Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.104 n.2 Pretoria Feb. 2014
CONTINUING MEDICAL EDUCATION
ARTICLE
Screening for peripheral arterial disease
B Natha
MB ChB, FCS (SA), Cert Vascular Surgery (SA); Division of Vascular Surgery, Department of Surgery, Groote Schuur Hospital, Cape Town, South Africa
Atherosclerosis is the leading cause of coronary, cerebrovascular and peripheral arterial disease (PAD) worldwide. Sedentary lifestyle, stress and high-fat/carbohydrate diets have contributed significantly to the rising prevalence of atherosclerosis in most populations.
Preventive strategies are currently aimed at curbing the socio-economic burden of atherosclerotic disease and its consequences in healthcare systems. While myocardial infarction and cerebrovascular accidents are the two leading causes of mortality and long-term morbidity, atherosclerotic PAD remains an accurate marker of more generalised disease. Screening programmes for at-risk individuals with undiagnosed PAD should therefore be beneficial in preventing future cardiovascular and cerebrovascular events.
This article reviews the evidence and benefits of selective screening for PAD.
Definitions
Historically, the terms peripheral arterial disease (PAD), peripheral vascular disease, and chronic arterial occlusion have been used interchangeably. However, the general consensus is that PAD is an umbrella term used to describe a group of disorders that results in structural and functional alteration of arteries supplying blood to the viscera and limbs (excluding coronary and intracranial arteries).
It is also predominantly recognised as a chronic ischaemic condition that leads to progressive stenosis and possible occlusion of arteries.
Screening is a process of identifying apparently healthy people who may be at increased risk for a disease or condition.
For a screening protocol to be most effective, the disease process or condition being investigated should have the following characteristics:
- The disease process or condition should be common.
- It should be simple and inexpensive to identify the condition in its early stages.
- The condition should have a long latent period.
- The benefits of early treatment or secondary prevention should by far outweigh delayed intervention. Secondary prevention strategies should be widely available and cost-effective.
Epidemiology of PAD
Prevalence
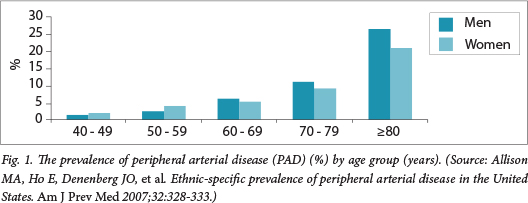
Numerous population-based epidemiological studies indicate that the prevalence of atherosclerotic PAD in the general population ranges from 3% to 14%. There is a significant- increase in prevalence to15- 25% in a population >70 years of age (Fig. 1).
Atherosclerosis is the primary aetiological process in 80% of patients with PAD.
Clinical presentation
For daily clinical and practical purposes, PAD can be classified as asymptomatic intermittent claudication or critical limb ischaemia. However, for a more detailed clinical classification the Fontaine or Rutherford classification systems are appropriate (Table 1).
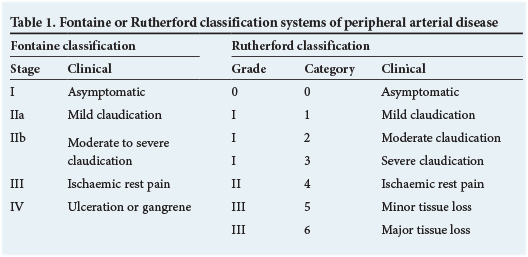
Both these classification systems attempt to stratify the extent of the atherosclerotic burden in the arterial tree with the clinical symptoms. They also allow an objective way of comparing different clinical sample cohorts for study purposes.
Regardless of the classification system used, the findings from population-based surveys demonstrate that 50 - 80% of people with PAD are asymptomatic or have vague atypical leg pain.
The lack of symptomalogy in people with obvious occlusive arterial disease can be explained by the observation that they adapt to their physiological and anatomical- limitations. They reduce their walking speed, adopt a more forgiving sedentary lifestyle or are impaired by other comorbidities that reduce their ambulatory activity and hence mask the underlying PAD symptoms. Therefore, the majority of people with PAD do not seek medical advice because the disease is seemingly benign and asymptomatic.
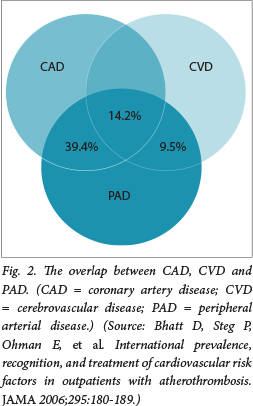
This clinical presentation is unfortunately not a true reflection of the aggressive nature of this disease process. Atherosclerosis does not selectively affect one arterial vascular bed in isolation; it is a generalised multivessel disease process. The PARTNERS (PAD Awareness,
Risk, and Treatment: New Resources for Survival) and REACH (Reduction of Atherothrombosis for Continued Health) surveys have shown a 40 - 60% association between PAD, coronary arterial disease and cerebrovascular disease (the strongest association being between peripheral and coronary arterial disease) (Fig. 2).
Natural history of PAD
The association between peripheral, coronary and cerebral arterial disease is clearly demonstrated when the long-term sequelae of PAD are assessed (Fig. 3).

Patients with asymptomatic PAD or atypical leg pain comprise 50 - 90% of an affected population, and have a good 5-year outcome as far as limb morbidity is concerned. Unfortunately, 20% of these patients will suffer from a non-fatal cardiac or cerebrovascular event and 10 - 15% will die from cardiovascular complications during the same time period.
The net result is that at 5-year follow-up, patients with asymptomatic PAD have at least a 20% reduced survival expectation than those without PAD.[1]
There is substantial evidence that risk factor and lifestyle modification for PAD significantly reduces cardiovascular and cerebrovascular events.
- All patients should be encouraged and supported with pharmacological agents and counselling to stop smoking.
- Those with diabetes mellitus should have their haemoglobin A1c (HbA1c) maintained around 6%.
- Patients with hypertension should aim to maintain a blood pressure equal to or below 130/85 mmHg and, if tolerated, should use an angiotensin-converting enzyme inhibitor (HOPE study).
- Meta-analysis of the major lipid trials recommends that the patient's low-density lipoprotein (LDL) be <2.59 mmol/l (for every 1 mmol/l decrease in LDL, there is a 20% reduction in the incidence of a cardiovascular event).
- The daily use of a low-dose antiplatelet agent such as aspirin is associated with a 25% odds reduction in experiencing a cardiovascular event (Antithrombotic Trialists' Collaboration).
- All patients should be encouraged to join a supervised walking programme.
Although PAD is a predominately asymptomatic condition, it is associated with serious long-term complications and mortality. Preventive strategies and screening are now more than vital. Targeted populations should be identified and matched with the most appropriate screening tools available.
Methods to screen for PAD
Clinical assessment
This should begin with a detailed history of the patient's claudication symptoms. Numerous epidemiological studies have attempted to address the efficacy of clinical assessment in screening for PAD. A large American study by Criqui et. al.[1] concluded that a history of claudication was only sensitive in 54% of cases and had a 10% positive predictive value in accurately diagnosing patients screened for PAD. This gross underestimation is due to the fact that the aetiologies of leg pain are diverse and not all related to arterial disease. Many patients were also missed because they were asymptomatic.
Physical examination with palpation of peripheral foot and wrist pulses has only a 50% sensitivity and a positive predictive value in confirming the diagnosis of PAD. This can be attributed to normal variation of arterial anatomy and congenitally absent pulses as well as inter-clinician variability.
Bedside investigations
A meta-analysis by Clarke et al.[2] indicated that an inter-arm systolic blood pressure difference of >10 mmHg is associated with a higher mortality and a 2.4-times higher risk ratio of PAD.
The most accurate bedside investigation for screening for PAD is the ankle brachial index (ABI) (Table 2). Fowkes et al.[3]
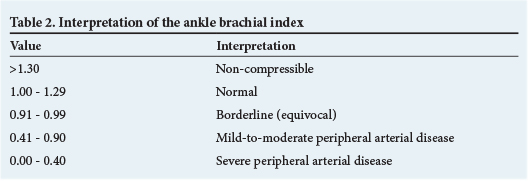
validated ABI measurements against digital subtraction angiography (DSA) to determine its sensitivity, specificity and accuracy as a lower extremity PAD diagnostic tool. An ABI of <0.9 has a 95% sensitivity and a 100% specificity compared with a DSA in detecting a 50% arterial stenosis and a 96% negative predictive value. An ABI of >1.3 is also pathological and represents diseased non-compressible arteries (most likely calcified).
There is also evidence that the lower the ABI the higher the likelihood of a cardiovasular event, as is demonstrated in Fig. 4.

A good clinical assessment and an ABI measurement are probably the most sensitive modalities with which to screen for PAD.
Who do we screen for PAD?
The United States Preventative Service Task Force and the American Heart Association do not advocate general population screening because the prevalence of PAD in asymptomatic PAD patients without cardiovascular risk factors is insignificant. General population screening is not cost-effective and may induce unnecessary stress in patients.
The American Heart Association recommendations for PAD screening are as follows:
- patients <49 years with diabetes and another risk factor
- patients >50 years with a history of smoking or diabetes
- all patients >65 years
- patients with an abnormal lower extremity pulse examination
- patients with atherosclerotic coronary, cerebral or renal arterial disease.
They also recommend that all patients should have a clinical assessment and an ABI as part of the screening. They further recommend smoking cessation, lipid lowering, antiplatelet therapy, and diabetes mellitus and hypertension treatment for individuals with asymptomatic lower extremity PAD.
The Trans-Atlantic Inter-Society Consensus (TASC) II document on the management of PAD also recommends selective screening/ surveillance for PAD.
TASC II recommendations
Recommendation 12 states that ABI screening to detect PAD should be performed on:
- all patients who have exertional leg symptoms
- all patients between the ages of 50 and 69 years who have a cardiovascular risk factor (particularly diabetes mellitus or smoking)
- all patients >70 years, regardless of risk factor status
- all patients with a Framingham risk score of 10 - 20%.
Based on the evidence briefly discussed above, the following approach to screening for PAD is suggested:
Why do we need to screen?
- PAD is common in a middle-aged/elderly population.
- Asymptomatic PAD and intermittent claudication are strongly associated with severe cerebrovascular complications and a significant mortality rate.
- There is overwhelming evidence that with early risk factor modification cerebrovascular events can be reduced.
How to screen?
- An ABI of <0.9 is the most sensitive method to confirm or exclude PAD. This should be done in conjunction with a clinical assessment.
Who to screen?
- Individuals who would benefit most from a screening programme are those known to have traditional atherosclerotic risk factors.
References
1. Criqui MH, Langer RD, Fronek A, et al. Mortality over a period of 10 years in patients with peripheral arterial disease. N Engl J Med 1992;326:381-386. [http://dx.doi.org/10.1056/ NEJM199202063260605] [ Links ]
2. Clark CE, Taylor RS, Shore AC, et al. Interarm blood pressure difference and vascular disease. Lancet 2012;379(9819):905-914. [http://dx.doi.org/10.1016/S0140-6736(11)61710-8] [ Links ]
3. Fowkes FG, Murray GD, Butcher I, et al. Ankle brachial index combined with Framinham Risk Score to predict cardiovascular events and mortality: A meta-analysis. JAMA 2008;300(2):197-208. [http://dx.doi.org/10.1001/ jama.300.2.197] [ Links ]
 Correspondence:
Correspondence:
B Natha
bhaveshnatha@gmail.com














