Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.104 n.2 Pretoria Feb. 2014
RESEARCH
A point-prevalence survey of public hospital inpatients with palliative care needs in Cape Town, South Africa
L van NiekerkI; P J RaubenheimerII
IMB ChB, MSc (Public Health); Department of Medicine, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
IIMB ChB, FCP (SA); Department of Medicine, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
ABSTRACT
OBJECTIVES: To assess the need for palliative care among inpatients occupying acute beds in the public sector hospitals of the Cape Town Metropole.
METHODS: A cross-sectional, contemporaneous, point-prevalence study was performed at 11 public sector hospitals in the Cape Town Metropole using a standardised palliative care identification tool. Data were collected on the socio-demographic characteristics, diagnoses, and prior and current care planning of patients.
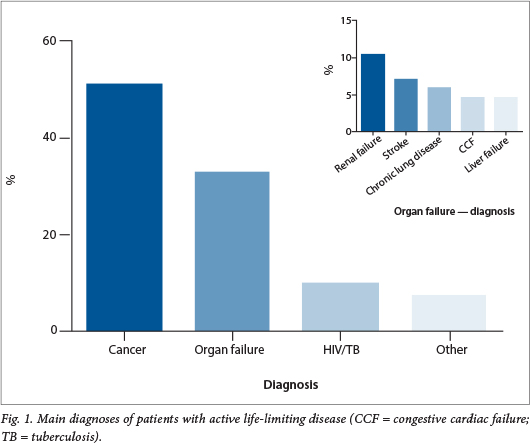
RESULTS: The case notes of 1 443 hospital inpatients were surveyed, and 16.6% were found to have an active life-limiting disease. The mean age of the group was 56 years. The diagnoses were cancer in 50.8%, organ failure in 32.5%, and HIV/tuberculosis in 9.6%. The greatest burden of disease was in the general medical wards, to which an overall 54.8% of patients meeting the requirements for palliative care were admitted.
CONCLUSIONS: This study provides evidence for the need for palliative care services in public sector hospitals and in the health system as a whole. The young age of patients and the high prevalences of end-stage renal failure and HIV are unique, and the burden in the general medical wards suggests a focus for initial inpatient programmes.
Palliative care involves a shift in the approach from curative modalities to comfort-focused care, which aims to improve the persons quality of life by providing relief of symptoms through psychological and supportive care, alongside medical treatment, in the last stage of life. This care is not exclusive to the person affected by the disease, but includes holistic care and support for the family. It aims to provide a person with a dignified death in his/her preferred place.[1] The need for palliative care is increasing globally, but is especially critical in developing countries. This need has mainly been informed from mortality statistics and disease prevalence. Of the 58 million annual deaths in 2008, 45 million occurred in developing countries.[2] The World Health Organization (WHO) estimates that approximately 9.67 million people are in need of palliative care across Africa.[3] A multi-country study conducted in Africa (Tanzania, Botswana, Ethiopia, Uganda and Zimbabwe) found the proportion of people requiring palliative care to be at least 0.5 - 1% of the total population.[3] South African (SA) statistics on mortality suggest that a large number of patients might potentially benefit from palliative care. In the Western Cape, for example, 65.3% of deaths can be attributed to three main disease groups: AIDS, cancer and non-communicable diseases (NCDs).[4] It has been estimated that 80% of cancer patients and 25 - 50% of HIV/AIDS patients will have pain in the terminal phase of their disease,[5] and it is increasingly recognised that the need for palliative care among those with NCDs is rising. Of global deaths, 80% of deaths due to NCDs are in low- and middle-income countries, and it is estimated that there will be a 300% increase in requirement for palliative care in such patients over the next 20 years.[2,6]
The need for palliative care among hospital inpatients has been well documented in Europe, but is not well established in Africa and SA.[7-10] In 2012, the prevalence of palliative need among Ugandan inpatients was published by Lewington et al.;[11] 46% of inpatients- were assessed as having an active life-limiting disease (ALLD), with HIV/AIDS being the commonest diagnosis. A recent survey at a large referral hospital in SA found that the inpatient mortality of medical patients admitted to the general medical service was 11%, with a 12-month post-discharge mortality of 35%; in many cases this was predictable on discharge, reflecting the burden of patients requiring palliative care in the acute medical service.[12]
In the face of resource constraints and the increasing demand for healthcare, it is becoming imperative for the SA health system to use existing resources efficiently and effectively. Research from Canada has found that in the last 6 months of their life people consume 21% of healthcare costs and occupy 24% of hospital days.[13] In the UK, every £1 spent on palliative cancer care was found to release a further £2 of hospital funds.[14] Significant cost savings from hospital-based palliative care consultation teams have been demonstrated, but even more savings are estimated to be achievable by providing patients with the necessary support to die at home.[15,16] A cost analysis conducted to evaluate the SA N'Doro hospital-based and outreach palliative care programme (Chris Hani Baragwanath Academic Hospital, Johannesburg) found that the cost per outreach visit was 50% less than the average cost of a patient day equivalent for district hospitals.[17]
The primary aim of this study was to measure the proportion of inpatients with ALLD who would be appropriate for palliative care intervention in the public hospitals of the Cape Town metropole.
Methods
A cross-sectional, contemporaneous, case note point-prevalence study was performed at each of the 11 public sector hospitals in the Cape Town metropole. The research was conducted between November 2011 and February 2012, excluding the 4 weeks of the December holiday period, as the hospital population is significantly lower during this time.
All occupied adult inpatient beds in the medical, surgical, gynaecology, oncology and short-stay emergency wards were included. This study focused on adult inpatients, and excluded obstetric and paediatric beds. Intensive care beds were also excluded, because prognostic prediction in this group is unreliable. All were acute-care beds, no long-stay or step-down beds being included. An independent medical practitioner performed the data collection. The sampling of inpatient beds in each hospital occurred on a single day where possible; for larger hospitals, sampling took place over 2 - 4 consecutive days. Weekends and Fridays were excluded.
A standardised tool for identification of patients with palliative care need was developed based on the UK Gold Standards Framework Prognostic Indicator Guidance and adapted for the SA context through consultation with local palliative and medical experts (Table 1). This tool has previously been piloted and used as a referral tool in a regional hospital in Cape Town.[18] The criteria for need for palliative care were based on two variables: an affirmative answer to the prognostic predictive question 'Would you not be surprised if the patient dies within the next 12 months?' and the presence of ALLD.

For all patients sampled, case notes were reviewed at the bedside and data were extracted on the socio-demographics, diagnosis, and presence of appropriate past and future care plans.
The research was commissioned by the Western Cape Department of Health, and ethical approval was obtained from the University of Cape Town Research Ethics Committee.
Results
The case notes of 1 443 patients in hospital beds were surveyed across 11 public hospitals providing acute care in the Cape Town Metropole. The average age of inpatients was 48 years (standard deviation ±17.5); 50.1% were male.
Prevalence of patients with an ALLD, potentially requiring palliative care
Using the defined survey tool, 240 patients were identified, comprising 16.6% of the total inpatient population sampled. This prevalence ranged from 7.1% to 28.7% across the various hospitals. The highest prevalence (44.4%) was in the oncology wards, followed by the medical wards (20.3%). It should be noted that only 2 of the hospitals sampled have oncology wards, the service being largely focused on providing curative care. However, the greatest burden of disease was found in the general medical wards: 54.8% of patients- meeting the requirements for palliative care were admitted to medical wards, 31.2% to surgical wards, 10.1% to oncology wards, and 3.3% to gynaecology wards.
Patient characteristics
The majority of patients (50.8%) had cancer, irrespective of which ward in the hospitals they were admitted to. In 32.5% of cases the life-limiting disease was a form of major organ failure, the most common being renal failure (10.4%), 9.6% of cases were attributable to HIV/tuberculosis (TB), and 7.1% of patients had other diagnoses, e.g. intracranial haemorrhage (Fig. 1).
More than half of the patients had an associated co-morbidity (diabetes, hypertension, HIV or TB) requiring additional care, and 37.9% had a Karnofsky Performance Scale rating of <50% ('patient requiring considerable assistance and frequent medical care'). In 3.3% of cases death was imminent (<24 hours).
Of the patients, 17.5% had a documented admission or casualty visit in the 6 months prior to their current admission: 12.5% of admissions were attributed to an acute exacerbation of pre-existing terminal disease (e.g. exacerbation of heart failure), 35.4% were due to a new but potentially expected complication related to the patient's preexisting terminal disease (e.g. a hip fracture in a patient with prostate cancer), and 38.3% were unrelated to the pre-existing terminal disease (e.g. a motor vehicle accident in a patient with renal failure).
Treatment and discharge planning
Of the patients 11.7% required inpatient palliative care (e.g. hospice facility or hospital palliative care bed), either because of severe symptoms or very poor social circumstances. Palliative needs could be met through appropriate outpatient home-based support in 79.2% of cases, while 9.2% of patients required a combination of services (e.g. initial acute symptom management in hospital/hospice followed by supportive further care at home). Only 21.3% of patients had existing documented advanced care directives in their case records.
Discussion
This is the first cross-sectional, contemporaneous, case note point-prevalence survey to assess palliative care need among hospital inpatients in SA. The data were collected from a variety of district, regional and central hospitals and are likely to be representative of other cities in SA.
The results from this study demonstrated that 1 in 6 (16.7%) of adult inpatients in the Cape Town metropole had an ALLD necessitating palliative care. This finding is comparable with similar surveys conducted in Europe and Australia, in which the point prevalence among inpatients ranged between 9.4% and 35%.[7-10] Of note, in these studies the mean age of patients requiring palliative care was over 70 years, in contrast to the mean of 56 years in our study. The single survey of palliative care needs in sub-Saharan Africa reported a 40% prevalence of palliative need among inpatients sampled in two Ugandan hospitals. This was largely ascribed to the HIV/AIDS burden in a setting where access to antiretroviral therapy is limited compared with the SA environment.[11]
In the present study, the primary diagnosis of the majority of patients needing palliative care was cancer. A third of patients identified had a primary diagnosis of organ failure. End-stage organ failure reflects the NCD burden experienced by SA.[91] A substantial number of patients had the diagnosis of end-stage renal failure (ESRF). In SA this is a life-limiting condition, even among younger patients, as resource constraints in the public healthcare system mean that access to chronic dialysis is limited. These patients, having a preventable condition with a treatment that is not accessible, have a very particular need for both intense counselling and forward planning for death. A lower than anticipated percentage of patients with palliative need had HIV/AIDS as a terminal diagnosis, which could be explained by the increase in access to and availability of antiretroviral treatment. A previous study of hospital inpatients in a large central hospital suggested that HIV status was not a predictor of poor outcomes in Cape Town, suggesting that most patients who- survive their initial admission would be expected to have a favourable long-term prognosis.[12]
The greatest burden of disease was in the general medical wards, where cancer was the predominant diagnosis. There are several reasons for this: 'medical beds' usually serve as 'diagnostic beds', so patients with undifferentiated disease are admitted there and cancer or end-stage organ disease is then diagnosed; there are limited oncology beds available, so the focus of oncology departments is on curative services or patients in whom good outcomes may be expected; and treatment options for patients with ALLD are largely limited to medical therapy. These patients admitted with end-stage chronic disease place an additional burden on acute medical beds in hospitals, already under strain with very high occupancy rates. Initial hospital-based programmes of palliative care treatment and co-ordination may want to focus on medical wards/beds.
The present survey reveals that long-term care of many patients will require resources and clear planning, especially since over half of the patients had additional chronic co-morbid disease such as diabetes, hypertension or HIV and over a third had a Karnofsky Performance Scale rating of <50%. All require clear long-term plans (about the intensity and kind of therapy that should be continued) that must be communicated to the long-term carers and other home-based care personnel to support families. There is a need for outpatient management and adequate home-based support for patients and their families, as the majority of patients are fit for discharge home. In most resource-constrained countries, a home-care model of palliative care predominates because of its affordability and acceptability to patients and family.[9]
This survey did not specifically set out to assess whether admissions could have been avoided. Given the pressure on acute beds in hospitals, the risks of hospital admission and patients' preferences not to be admitted, it is important to ask whether patients with palliative needs could be managed outside the hospital and whether admission could have been prevented. The combined high percentage of patients with previously diagnosed ALLD, with recent visits to the emergency department or with exacerbation of a pre-existing condition, suggests that such opportunities exist. In addition, to use existing acute hospital beds most efficiently, access to and availability of intermediate/step-down facilities must be improved.
Patients with life-limiting disease benefit from future care planning and advanced care directives (e.g. preferred place of death). Notably, only a fifth of patients in this survey with a clear palliative need had documented evidence of advanced care directives. In the UK, dying at home is the expressed wish of around 65% of people at the beginning of cancer and organ failure trajectories.[1] Assisting patients with formulating and documenting advanced care directives, for which improved training in palliative care among health professionals is necessary, will support future care planning and prevent unnecessary referral, hospital admission and inappropriate investigations at the end of life.
Conclusion
This survey documents the high prevalence of patients with palliative care needs occupying acute-care beds in the Cape Town Metropole. A notable finding of our study was the much younger average age of patients with palliative need compared with international samples, reflecting the dual burden of disease in general medical wards in particular, where patients with NCDs, cancer and HIV/ AIDS are admitted. Resource constraints result in patients requiring palliative care for conditions treatable in other international settings, e.g. ESRF. There are potential areas for great improvement in quality of patient care, with possible cost savings deriving from establishing palliative care programmes in primary care, improving care co-ordination across the different platforms of care, increasing training and exposure to palliative care for teams looking after inpatients, particularly in general medical wards, and establishing expert palliative care co-ordinating teams in large hospitals. Providing palliative care to patients not only relieves symptoms and improves patient satisfaction, but may also reduce admission rates and length of stay, and decrease the overall cost of care.
References
1. Murray SA, Kendall M, Boyd K, et al. Illness trajectories and palliative care. BMJ 2005;330(7498):1007-1011. [http://dx.doi.org/10.1136/bmj.330.7498.1007] [ Links ]
2. World Health Organization. Global Status Report on Noncommunicable Diseases 2010. http://www.who.int/nmh/publications/ncd_report_full_en.pdf (accessed 4 November 2013). [ Links ]
3. World Health Organization. A Community Health Approach to Palliative Care for HIV/AIDS and Cancer Patients in Sub-Saharan Africa. Geneva: WHO, 2005. [ Links ]
4. Bourne D, Matzopoulos R, Bradshaw D, et al. Western Cape Burden of Disease Reduction Project. Final report 2007. http://www.westerncape.gov.za/Text/2007/6/cd_volume_2_mortality_surveillance.pdf (accessed 4 November 2013). [ Links ]
5. Harding R, Higginson IJ. Palliative care in sub-Saharan Africa: An appraisal. Lancet 2005;365(9475):1971-1977. [http://dx.doi.org/10.1016/S0140-6736(05)67094-8] [ Links ]
6. Grant L, Dowing J, Namukwaya E, et al. Palliative care in Africa since 2005: Good progress but much further to go. BMJ Support Palliat Care 2011;1(2):118-122. [http://dx.doi.org/10.1136/bmjspcare-2011-000057] [ Links ]
7. Desmedt MS, de la Kethulle YL, Deveugele MI, et al. Palliative inpatients in general hospital: A one day observational study in Belgium. BMC Palliat Care 2011;10:2. [http://dx.doi.org/10.1186/1472-684X-10-2] [ Links ]
8. Morize V, Nguyen DT, Lorente C. Descriptive epidemiological survey on a given day in all palliative care patients hospitalised in a French university hospital. Palliat Med 1999;13(2):105-117. [ Links ]
9. To TH, Greene AG, Agar MR, Currow DC. A point prevalence survey of hospital inpatients to define the proportion with palliation as the primary goal of care and the need for specialist palliative care. Intern Med J 2011;41(5):430-433. [http://dx.doi.org/10.1111/j.1445-5994.2011.02484.x] [ Links ]
10. Sigurdardottir KR, Haugen DF. Prevalence of distressing symptoms in hospitalised patients on medical wards: A cross-sectional study. BMC Palliat Care 2008;7:16. [http://dx.doi.org/10.1186/1472-684X-7-16] [ Links ]
11. Lewington J, Namukwaya E, Limoges J, Leng M, Harding R. Provision of palliative care for life-limiting disease in a low income country national hospital setting: How much is needed? BMJ Support Palliat Care 2012;2(2):140-144. [http://dx.doi.org/10.1136/bmjspcare-2011-000188] [ Links ]
12. Stuart-Clark H, Vorajee N, Zuma S, et al. Twelve-month outcomes of patients admitted to the acute general medical service at Groote Schuur Hospital. S Afr Med J 2012;102(6):549-553. [ Links ]
13. Menee V, Lix L, Steinbach C, et al. Patterns of Health Care Use and Cost at the End of Life. Winnipeg, MB: Manitoba Centre for Health Policy, 2004. [ Links ]
14. Burke K. Palliative care at homes to get further funds if it saves money. BMJ 2008;328(7439):544. [http://dx.doi.org/10.1136/bmj.328.7439.544-b] [ Links ]
15. Morrison RS, Penrod JD, Cassel B, et al. Cost savings associated with US hospital palliative care consultation programs. Arch Intern Med 2008;168(16):1783-1790. [http://dx.doi.org/10.1001/ archinte.168.16.1783] [ Links ]
16. Hatziandreu E, Archontakis F, Day A, National Audit Office. The potential cost savings of greater use of home- and hospice-based end of life care in England. RAND Corporation. 2008. http:// www.rand.org/content/dam/rand/pubs/technical_reports/2008/RAND_TR642.pdf (accessed 4 November 2013). [ Links ]
17. Hongoro C, Dinat N. A cost analysis of a hospital-based palliative care outreach program: Implications for expanding public sector palliative care in South Africa. J Pain Symptom Manage 2011;41(6)1015-1024. [http://dx.doi.org/10.1016/j.jpainsymman.2010.08.014] [ Links ]
18. DesRoisiers T, Cupido C, Pitout E, et al. A hospital-based palliative service for patients with advanced organ failure in sub-Saharan Africa reduces admissions and increases home death rates. J Pain Symptom Manage 2013;21 August. [Epub ahead of print] [http://dx.doi.org/10.1016/j.jpainsymman.2013.05.021] [ Links ]
19. Mayosi BM, Flisher UG, Sitas F, et al. The burden of non-communicable disease in South Africa. Lancet 2009;374(9693):934-947. [http://dx.doi.org/10.1016/S0140-6736(09)61087-4] [ Links ]
 Correspondence:
Correspondence:
P J Raubenheimer
peter.raubenheimer@uct.ac.za
Accepted 7 October 2013.














