References
1. UNAIDS. Global Report: UNAIDS Report on the Global AIDS Epidemic 2013. Geneva: UNAIDS, 2013. [ Links ]
2. Shisana O, Rehle T, Simbayi L, et al. South African National HIV Prevalence, Incidence and Behaviour Survey, 2012. Cape Town: HSRC Press, 2014. [ Links ]
3. Violari A, Cotton MF, Gibb DM, et al. Early antiretroviral therapy and mortality among HIV-infected infants. New Engl J Med 2008;359:2233. [http://dx.doi.org/10.1056/NEJMoa0800971] [ Links ]
4. Judd A, Ferrand RA, Jungmann E, et al. Vertically acquired HIV diagnosed in adolescence and early adulthood in the United Kingdom and Ireland: Findings from national surveillance. HIV Medicine 2009;10(4):253-256. [ Links ]
5. Dollfus C, Chenadec JL, Faye A, et al. Long-term outcomes in adolescents perinatally infected with HIV-1 and followed up since birth in the French Perinatal Cohort (EPF/ANRS CO10). Clin Infect Dis 2010;51(2):214-224. [http://dx.doi.org/10.1086/653674] [ Links ]
6. Patel K, Hernan MA, Williams PL, et al. Long-term effectiveness of highly active antiretroviral therapy on the survival of children and adolescents with HIV infection: A 10-year follow-up study. Clin Infect Dis 2008;46(4):507-515. [ Links ]
7. Bakanda C, Birungi J, Mwesigwa R, et al. Survival of HIV-infected adolescents on antiretroviral therapy in Uganda: Findings from a nationally representative cohort in Uganda. PloS One 2011;6(4):e19261. [http://dx.doi.org/10.1371/journal.pone.0019261] [ Links ]
8. Nglazi MD, Kranzer K, Holele P, et al. Treatment outcomes in HIV-infected adolescents attending a community-based antiretroviral therapy clinic in South Africa. BMC Infectious Diseases 2012;12:21. [http://dx.doi.org/10.1186/1471-2334-12-21] [ Links ]
9. Nachega JB, Hislop M, Nguyen H, et al. Antiretroviral therapy adherence, virologic and immunologic outcomes in adolescents compared with adults in southern Africa. J Acquir Immune Defic Syndr 2009;51(1):65-71. [http://dx.doi.org/10.1097/qai.0b013e318199072e] [ Links ]
10. Van Cutsem G, Knight L, Abrahams M, et al. Outcomes in children, adolescent, youth and adults on ART in Khayelitsha. AIDS 2010 - XVIII International AIDS Conference; Vienna, 2010. [ Links ]
11. Agwu AL, Fairlie L. Antiretroviral treatment, management challenges and outcomes in perinatally HIV-infected adolescents. J Int AIDS Soc 2013;16(1):18579. [http://dx.doi.org/10.7448/ias.16.L18579] [ Links ]
12. PENPACT Study Team, Babiker A, Castro nee Green H, Compagnucci A, et al. First-line antiretroviral therapy with a protease inhibitor versus non-nucleoside reverse transcriptase inhibitor and switch at higher versus low viral load in HIV-infected children: An open-label, randomised phase 2/3 trial. Lancet Infect Dis 2011;11(4):273-283. [http://dx.doi.org/10.1016/s1473-3099(10)70313-3] [ Links ]
13. Purdy JB, Freeman AF, Martin SC, et al. Virologic response using directly observed therapy in adolescents with HIV: An adherence tool. Journal of the Association of Nurses in AIDS Care: JANAC 2008;19(2):158-165. [ Links ]
14. World Health Organization. Guideline on HIV disclosure counselling for children up to 12 years of age. Geneva: World Health Organization, 2011. [ Links ]
15. Calabrese SK, Martin S, Wolters PL, Toledo-Tamula MA, Brennan TL, Wood LV. Diagnosis disclosure, medication hiding, and medical functioning among perinatally infected, HIV-positive children and adolescents. AIDS Care 2012;24(9):1092-1096. [http://dx.doi.org/10.1080/09540121.2012.699670] [ Links ]
16. Kennedy DP, Cowgill BO, Bogart LM, et al. Parents' disclosure of their HIV infection to their children in the context of the family. AIDS Behav 2010;14(5):1095-1105. [http://dx.doi.org/10.1007/s10461-010-9715-y] [ Links ]
17. HIVguidelines.org. Transitioning HIV-Infected Adolescents into Adult Care. http://wwwhivguidelinesorg/clinical-guidelines/adolescents/transitioning-hiv-infected-adolescents-into-adult-care/ (accessed 15 April 2014). [ Links ]
 Correspondence:
Correspondence:
L Fairlie
lfairlie@wrhi.ac.za














