Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.104 no.7 Pretoria Jul. 2014
FORUM
HEALTH AND FINANCE
National expenditure on health research in South Africa: what is the benchmark?
F ParukI; J M BlackburnII; I B FriedmanIII; B M MayosiIV
IFathima Paruk, PhD, FCOG (SA), Cert Crit Care (SA), is Director of the Cardiothoracic Intensive Care Unit in the Department of Anaesthesiology and Division of Critical Care, Charlotte Maxeke Johannesburg Academic Hospital, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa (SA), and a member of the Human Research Ethics Committee at the University of Witwatersrand and of the National Health Research Committee (NHRC), Department of Health (DoH), SA
IIJonathan Blackburn, DPhil (Oxon), holds the National Research Foundation SA Research Chair in Applied and Chemical Proteomics in the Institute of Infectious Disease and Molecular Medicine and Division of Medical Biochemistry, Faculty of Health Sciences, University of Cape Town, SA, and is a member of the NHRC
IIIIrwin Friedman, MB BCh, FFPH (UK), is Public Health Physician in the Health Programme, SEED Trust, Durban, SA, a member of the Technical Task Team of the SA Health Products Regulatory Authority, which is linked to the SA DoH, and a former member of the NHRC
IVBongani Mayosi, DPhil, FCP (SA), is Professor of Medicine and Head of the Department of Medicine, Groote Schuur Hospital and University of Cape Town, and Chair of the NHRC. Fathima Paruk and Jonathan Blackburn contributed equally to this work
ABSTRACT
The Mexico (2004), Bamako (2008) and Algiers (2008) declarations committed the South African (SA) Ministry of Health to allocate 2% of the national health budget to research, while the National Health Research Policy (2001) proposed that the country budget for health research should be 2% of total public sector health expenditure. The National Health Research Committee has performed an audit to determine whether these goals have been met, judged by: (i) health research expenditure as proportions of gross expenditure on research and development (GERD) and the gross domestic product (GDP); and (ii) the proportion of the national health and Department of Health budgets apportioned to research. We found that total expenditure on health research in SA, aggregated across the public and private sectors, was R3.5 billion in 2009/10, equating to 16.7% of GERD. However, the total government plus science council spend on health research that year was only R729 million, equating to 3.5% of GERD (0.03% of the GDP) or 0.80% of the R91.4 billion consolidated government expenditure on health. We further found that R418 million was spent through the 2009/2010 Health Vote on health research, equating to 0.46% of the consolidated government expenditure on health or 0.9% of the R45.2 billion Health Vote. Data from other recent years were similar. Current SA public sector health research allocations therefore remain well below the aspirational goal of 2% of the national health budget. We recommend that new, realistic, clearly defined targets be adopted and an efficient monitoring mechanism be developed to track future health research expenditure.
High-quality research is essential for identifying the health needs and improving the health outcomes of a population.[1] Health research drives development, as it generates the knowledge needed to improve health systems performance and, ultimately, health and health equity.[2] Remarkable medical advances have taken place in South Africa (SA), such as the invention of computed tomography[3] and the first human heart transplant,[4] through investment in health research by government and industry. There has, however, been a perceived reduction in state expenditure on health research in real terms from the beginning of the 1980s,[5] characterised by a redistribution of state expenditure in the healthcare system towards primary healthcare and an apparent stagnation in real terms in the level of government-funded health research expenditure between 1996 and 2006.[6]
The Consensus Report on Revitalising Clinical Research in South Africa of the Academy of Science of South Africa (ASSAf)[5] has identified the low level of investment in clinical research as a major factor in SA's declining clinical research performance. This report recommended inter alia that developing countries should invest at least 2% of their gross domestic product (GDP) in research and development (R&D), and that 20% of gross expenditure on R&D (GERD) (i.e. 0.4% of the GDP) should be allocated to health research.[5] Against this background, the SA Ministry of Health, the Department of Health (DoH) and the National Health Research Committee (NHRC) have made a series of commitments to increase investment in health research through the country budget and the national health budget. For example, the National Health Research Policy of 2001[7] proposed that the country budget for health research should be raised to at least 2% of total public sector health expenditure. Subsequently, the Ministry of Health committed itself through the Mexico, Bamako and Algiers declarations to allocate at least 2% of the national health budget to research.[8-10] In addition, the 2011 National Health Research Summit report[11] recommended that the national DoH increase its funding for health research to achieve the 2% target of the national health budget.
This multiplicity of commitments, compounded by the lack of a detailed information system, renders interpretation of these commitments a complex process. The NHRC, which is a statutory body tasked with setting priorities for health research in SA, has therefore conducted an audit to determine the proportion of gross expenditure on R&D that has been spent on health research (as a proxy for the proportion of country budget spent on health research) in the past decade, as well as the proportion of the budget of the DoH that was spent on research in the period 2009/10 - 2012/13. We have compared these data with internationally accepted benchmarks as a way to judge historical trends and to provide a benchmark for future aspirations.
Sources of information
We used several sources of information on public and private expenditure on health research in SA, including the national surveys of research and experimental development of the Department of Science and Technology (1991/2 and 2009/10);[12-14] the Global Forum for Health Research (GFHR) reports Financing Research and Development for Health[15] and Monitoring Financial Flows for Health Research;[16] the National Treasury's 2013 Estimates of National Expenditure;[17] the ASSAf report Revitalising Clinical Research in South Africa;[5] the National Treasury's medium-term budget policy statements (2010 and 2012);[18,19] the 2001 Health Research Policy in South Africa document;[7] and the 2011 National Health Research Summit report Strengthening Research for Health, Innovation and Development in South Africa.[11]
Findings
Various recommendations for the minimum level of investment in health research, based on different metrics, are outlined in Table 1. [5,7,9,20] The 2001 Health Research Policy in SA was developed through consultation of relevant stakeholders by the Essential National Health Research Committee, the forerunner of the NHRC. This policy was adopted by the national DoH, but it was not presented to Cabinet or gazetted by Parliament.
In SA, health research is funded from multiple sources including local (public and private sectors) and foreign agencies. Moreover, in the public sector, health research funding is not exclusively provided by the DoH but also by the departments of Science and Technology and of Higher Education and Training. In view of the complexities of the SA health research funding model, we have used GERD - both as a proportion of the GDP and in absolute terms - together with the proportion of GERD (both in absolute and percentage terms) allocated to health research as surrogate indicators of total health expenditure on research in this country. Furthermore, we have established the total government sector expenditure on health research, as well as the specific DoH expenditure on health research, as proportions of the consolidated government expenditure on health. In the absence of accurate definitions of the 'health research budget' and 'total public health expenditure' in the National Health Research Policy of 2001, we used the consolidated government expenditure outcome on health as a proxy for the national health budget and the Health Vote as a proxy for the DoH's budget.
In this audit, we assessed performance against two metrics: (i) health research expenditure (government sector and total) as proportions of the GDP and GERD; and (ii) the proportion of national health budget and DoH budget apportioned to research.
Gross expenditure on R&D
Fig. 1 illustrates GERD for a basket of high-and low-middle-income countries (HICs and LMICs, respectively) for the year 2006, as well as for India (2004), New Zealand and Mexico (2005) and China (2007).[15,16]

The SA data relate to aggregated public and private sector funding sources and reveal that ~0.9% of the GDP was spent on R&D in 2006, which was well below the ASSAf target of 2% for a middle-income country. Countries that invested less than 0.9% of their GDP on R&D include India, Mexico and Greece, while China spent 1.49% of its GDP on R&D and established market economies spent 1.8 - 4.3%.
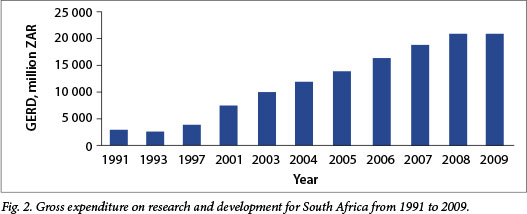
Analysis of GERD in SA for the period 1991 - 2009 reveals that it declined between 1991 and 1994 (Fig. 2). Since 1994 there has been a steady increase in the nominal value of GERD from under R4 billion to R20.9 billion in 2009/10, equating to an average increase of 11.7% per year during this period, which is well above the average inflation rate of ~6.5% for the same period (based on consumer price index (CPI) data from Statistics South Africa[21]). GERD in SA therefore increased ~2-fold in real terms over the period 1994 - 2009. Interestingly, although there was a R1.1 billion increase in public research expenditure in 2009/10 aggregated across government departments, science councils and higher education, the 9.7% reduction in research expenditure in the private sector in that year resulted in an overall decline in GERD from R21.04 billion in 2008/9 to R20.9 billion in 2009/10, probably reflecting the 2008/2009 global financial crisis. Notably, the percentage of the GDP spent on R&D has never exceeded 1% (Fig. 3), despite the annual growth in the economy exceeding 5% between 2006 and 2008. It declined from 0.92% in 2008/9 to 0.87% in 2009/10, and remains persistently below the ASSAf target of 2%.[5]

GERD spent on health research
Fig. 4 illustrates the investment in health research as a proportion of GERD for various HICs and LMICs made in 2005,[15,16] and reveals that for SA this figure was 14.8%. Furthermore, Fig. 5 shows that over the period 2001 - 2009, the percentage of GERD spent on health research has never exceeded 17%. The total R&D spend on health research in SA in 2009/10 has been reported at R3.5 billion, equating to 16.7% of GERD, which is close to the ASSAf recommendation of 20% of GERD to be spent on health research.[5] However, the aggregated SA government plus science council spend on health research in 2009/10 was only R729 million out of the total R&D spend on health research of R3.5 billion. According to the Department of Science and Technology's National Survey of Research and Experimental Development (2009/10),[14] the government sector expenditure on health research in that year was made up of ~R288 million government spend and ~R441 million science council spend; this represents an approximately 4-fold rise in government sector health research expenditure in real terms since 1991/2 from a nominal base of ~R54 million (equivalent to R187 million in 2009, adjusted by the CPI). Government sector spend on health research has therefore risen from ~1.9% of GERD in 1991/2 to 3.5% in 2009/10.


Proportion of national health budget spent on health research
The absence of adequate information systems makes it difficult to track trends of the DoH's investment in health R&D activities accurately. Blecher and McIntyre[22] reported that 1.1% of the total expenditure on health in SA in 1991/92 was spent on research. Fig. 6 illustrates the proportion of the national health budget of HICs and LMICs that was spent on health R&D for the year 2005. According to the GFHR, SA spent 1.6% of the national health budget on R&D in that year.[15,16]

The National Treasury medium-term budget policy statements (2010 and 2012)[18,19] record the consolidated government expend- iture outcome on health as R91.4 billion in 2009/10 and R114.1 billion in 2011/12, while the 2013 National Treasury Estimates of National Expenditure[17] records the audited Health Vote at R45.2 billion in 2009/10 and R55.3 billion in 2011/12. According to the audited figures contained in the 2013 Estimates of National Expenditure and the 2013 Health Vote documents, the major recipients of national DoH research funding in SA in 2011/12 were: (i) the Health Systems Trust to support health systems research activities, including the annual South African Health Review and the District Health Barometer; (ii) the Health Information Management, Monitoring and Evaluation Unit in the DoH, to develop and maintain a national health information system, and commission and co-ordinate research; (iii) the Human Resources Policy Research and Planning Unit, which is responsible for medium- to long-range human resources planning in the national health system and public entities; and other agencies such as (iv) the National Health Laboratory Service and (v) the South African Medical Research Council (MRC). The figures for 2009/10 through to 2012/13 are shown in Table 2, although it should be emphasised that the cumulative figures in this table are estimates, since not all allocations may be accounted for precisely in the 2013 Budget and Health Vote documents.
Collectively, the five major recipients of DoH funding for research constitute 0.46% (R417.9 million) and 0.35% (R403 million) of the consolidated government expenditure on health in 2009/10 and 2011/12, respectively (Table 2); these figures suggest that the DoH's expenditure on health research has fallen well below the 1.6% cited by the GFHR for 2005.[13,14]
These estimates for 2009/10 and 2011/12 are limited by the fact that they are derived from the Health Vote documents, which only identify five recipients of national DoH funding; we are aware that the DoH may fund other research-related activities, but these funding streams are not tracked and are therefore not reflected in the above calculation. The lack of complete health research funding records clearly highlights the need for adequate information systems to track financial flows and thereby accurately gauge health research financing streams in SA.
Despite the caveats set out above, these various figures imply that in recent years an inadequate proportion of the national DoH budget has been spent on health research, perhaps reflecting in part the consequences of the Mbeki-Dlamini-Msimang denialism and its impact on government funding for medical research. This inadequate expen- diture by the national DoH on health research is in sharp contrast to the fact that total health research expenditure in SA has increased from R384 million in 1991/2 to R3.5 billion in 2009/10;[12-14] taking into account the CPI, this means that there has been a 2.6-fold increase in total health research expenditure in real terms over the past 19 years, reflecting the new role of business and foreign governments as major funders of health R&D in SA.
The MRC is the DoH's primary research funding instrument; it is therefore of particular note that the MRC's audited baseline funding from the DoH increased from R221 million in 2007/8 to only
R238 million in 2011/12,[23] equating to an average increase of ~1.9% per annum over this period. However, during the same period the CPI increased by 6.8% per annum,[21] meaning that the MRC's baseline funding declined by 17.4% (~R50 million) in real terms between 2007 and 2011. The SA National Treasury's medium-term expenditure forecast (2013)[17] then estimates an increase in the MRC's baseline funding from R297 million in 2012/13 to R616 million in 2015/16, equating to an annual increase of 26.8% in nominal terms over the period 2011/12 - 2015/16.
We note that at present there is no direct public health sector research funding stream that flows to universities or provincial DoHs. For example, the conditional grant for health R&D of the mid-1990s has been replaced by the health professions training and development grant, which may not be used for research purposes. The policy framework of the professional education- and trainingfunding streams provided to the provincial health departments should therefore be clarified to enhance their contribution to health research.
Non-governmental funding for health research
Major contributors to health research funding in SA include pharmaceutical organisations and foreign not-for-profit entities such as the US National Institutes of Health (NIH) (which invests over $80 million per year in SA in the form of more than 400 research and research training awards; source NIH), the Bill and Melinda Gates Foundation and the Wellcome Trust. Precise details pertaining to funding from some of these sources are not readily available, but it is estimated, for example, that pharmaceutical companies spent R822 million on R&D (primarily including clinical trials) in SA in 2005/6.[24]
Discussion
The origin of the various commitments and recommendations made by the SA Ministry of Health, the DoH and the NHRC to allocate at least 2% of the national health budget to research can seemingly be traced back to the Commission on Health
Research for Development (COHRED) report of 1990, entitled Health Research: Essential Link to Equity in Development,[20]which recommended: 'All countries should vigorously undertake essential national health research (ENHR) to accelerate health action in diverse national and community settings ... Countries should invest at least 2% of national health expenditures to support ENHR studies this recommendation was further clarified in the report as 'We recommend that all governments commit 2% of their health budgets for ENHR.' As such, it seems clear that the COHRED report referred to government sector expenditure on health research, not total expenditure, and we therefore suggest that the various SA government commitments should henceforth be interpreted in that light.
Against this background, the analysis presented here shows that the expenditure on health research by the DoH of R403 million in 20011/12 equated to only 0.35% of the consolidated government expenditure on health (i.e. the national health budget) and only 0.73% of the Health Vote (i.e. the DoH's budget). If we relax the criteria to include total government sector spend on health research, the R729 million expenditure recorded for 2009/10 (the latest year for which data are available) equated to only 0.80% of the national health budget for that year. Therefore, by any logical metric -for example 'DoH research expenditure as a proportion of its own budget' or 'total government sector health research expenditure as a proportion of the national health budget' - the SA government's current allocations to health research are far below the aspirational target of 2% allocation of the national health budget to health research. These data suggest that health research expenditure by the government would need to at least double in order to provide appropriate levels of investment in health research and to approach the levels to which it has previously committed itself.
The data presented here demonstrate, however, that in contrast to general perception, total SA investment in health research from the aggregated public, private and foreign sectors has increased steadily in real terms during recent years judged by several metrics, a trend that seems set to continue in the short term at least. For example, the percentage of the GDP spent on R&D was 0.87% in 2009/10, GERD increased 2-fold in real terms from 1994 to 2009/2010, the percentage of GERD spent on health research was 16.7% in 2009/10, the government sector expenditure on R&D increased 4-fold in real terms from 1991/2 to 2009/10, and the total health research expenditure increased 2.6-fold in real terms from 1994 to 2009/10. However, we note that this total investment in health research in 2009/10 equated to only 0.15% of the GDP (GERD being 0.87% of the GDP and 16.7% of GERD being spent on health research), meaning that total investment in health research would need to at least double in order to approach the ASSAf target of 0.4% of the GDP and thereby provide appropriate levels of investment in health research in SA.
The global disparity in the distribution of funds for health R&D has resulted in many developing countries spending lower proportions of their GDP on health research, despite a high proportion of disease burden. It is therefore not surprising that in developing countries there is a perceived lack of capacity to develop innovative technologies to meet the health needs of the population. There is a concerted effort driven by the World Health Organization to redress these inequities. The Consultative Expert Working Group on Research and Development: Finance and Co-ordination (CEWG) has proposed novel strategies to incentivise, co-ordinate and sustain heath research in developing countries.[25] The CEWG proposes that all countries commit to contributing at least 0.01% (0.15 - 0.2% for developed countries) of the GDP on government-funded health R&D. They additionally recommend that the funds be pooled and managed centrally so that developing countries receive 20 -50% of the pooled funds. We suggest that these CEWG recommendations provide a more tangible and transparent aspiration and means to enable properly funded health research in SA than the current confused '2% of national health budgets to research' commitments. We therefore recommend that the CEWG proposals should be adopted by the SA government without delay.
The data presented here show that in 2009/10 the proportion of the R3.5 billion total health expenditure in 2009/10 attributable to SA government funding was only R729 million, meaning that government-funded health R&D constituted only 0.03% of the GDP in that year, close to the bottom of the CEWG-recommended range. Once again, these data suggest that there is considerable scope to increase government sector investment in health research immediately.
Among others, the data presented here illustrate the need to develop an efficient monitoring mechanism to track the level of expenditure on health research by governmental and non-governmental funders in the national health research system so that performance against international benchmarks can be assessed accurately. Such a national information system for health research expenditure will also be invaluable in enabling accurate assessment of whether health research funding is being effectively utilised to address SA healthcare priorities, and in addition will provide a means to better co-ordinate the activities of different government departments in the health research arena. As such, it should form a cornerstone of plans for the new National Health Research Observatory in SA now being developed by the NHRC.
A new consensus is emerging on the fundamental importance of a national health research system as an integral component in strengthening the public sector delivery system in preparation for the new National Health Insurance (NHI) system, the aim of which is to achieve a long and healthy life for all SA citizens.[26] The procurement and allocation of funds for research is one of the central functions of a health research system,[2] and the need for increased investment in R&D has been recognised. It is therefore of concern that, using the annual baseline allocations to the MRC in the period 2007/8 - 2011/12 as a barometer, the proportion of the budget of the national DoH that has been allocated to health research has been in decline in real terms in recent years, despite the fact that SA faces an unprecedented burden of infectious and non-communicable diseases. One step in the right direction will therefore be for the national DoH to progressively increase the percentage of the Health Vote allocated to health research, and we note encouraging signs of this in the 2013 Estimates of National Expenditure,[17] which forecast an increase in the MRC's baseline funding to R616 million in 2015/16, constituting a 26.8% average growth rate in nominal terms in the period 2011/12 - 2015/16. In addition, we note the recent launch of the new National Health Scholars Programme and the Strategic Health Innovation Partnership - both of which are partially supported by new budgets from the national DoH - as further evidence of progress towards developing new funding streams for expenditures on health research under the national DoH and its entities.
In conclusion, it seems clear from our analysis that neither the aspirational public commitments made by the the SA Ministry of Health to specific levels of funding of health research, nor the goals for funding of health research set out in the National Health Research Policy (2011), have been met and indeed that they may not be achievable in full in the short term. We therefore recommend that a new set of realistic, transparent, internationally accepted and more clearly defined targets be adopted forthwith as a means to ensure adequate future government investment in health research in SA.
Acknowledgements. This report is based on the work of the NHRC. We gratefully acknowledge the helpful comments of the following members of the Committee during the development of this manuscript: Prof. Nobelungu J Mekwa (Deputy Chair), Prof. Hoosen Coovadia, Prof. Mohamed Jeenah, Dr Edith N Madela-Mntla, Prof. Adelaide S Magwaza, Dr Zinhle Makatini, Prof. Dan L Mkize, Ms Catherine Mokgatle-Makwakwa, Dr Kebogile Mokwena and Ms Khanyisa Nevhutalu. We are grateful to Dr Mark Blecher (Treasury) for assistance with sources of information and to Mr Mpho Kgasi for secretarial support. We wish to express our gratitude to Dr Andrew Kanyegirire (COHRED) for permission to use published COHRED data to generate Figs 1, 4 and 6. We are particularly grateful to Prof. Wieland Gevers, Executive Director, ASSAf, for his insight and helpful discussions during the preparation of this manuscript.
1. IJsselmuiden C, Marais DL, Becerra-Posada F, Ghannem H. Africa's neglected area of human resources for health research - the way forward. S Afr Med J 2012;102(4):228-233. [ Links ]
2. Pang T, Sadana R, Hanney S, Bhutta ZA, Hyder AA, Simon J. Knowledge for better health: A conceptual framework and foundation for health research systems. Bull World Health Organ 2003;81(11):815-820. [ Links ]
3. Vaughan CL, Mayosi BM. Origins of computed tomography. Lancet 2007;369(9568):1168. [http://dx.doi.org/10.1016/S0140-6736(07)60562-5] [ Links ]
4. Barnard CN. The operation. A human cardiac transplant: An interim report of a successful operation performed at Groote Schuur Hospital, Cape Town. S Afr Med J 1967;41(12):1271-1274. [ Links ]
5. Mayosi BM, Dhai A, Folb P, et al. Revitalising Clinical Research in South Africa: A Study on Clinical Research and Related Training. Pretoria: Academy of Science of South Africa, 2009. [ Links ]
6. Coovadia H, Jewkes R, Barron P, Sanders D, McIntyre D. The health and health system of South Africa: Historical roots of current public health challenges. Lancet 2009;374(9692):817-834. [http://dx.doi.org/10.1016/S0140-6736(09)60951-X] [ Links ]
7. Department of Health. Health Research Policy in South Africa. Pretoria: DoH, 2001. [ Links ]
8. Mexico Statement on Health Research. Knowledge for Better Health: Strengthening Health Systems. From the Ministerial Summit on Health Research, Mexico City, 16-20 November 2004. http://www.who.int/rpc/summit/agenda/en/mexico_statement_on_health_research.pdf (accessed 24 March 2014). [ Links ]
9. The Bamako call to action: Research for health. Lancet 2008;372(9653):1855. [http://dx.doi.org/10.1016/S0140-6736(08)61789-4] [ Links ]
10. The Algiers Declaration: Ministerial Conference on Research for Health in the African Region - Narrowing the Knowledge Gap to Improve Africa's Health. Brazzaville, Congo: World Health Organization: Africa, 2008. [ Links ]
11. Mayosi BM, Mekwa JN, Blackburn J, et al. Strengthening Research for Health, Innovation and Development in South Africa: Proceedings and Recommendations of the 2011 National Health Research Summit. Pretoria: National Health Research Committee, South Africa, 2012. [ Links ]
12. Department of National Education. Resources for R&D in the Republic of South Africa 1991/1992. Results of Survey Programme No. 17. Pretoria: Department of National Education, 1993. [ Links ]
13. Department of Science and Technology. National Survey of Research and Experimental Development (2008/09 Fiscal Year). Pretoria: Department of Science and Technology, 2010. [ Links ]
14. Department of Science and Technology. National Survey of Research and Experimental Development (2009/10 Fiscal Year). Pretoria: Department of Science and Technology, 2012. [ Links ]
15. Landriault E, Matlin SA. The 2008 Report Card on Financing Research and Development for Health. Geneva: Global Forum for Health Research, 2009. [ Links ]
16. Burke MA, Matlin SA. Monitoring Financial Flows for Health Research 2008. Geneva: Global Forum for Health Research, 2008. [ Links ]
17. National Treasury, Republic of South Africa. Estimates of National Expenditure 2013. http://www.treasury.gov.za/documents/national%20budget/2013/ene/FullENE.pdf (accessed 24 March 2014). [ Links ]
18. National Treasury, Republic of South Africa. Medium Term Budget Policy Statement 2010. http://www.treasury.gov.za/documents/mtbps/2010 (accessed 24 March 2014). [ Links ]
19. National Treasury, Republic of South Africa. Medium Term Budget Policy Statement 2012. http://www.treasury.gov.za/documents/mtbps/2012 (accessed 24 March 2014). [ Links ]
20. Commission on Health Research for Development (COHRED) report of 1990: Health Research: Essential Link to Equity in Development. Cambridge, Mass: Oxford University Press, 1990. [ Links ]
21. Statistics South Africa. Consumer Price Index History. February 2014. http://beta2. statssa.gov.za/ publications/P0141/CPIHistory.pdf (accessed 24 March 2014). [ Links ]
22. Blecher MS, McIntyre D. Expenditure on health in South Africa, 1991/1992. S Afr Med J 1995;85(5):365-370. [ Links ]
23. National Treasury, Republic of South Africa. Estimates of National Expenditure 2011. http://www.treasury.gov.za/documents/national%20budget/2011/ene/FullENE.pdf (accessed 24 March 2014). [ Links ]
24. Kahn M, Gastrow M. Pharmacologically active: Clinical trials and the pharmaceutical industry. S Afr Med J 2008;98(2):114-116. [ Links ]
25. Rottingen JA, Chamas C, Goyal LC, Harb H, Lagrada L, Mayosi BM. Securing the public good of health research and development for developing countries. Bull World Health Organ 2012;90(5):398-400.
[http://dx.doi.org/10.2471/BLT.12.105460]
26. Mayosi BM, Lawn JE, van Niekerk A, Bradshaw D, Abdool Karim SS, Coovadia HM. Health in South Africa: Changes and challenges since 2009. Lancet 2012;380(9858):2029-2043. [http://dx.doi. org/10.1016/S0140-6736(12)61814-5] [ Links ]
 Correspondence:
Correspondence:
F Paruk
(Fathima.Paruk@wits.ac.za)
J M Blackburn
(Jonathan.Blackburn@uct.ac.za)
Accepted 6 April 2014.














