Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.104 no.2 Pretoria Fev. 2014
RESEARCH
The cost of harmful alcohol use in South Africa
R G MatzopoulosI; S TruenII; B BowmanIII; J CorrigallIV
IBBusSci, MPhil (Epidemiology), PhD; School of Public Health and Family Medicine, Faculty of Health Sciences, University of Cape Town, South Africa. Burden of Disease Research Unit, South African Medical Research Council, Parow, Cape Town, South Africa
IIBEcon (Hons), MEcon; DNA Economic Consultancy, Hatfield, Pretoria, South Africa
IIIBA (Hons), PhD; School of Human and Community Development, Faculty of Humanities, University of the Witwatersrand, Johannesburg, South Africa
IVMB ChB, MMed (Public Health), FCPHM (SA); School of Public Health and Family Medicine, Faculty of Health Sciences, University of Cape Town, South Africa
ABSTRACT
BACKGROUND: The economic, social and health costs associated with alcohol-related harms are important measures with which to inform alcohol management policies and laws. This analysis builds on previous cost estimates for South Africa.
METHODS: We reviewed existing international best-practice costing frameworks to provide the costing definitions and dimensions. We sourced data from South African costing literature or, if unavailable, estimated costs using socio-economic and health data from secondary sources. Care was taken to avoid possible causes of cost overestimation, in particular double counting and, as far as possible, second-round effects of alcohol abuse.
RESULTS: The combined total tangible and intangible costs of alcohol harm to the economy were estimated at 10 - 12% of the 2009 gross domestic product (GDP). The tangible financial cost of harmful alcohol use alone was estimated at R37.9 billion, or 1.6% of the 2009 GDP.
DISCUSSION: The costs of alcohol-related harms provide a substantial counterbalance to the economic benefits highlighted by the alcohol industry to counter stricter regulation. Curtailing these costs by regulatory and policy interventions contributes directly and indirectly to social well-being and the economy.
CONCLUSIONS: Existing frameworks that guide the regulation and distribution of alcohol frequently focus on maximising the contribution of the alcohol sector to the economy, but should also take into account the associated economic, social and health costs. Current interventions do not systematically address the most important causes of harm from alcohol, and need to be informed by reliable evidence of the ongoing costs of alcohol-related harms.
The economic, social and health costs associated with alcohol-related harms are important considerations for determining policies and regulation of alcohol access. In South Africa (SA) two estimates are frequently cited to characterise the various costs of- alcohol-related harms. In 2003 Parry et al.[1] conservatively estimated these at R8.7 billion, or 1% of the gross domestic product (GDP), based on the method of Single et al.[2] Budlender[3] estimated that R17 billion was allocated by national and provincial government for expenditures related to addressing alcohol-related harms in 2010 compared with R16 billion in tax and excise revenue, an annual loss to the fiscus of R1 billion. However, the study underestimated social costs, as it omitted costs borne by local government and individuals.
As useful as these studies have been for stimulating an evidence-based approach to addressing alcohol harms, their limited scope suggests that they underestimate the true costs to the economy. Parry et al}[1]-provided estimates in the absence of other suitable costing studies, but questioned the applicability of methods derived from high-income countries. Budlender,[3] noting that government expenditures addressing alcohol harms occurred within general allocations, selected lower values from possible cost ranges and omitted several cost items to avoid overestimation. Government spending also only accounts for a fraction of the total costs incurred from harmful alcohol use. Government spending on mitigating the impact of alcohol abuse incurs significant opportunity costs in terms of foregone spending or investment in more socially desirable avenues. At an individual level, it is estimated that 13% of discretionary disposable income was spent on alcohol consumption in 2005,[4] which in a resource-constrained country such as SA could have been used more productively.
We aimed to provide a more comprehensive cost estimate to inform evidence-based alcohol policy and legislation by applying cost calculation methods informed by current best practice frameworks. The research was commissioned by the National Liquor Authority, a division of the SA Department of Trade and Industry, which regulates the manufacturing and distribution of alcohol.
Methods
Moller and Matic[5] distinguish between three cost dimensions that comprise the full economic welfare costs of harmful alcohol use, namely: (i) health and crime expenditures, in which resources are allocated to address alcohol-related harms; (ii) labour and productivity costs, in which the effect of alcohol on economic output and production is quantified; and (iii) non-financial welfare costs, such as pain, suffering and loss of life or of 'quality of life', which do not have a monetary value. Another important distinction is made between costs borne by drinkers themselves (internal costs) and those borne by government or society at large (external costs).[5] The method of Single et al.[2] was applied to calculate costs attributable to alcohol use across these dimensions, supplemented by the avoidable costs of alcohol described by Collins et al} [6]
As costing studies estimate the total cost to society (internal and external costs), care must be taken not to include separate estimates of internal and/or transfer costs, which would result in double counting. To illustrate, an individual disabled by alcohol abuse may receive disability payouts from government. This payout is a transfer cost - the money is transferred from the taxpayer to the disabled individual, but is not lost to the economy, and therefore should not be counted as a cost of alcohol abuse. Including such transfer costs would effectively double count the external costs of productivity losses and overestimate the social costs involved in harmful alcohol use.[7]
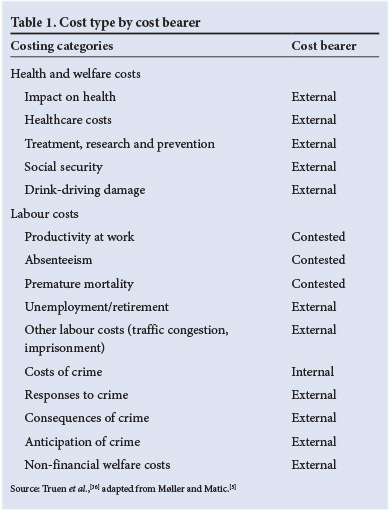
Secondary health and economic data provided estimates for which no figures exist in the literature. Where no suitable local data were available, we applied data from comparable countries. Although not optimal, the use of estimates is preferable to omitting cost components entirely, which would result in systematic underestimation of total costs.[5] We applied a prevalence-based approach that estimates current costs of past harmful alcohol use, rather than an incidence-based approach that includes future costs of current consumption. Cost categories and the primary bearer for each are summarised in Table 1.
Results
Health and welfare costs Impact on health
Alcohol, the most widespread drug of abuse in SA, is the most harmful drug at a population level. It is the third-largest contributor to death and disability after unsafe sex/sexually transmitted infections and interpersonal violence, both of which are themselves influenced by alcohol consumption.[8] In total, 36 840 deaths (6.1% of total mortality), 787 749 years of life lost (7.4% of premature mortality) and 344 331 years lived with a disability (6.2% of total disability) were attributable to alcohol, [9] which together accounted for more than 1.1 million disability-adjusted life years (DALYs), or 7% of the total disease burden.[10]
More recent analysis has included the contribution of alcohol to infectious diseases,[11-13] which increased the estimated total alcohol attributable DALYs for SA to more than 1.3 million in 2004.[11,12]
Injury-related causes account for nearly half (41%), with the largest single contribution from intentional injuries, i.e. interpersonal violence and suicide, at 25%. Unintentional injuries, including road traffic injuries, accounted for 16% of DALYs. Infectious diseases accounted for a third of DALYs, with tuberculosis (18%) and HIV/ AIDS (13%) being the largest contributors. Non-communicable diseases accounted for the remaining alcohol-attributable DALYs, with neuropsychiatric disorders, including epilepsy and common mental disorders, the single largest component (12%).[11,12]
Healthcare costs
A common method used to derive healthcare costs is to calculate the alcohol-attributable fraction (AAF) for each health condition that is caused by alcohol and then to apply the AAFs to the costs of treatment for cases presenting to the health system for each diagnosis.[14] Table 2 presents estimated AAFs for SA from recent burden of disease studies. Calculation of treatment costs is complicated by the absence of reliable national healthcare cost data that match health outcomes to healthcare expenditure. There is considerable cost variation across diagnoses and also between cases with the same diagnosis but treated in different levels of state facilities or in the private healthcare system. There are hospital-based cost studies,[15] but these are not representative of hospital admissions or health-seeking patterns. The private healthcare system collects suitable data,[16] but these are not available publicly.[17]
Budlender [3] estimated the cost of alcohol-related treatment to public healthcare by applying an estimate of 9.2% for each province. This was based on the estimated 14.5% of net DALYs attributable to alcohol for males and 3.9% for females[13] and may be an underestimate,[3] but is preferable to others as it includes the burden of infectious disease. In generating an estimate of the cost of alcohol to the national and provincial health departments at R6 billion per annum, Budlender [3] identified several health sub-programmes where alcohol may have a more pronounced effect on cost, namely coroner services, emergency transport, tuberculosis hospitals and forensic services.
The public health service, which treats 70 - 80% of the population, accounts for less than half of all health expenditure (42%), with per capita spending on healthcare in the private sector being 3.5 - 5.5 times higher.'[18] The private sector is roughly equivalent to the public health sector in terms of total spending,'181 but to adjust the estimate for the different disease profiles we halved the estimated private sector spending for health outcomes treated primarily in the public sector, such as liver cancers, hypertensive disease and type 2 diabetes. This equated to private sector spending on alcohol-attributed causes of R3.33 billion. Together with public sector spending, the estimated total healthcare cost is R9.33 billion. However, this ignores outpatient and primary care costs, which, according to a European review, [19] ranged from 25% to 65% of total inpatient health costs. Applying the lowest of these estimates, 25%, implied a further R2.33 billion, bringing the total healthcare cost in 2009 to R11.66 billion.
Treatment, research and prevention
Alcohol-related health costs encompass the treatment of individuals with disorders, social costs for dependants, and costs related to research and prevention. Alcohol abusers account for more than half of all patients in treatment for drug addiction,[20] the costs of- which are partially borne by the Department of Social Development. Budlender [3] attributes these costs to national and provincial government treatment programmes. Budlender's study omits costs of private treatment and treatment in partially subsidised centres and those maintained by local government agencies. The estimated research costs to government were limited to an estimated R6 million per annum across all science councils, which excluded direct ad hoc research spending by other provincial and national government departments (e.g. the current study) and projects undertaken by local government agencies, as well as alcohol treatment and prevention research by universities and non-governmental organisations, such as Soul City and the Open Society Foundation. [3] It would be preferable to attribute a percentage of all social welfare and health research spending to alcohol, but in the absence of suitable data, we applied an estimate of R18 million to take into account social welfare and private spending on research, a tripling of Budlender's estimate for spending across all science councils.
Social security
To estimate the social care and welfare costs of alcohol to the state, Budlender[3] allocated 20% of the Social Development budget for the care and support of families, 1% of the youth development budget, 2% of the cost of services, 1% of disability grants and an undisclosed percentage of HIV/AIDS costs. We estimated alcohol-attributable allocations from government departments, applying an AAF of 4% for HIV/AIDS (Table 3).
Drink driving damage
The CSIR estimated the cost of traffic crashes to the national economy in 2002 at R42.5 billion, which equated to R67.6 billion in 2009. [21] This included human casualty costs (56%), already reflected in healthcare costs, and a further 44% in vehicle damage and incident costs, i.e. R29.7 billion. This is likely to be an underestimate, as the Council for Scientific and Industrial Research study omitted ancillary costs. A Californian study indicated that monetary costs account for less than half of the costs of alcohol-attributable crashes (47%), with the rest accruing from 'quality of life', including medical expenses, property damage, employer costs, costs to public services and travel delays. [22]
An estimated 24% of SA driver deaths and non-fatal injuries would be prevented if drivers were not driving under the influence of alcohol.[23]As drunk drivers are also likely to be over-represented among those involved in collisions with pedestrians and cyclists and in crashes in which motor vehicle passengers are killed, we proposed that all other collisions would be reduced to a similar extent. This is congruent with a US study that estimated alcohol-attributable costs to crash victims at 27%.[22] The alcohol-attributable fraction of 27% was applied to the R29.7 billion total crash cost to estimate a R7.9 billion total annual vehicular damage cost of alcohol-involved crashes in SA.
Labour costs Productivity at work
Alcohol misuse is a risk factor for work-related injuries, increased absenteeism and high employee turnover.[24] A significant proportion of school-age adolescents (29%) also misuse alcohol,[25] which can be linked to absenteeism and academic failure. Another systematic review[26] found that alcohol abuse increased the likelihood of drug abuse and risky sexual behaviour, which reduced human capital development and thus the ability of citizens to participate in and contribute to society.
Moller and Matic[5] suggest that the impact of harmful use of alcohol on labour supply and overall productivity is discernible through the- following four channels: lower productivity due to hangovers or drunkenness at work; absenteeism due to hangovers; unemployment and retirement effects; and other labour costs. While common sense suggests that a drunken individual, or one suffering from a hangover, is likely to be less productive than a sober individual, in practice studies have not yielded the expected results. Rather there is an inverse U-shaped relationship between wage levels and alcohol consumption.[27-29] The relationship between problem drinking and wages suggests a reduction in productivity, but the evidence is mixed. [29] In the absence of conclusive research, an estimate of the impact on productivity in SA is not warranted.
Absenteeism
There is a paucity of research on the proportion of sick-days attributable to harmful alcohol use. A typical assumption is that 4 - 6% of absenteeism is due to harmful alcohol use. [5] A single study conducted by a commercial firm and covering 7 000 employees in 60 firms found that absentee rates average 2.3% in workers earning R1 000 or less per month,- and 1.3% in workers earning R10 000 -15 000 per month. We calculated the cost of absenteeism by multiplying employee compensation by absenteeism rates, by the fraction of absenteeism attributable to alcohol, and finally by the productivity loss factor. Given total employee compensation costs of R1 081.4 billion in 2009, the alcohol-attributable fraction approach suggests that the cost of alcohol-attributable absenteeism ranges from R140.6 million to R447.7 million annually.
Premature mortality and morbidity
One method of calculating the cost of mortality and morbidity is to estimate the net present value of the earnings stream that an individual would have earned if it had not been for the event that resulted in premature death or disability. A key problem with this approach is that it produces different values for deaths between, and even within, countries. In SA, where unemployment levels are high, low-skill workers can be replaced relatively easily, and the cost to the economy of premature death may be limited to the friction associated with finding a new employee. [5] We sought to measure the economic value of premature mortality by estimating the average amount an individual would be willing to pay to prevent death, which generates a value of statistical life (VSL). VSLs must be treated with some caution,[30] but they do estimate the value society places on averting premature mortality, which takes into account the emotional costs of such mortality.
Using average per capita employee compensation as a proxy, based on 2009 GDP'[31] and mid-year population estimates, [32] the economic benefits lost as a result of premature mortality in SA equate to R21 632 per death. The total impact on society is substantially higher if emotional costs are included. Miller'301 suggests that the best estimate of VSL is 143 times the per capita GDP. Lindhjem et al. [33] provide a more conservative estimate of mean VSL of 73.8 times the per capita GDP in countries with similar purchasing power parity-adjusted per capita GDPs to that of SA.
At 2009 per capita GDP levels, Lindhjem et al.'s [33] VSLs suggest that the average SA citizen would pay R3.5 million to prevent their death. The total VSL-projected costs of the 36 840 - 46 153 alcohol-attributable deaths calculated by Schneider et al. [9] and Rehm et al.[13] amount to between R128.9 billion and R161.5 billion, or 5.0 - 6.8% of the GDP. As approximately 22.5 years of life are lost per alcohol-attributable death, the estimated 339 263 years lost to disability are equivalent to 15 075 premature deaths, or a VSL of R53.3 billion (an additional 2.2% of GDP).
Unemployment and early retirement
There are several ways in which harmful alcohol use can impact on the probability of a person's finding employment. However, in practice the extent to which problem drinking is associated with unemployment may depend on whether intoxication is felt to be socially acceptable, and on absolute poverty levels. For example, poverty could constrain the purchase of alcohol among the poor, making problem drinking the preserve of the employed. However, the nature of the relationship is unclear.[5]
Other labour costs
Most sources of alcohol-related decreases in labour productivity reflect the reduction in the amount of time available to work. Examples include delays in getting to work due to traffic congestion caused by alcohol-attributable accidents, time spent incarcerated due to crimes committed under the influence of alcohol, and time spent caring for those disabled by alcohol-attributable health problems.[5] Data to estimate the size of these impacts on labour productivity in SA are not available.
Costs of crime
Alcohol-attributable crime imposes a significant cost burden. A US study estimated that alcohol-attributable crimes cost more than double those attributable to drugs, with alcohol-related violent crimes accounting for more than 85% of total costs for alcohol and drug-related crimes.[34] Neither violent crimes nor alcohol-related harms are as pronounced in the USA as in SA, which implies that these costs may be yet higher in SA. A recent study using accounting methodology provided an aggregated cost of crime in SA of US$22.1 billion or 7.8% of the GDP in 2007 (R155 billion at an approximate 2007 exchange rate of R7:$1).[35] This study's superficial burden of disease analysis significantly underestimates the true extent of homicide, and it is likely that the cost of crime is similarly underestimated. Crime costs in low- to middle-income countries in Latin America with high crime levels, such as Colombia, Brazil or Venezuela, range from 5% to 15% of the GDP. Moller and Matic[5] distinguish between three categories of costs related to crime in order to avoid double counting and then apportion a share of these costs to alcohol: (i) costs in response to crime; (ii) costs as a consequence of crime; and (iii) costs in anticipation of crime.
Costs in response to crime
Alda and Cuesta[35] estimated the institutional costs incurred by SA government agencies in responding to crime, including correctional services, justice and police and public security, at $7.169 billion in 2007 (R50 billion at an exchange rate of R7:$1), equivalent to 2.55% of the GDP. Applying Budlender's[3] AAFs of 22.5% for police and public security, 38.5% for correctional services and 2% for justice costs, it is estimated that costs of R9.68 billion were attributable to alcohol. [36]
Consequences of crime
Alda and Cuesta[35] calculated health costs relating to crime to have been $7.37 billion (R52 billion) in 2007, equivalent to 2.6% of the GDP. Two-thirds accrued from the contribution to disease burden and productivity losses and the rest primarily from emotional costs, with medical costs accounting for less than 1%. The estimated economic costs of foregone foreign direct investment of $1.287 billion (R9 billion) and transfer costs of $3.426 billion (R24 billion) from theft of residential property, vehicles, weapons and livestock also need to be included. Assuming that 75% were- relevant to alcohol use, Budlender's[3] AAF of 25% suggests that R1.7 billion was lost in foreign direct investment and R4.5 billion in transfer costs. In addition, Budlender estimated the cost of victim empowerment, among social development costs, at R109 million across national and provincial departments in 2009.
Anticipation of crime
Economic costs of crime are also incurred in anticipation of criminal activity, via expenditures on security measures such as anti-theft devices and guards. Moller and Matic[5] could identify only one comprehensive study that included these costs, which were found to be of a similar scale to costs in response to crime. Alda and Cuesta[35] estimate that $2.83 billion (R20 billion) was spent on private security for businesses and households in 2007. Applying a fraction of 75% for alcohol-relevant costs and Budlender's AAF of 25%[3] provides an estimate of R3.7 billion for costs attributable to alcohol in anticipation of crime.
Non-financial welfare costs
The emotional costs placed on premature mortality and morbidity associated with alcohol are obtained from the amounts that individuals would pay for their prevention. Additional non-financial welfare costs accrue to people affected by the actions of others who misuse alcohol. It is not possible to estimate the value of all non-financial welfare costs associated with alcohol consumption, but in the SA context the following two examples, relating to traffic crashes and crime, suggest that these are likely to be substantial. Miller[22] and Rosen et al.[37] suggest that the cost of emotional pain associated with traffic crashes and violent crime, respectively, is approximately the same as the economic costs, which would equate to R12.9 billion for traffic crashes. Alda and Cuesta[35] estimate that one-third of health costs relating to crime can be attributed to emotional costs. Applying 75% of their total healthcare cost of $7.37 billion in 2007 (R52 billion) for 'alcohol-relevant' costs and an AAF of 25% suggests that emotional costs of alcohol-related crime are approximately R3.2 billion.
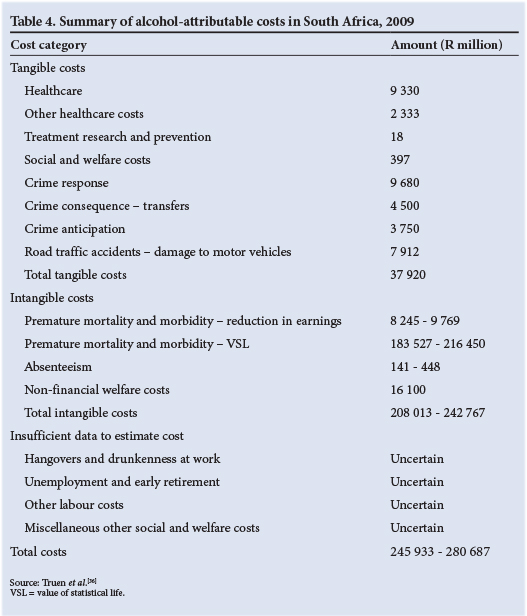
Summary of total alcohol-attributable costs
A summary of the costs attributable to harmful alcohol use, based on the analysis of secondary sources described in the preceding section, is shown in Table 4. Total tangible and intangible costs represent 10 -12% of 2009 GDP. The tangible financial costs of harmful alcohol use alone amount to an estimated R37.9 billion, or 1.6% of the 2009 GDP.
Discussion
The SA alcohol industry poses complex challenges for policy makers. While it makes a considerable contribution to the domestic economy through employment, output and export earnings, it imposes enormous social and emotional costs. Alcohol ranks as the most harmful of a selection of 20 drugs, based on the magnitude of harms the drug causes both to drinkers and those affected by drinking.[38] Inclusion of the intangible, non-financial costs of the trauma associated with alcohol-related illness, injury and violence goes some way towards indicating how much value citizens place on any intervention that would help to mitigate this trauma. VSL estimates in particular suggest that South Africans would be willing to pay R183.5 - 216.5 billion, or 8 - 9% of the GDP, to avoid the deaths, illnesses and disabilities caused by alcohol. These figures still underestimate the total cost of alcohol, as there were insufficient data to estimate several entire cost categories, and the VSL estimates excluded many sources of psychological trauma.
There will always be gaps in locally relevant data requiring the imputation of costs. Costing studies will continue to produce underestimates of harms if generation of the type and quality of data required for costing exercises is not considered important in the day-to-day routines of both the public and private sectors. For example, the current study could not include estimates of the costs related to employee hangovers or drunkenness at work. Given the high rates of alcohol consumption, these are likely to be frequent outcomes with a significant impact on the SA economy. The systematic collection and release of such data are therefore crucial to estimating the full socio-economic impacts of alcohol-related harms. Expressing these in economic terms provides necessary leverage to drive the political will, and gain popular support, for evidence-based interventions at both national and provincial levels.
Ideally, interventions should be designed so as to minimise the social and economic costs of alcohol abuse, while limiting the impact on the industry's generation of economic benefits. The figures in this study point to a disproportionate investment in intervention strategies that seek to address alcohol-related harms that are not the major contributors to the country's burden of disease.[36] For example, the alcohol industry, via its statutorily required anti-abuse initiatives, invests heavily in fetal alcohol syndrome (FAS) prevention, driver safety messaging, and educational campaigns targeting adolescents. However, FAS constitutes less than 6% of the total alcohol-attributable burden of disease, whereas violence, followed by tuberculosis, unintentional injuries and HIV/AIDS, are the major contributors, together accounting for nearly three-quarters of the burden.'91 Pedestrians rather than drivers are most at risk for alcohol-related traffic fatalities. The group at highest risk for alcohol-related harms is aged 18 - 35 years. Current interventions are less likely to yield the return on investments in economic terms than if the focus were shifted to those risk factors, and at-risk groups, that together account for the high costs of alcohol-related harms.
Despite its limitations, this study provides a comprehensive assessment of the cost of alcohol-related harms. It clearly shows that harm-related consumption of alcohol has economic effects that extend beyond many of the factors often used to justify the economic benefits of retaining the existing legislation that governs the alcohol market. The unavailability of essential costing data results in an underestimate of the true economic, social and health costs of alcohol in SA. Providing a more accurate assessment of these costs will require a cross-sectoral commitment to funding and research aimed at providing the kinds of data absent from this study.
Conclusion and recommendations
Much more can be done to mitigate the costs of harmful alcohol use and its impact on economic growth. Given the prevalence and magnitude of drinking in SA, it is not surprising that companies on the supply side of the alcohol market are powerful and influential. Their economic influence means that the existing frameworks that guide the regulation and distribution of alcohol are founded on claims about maximising their contributions to the local economy. Industry claims must always be assessed against the economic, social and health costs associated with the end use of their products. Furthermore, consideration should be given to who is benefiting from the industry and who is paying its costs.
Regulatory and policy interventions have the potential to substantially curtail the costs of harmful alcohol use, and in doing so make a direct contribution to the well-being of the average SA citizen, and to the economy. However, such regulation will only be effective if informed by good evidence provided by ongoing economic, social and health research into the effects of alcohol.
Acknowledgements
The current study formed part of a larger costing project[36] commissioned by the National Liquor Authority, a division of- the National Department of Trade and Industry of SA, to assist future development of evidence-based policy and law.
References
1. Parry CDH, Myers B, Thiede M. The case for an increased tax on alcohol in South Africa. S Afr J Econ 2003;71(2):265-281. 'http://dx.doi.org/10.1111/j.1813-6982.2003.tb01308.x1 [ Links ]
2. Single E, Robson L, Xie X, Rehm J. The economic costs of alcohol, tobacco and illicit drugs in Canada, 1992. Addiction 1998;93(7):991-1006. 'http://dx.doi.org/10.1080/096521498351701 [ Links ]
3. Budlender D. National and Provincial Government Spending and Revenue Related to Alcohol Abuse. Johannesburg: Soul City Development Institute, 2009. [ Links ]
4. A & T Consulting. Industry Study: The South African Liquor Industry. Pretoria: Department of Trade and Industry, 2005. http://www.restaurant.org.za/downloads/SALiquorIndustryJune05.pdf (accessed 10 December 2013). [ Links ]
5. Moller L, Matic S. Best Practice in Estimating the Costs of Alcohol: Recommendations for Future Studies. Copenhagen: WHO Regional Office for Europe, 2010. [ Links ]
6. Collins D, Lapsley H, Brochu S, et al. International Guidelines for the Estimation of the Avoidable Costs of Substance Abuse. Ottawa: Health Canada, 2006. [ Links ]
7. Jones L, Bates G, McCoy E, et al. The Economic and Social Costs of Alcohol-related Harm in Leeds 2008-09. Liverpool: Liverpool John Moores University, 2010. [ Links ]
8. Norman R, Bradshaw D, Schneider M, et al. Estimating the burden of disease attributable to interpersonal violence in South Africa in 2000. S Afr Med J 2007;97(8):653-656. [ Links ]
9. Schneider M, Norman R, Parry C, Bradshaw D, Plüddemann A. Estimating the burden of disease attributable to alcohol use in South Africa in 2000. S Afr Med J 2007;97(8):664-672. [ Links ]
10. Bradshaw D, Groenewald P, Laubscher R, et al. Initial Burden of Disease Estimates for South Africa, 2000. Parow, Cape Town: Burden of Disease Research Unit, Medical Research Council of South Africa, 2003. [ Links ]
11. Parry C, Rehm J, Poznyak V, Room R Alcohol and infectious diseases: An overlooked causal linkage: Addiction 2009;104(3):331-332. 'http://dx.doi.org/10.1111/j.1360-0443.2008.02500.x1 [ Links ]
12. Rehm J, Anderson P, Kanteres F, Parry CD, Samokhvalov AV Patra J. Alcohol, Social Development and Infectious Disease. Stockholm: Swedish Ministry of Health and Social Affairs, 2009. Report No. 978-1-77052-444-6. [ Links ]
13. Rehm J, Kehoe T, Rehm M, Patra J. Alcohol Consumption and Related Harm in WHO Africa Region in 2004. Toronto: Centre for Addiction and Mental Health, 2009. [ Links ]
14. Single E, Collins D, Easton B, et al. International Guidelines for Estimating the Costs of Substance Abuse. Geneva: World Health Organization, 2003. [ Links ]
15. Marszalek J, De Villiers PJT. Morbidity profile of admissions to GF Jooste Hospital, Manenberg, Cape Town. S Afr Fam Pract 2006;48(6):15a-e. [ Links ]
16. Bowman B. Towards a South African injury costing model: A review of the literature for the development of a process path. African Safety Promotion 2002;1(1):55-64. [ Links ]
17. Bowman B, Stevens G. Injury costing in South Africa: The state of the sector. In: Suffla S, Van Niekerk A, Duncan N. Crime, Violence and Injury Prevention in South Africa: Developments and Challenges. Cape Town: MRC Press, 2004:170-183. [ Links ]
18. World Health Organization Statistical Information System (WHOSIS). 2012. http://www.who.int/whosis/en/ (accessed 5 January 2012). [ Links ]
19. Anderson P, Baumberg B. Alcohol in Europe: A Public Health Perspective. London: Institute of Alcohol Studies, 2006. http://ec.europa.eu/health-eu/news_alcoholineurope_en.htm (accessed 8 January 2013). [ Links ]
20. Plüddemann A, Dada S, Parry C, et al. Monitoring Alcohol & Drug Abuse Trends in South Africa (July 1996 - December 2008). Cape Town: Medical Research Council, 2009. [ Links ]
21. De Beer EJH, Van Niekerk EC. The Estimation of Unit Costs of Road Traffic Accidents in South Africa. Pretoria: National Department of Transport, 2004. [ Links ]
22. Miller TR, Lestina DC, Spicer RS. Highway crash costs in the United States by driver age, blood alcohol level, victim age, and restraint use. Accid Anal Prev 1998;30(2):137-150. 'http://dx.doi.org/10.1016/S0001-4575(97)00093-61 [ Links ]
23. Peer N, Matzopoulos R, Myers JE. The Number of Motor Vehicle Crash Deaths Attributable to Alcohol-impaired Driving and its Cost to the Economy Between 2002 and 2006 in South Africa. Cape Town: University of Cape Town, 2009. [ Links ]
24. Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Alcohol and Global Health 1: Global burden of disease and injury and economic cost attributable to alcohol use and alcohol- use disorders. Lancet 2009;373(9682):2223-2233. 'http://dx.doi.org/10.1016/S0140-6736(09)60746-71 [ Links ]
25. Reddy S, James S, Sewpaul R, et al. The 2nd South African National Youth Risk Behaviour Survey: 2008. Cape Town: Medical Research Council, 2010. [ Links ]
26. Townsend L, Flisher AJ, King G. A systematic review of the relationship between high school dropout and substance use. Clin Child Fam Psychol Rev 2007;10(4):295-317. 'http://dx.doi.org/10.1007/s10567-007-0023-71 [ Links ]
27. French MT, Zarkin GA. Is moderate alcohol use related to wages? Evidence from four worksites. J Health Econ 1995;14(3):319-344. 'http://dx.doi.org/10.1016/0167-6296(95)90921-R1 [ Links ]
28. Berger MC, Leigh JP. The effect of alcohol use on wages. Appl Econ 1988;20(10):1343-1351. 'http://dx.doi.org/0.1080/000368488000001051 [ Links ]
29. Lye J, Hirschberg J. Alcohol consumption and human capital: A retrospective study of the literature. J Econ Surv 2010;24(2):309-338. 'http://dx.doi.org/10.1111/j.1467-6419.2009.00616.x1 [ Links ]
30. Miller TR. Variations between countries in values of statistical life. Journal of Transport, Economics and Policy 2000;34(2):169-188. http://www.jstor.org/stable/20053838'01 (accessed 10 December 2013). [ Links ]
31. South African Reserve Bank. Full Quarterly Bulletin, December 2013, No. 270. Pretoria: SARB, 2013. [ Links ]
32. Statistics South Africa. Mid-year Population Estimates 2010. Statistical Release P0302. Pretoria: Statistics South Africa, July 2010. [ Links ]
33. Lindhjem H, Navrud S, Braathen NA, Biausque V. Valuing mortality risk reductions from environmental, transport, and health policies: A global meta-analysis of stated preference studies. Risk Anal 2011;31(9):1381-1407. 'http://dx.doi.org/10.1111/j.1539-6924.2011.01694.x1 [ Links ]
34. Miller TR, Levy DT, Cohen MA, Cox KLC. Costs of alcohol and drug-involved crime. Prev Sci 2006;7(4):333-342. 'http://dx.doi.org/10.1007/s11121-006-0041-61 [ Links ]
35. Alda E, Cuesta J. A comprehensive estimation of costs of crime in South Africa and its implications for effective policy making. J Int Dev 2010;23(7):926-935. 'http://dx.doi.org/10.1002/jid.17211 [ Links ]
36. Truen S, Ramkolowan Y, Corrigall J, Matzopoulos R. Baseline Study of the Liquor Industry Including the Impact of the National Liquor Act 59 of 2003. Pretoria: Department of Trade and Industry, 2011. http://www.thedti.gov.za/business_regulation/docs/nla/other_pdfs/dna_economics_nla_act.pdf (accessed 10 December 2013). [ Links ]
37. Rosen SM, Miller TR, Simon M. The cost of alcohol in California. Alcohol Clin Exp Res 2008;32(11):1925-1936. 'http://dx.doi.org/10.1111/j.1530-0277.2008.00777.x1 [ Links ]
38. Nutt DJ, King LA, Phillips LD. Drug harms in the UK: A multicriteria decision analysis. Lancet 2010;376(9752):1558-1565. 'http://dx.doi.org/10.1016/S0140-6736(10)61462-61 [ Links ]
 Correspondence:
Correspondence:
R G Matzopoulos
richard.matzopoulos@mrc.ac.za
Accepted 28 November 2013.














