Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.104 no.2 Pretoria Fev. 2014
FORUM
CLINICAL PRACTICE
Strengthening pharmacovigilance in South Africa
U Mehta; M Dheda; G Steel; M Blockman; A Ntilivamunda; G Maartens, Y Pillay; K Cohen
Ushma Mehta is a consultant for the Division of Clinical Pharmacology, Department of Medicine, University of Cape Town (UCT), South Africa and an independent pharmacovigilance consultant based in Cape Town, South Africa. Mukesh Dheda is the national pharmacovigilance co-ordinator at the Pharmacovigilance Unit, Medicines Regulatory Authority, National Department of Health (NDoH), Pretoria, South Africa. Gavin Steel is Chief Director of Sector-wide Procurement with the Essential Drugs Programme, NDoH, Pretoria, South Africa. Marc Blockman is a senior specialist in the Division of Clinical Pharmacology, Department of Medicine, UCT, South Africa. Augustin Ntilivamunda is a medical officer with the World Health Organization, South Africa. Gary Maartens is Head of the Division of Clinical Pharmacology, Department of Medicine, UCT, South Africa. Yogan Pillay is Deputy Director General of HIV/AIDS, TB and Maternal and Child Health, NDoH, Pretoria, South Africa. Karen Cohen is a specialist in the Division of Clinical Pharmacology, Department of Medicine, UCT, South Africa
ABSTRACT
This report outlines findings and recommendations of a national pharmacovigilance workshop held in August 2012 in South Africa (SA). A survey of current pharmacovigilance activities, conducted in preparation for the meeting, identified multiple programmes collecting drug safety data in SA, with limited co-ordination at national level. The meeting resolved that existing pharmacovigilance programmes need to be strengthened and consolidated to ensure that important local safety issues are addressed, data can be pooled and compared and outputs shared more widely. Pharmacovigilance activities should inform treatment guidelines with the goal of improving patient care. A variety of pharmaco-epidemiological approaches should be employed, including nesting drug safety studies within existing sentinel cohorts and the creation of a pregnancy exposure registry. The attendees agreed on key principles that will inform a national pharmacovigilance plan and compiled a list of priority pharmacovigilance issues facing public health programmes in SA.
Start where you are. Use what you have. Do what you can. - Arthur Ashe
Pharmacovigilance is the science of adverse drug reactions (ADRs) and drug-related problems: their detection, assessment, management and prevention.[1] In 1992, South Africa (SA) was the first country in Africa to become a member of the World Health Organization (WHO) International Drug Monitoring Programme which co-ordinates international pharmacovigilance activities. Traditionally, pharmacovigilance activities were limited to spontaneous reporting of ADRs, which has been the mainstay of regulatory pharmacovigilance activities for many years. More recently, pharmacovigilance encompasses a growing range of quantitative and qualitative methods, which have become an integral part of the process for registration of medicines. Pharmacovigilance is recognised as an important component of monitoring and evaluation of public health programmes and medical institutions.[1]
Pharmacovigilance is a responsibility shared with the medicine regulatory authority, public health programmes, the pharmaceutical industry, and the Essential Drugs Programme (EDP). As pharmacovigilance initiatives evolve and expand in SA, a national consolidated plan that integrates programmatic, regulatory and clinical/institutional pharmacovigilance is needed. This plan would strive to ensure that pharmacovigilance systems prioritise key national medicine safety concerns; are methodologically robust and ethical; and communicate their data and findings effectively to ensure that the data are used to inform policy and improve patient care.
In August 2012, key stakeholders attended a national pharmacovigilance workshop hosted by the National Department of Health (NDoH) in collaboration with the University of Cape Town (UCT) supported by a grant from the US Centers for Disease Control- and Prevention (CDC). The workshop aimed to obtain an overview of non-regulatory pharmacovigilance activities being conducted in the public sector, and to identify key strengths, shortcomings, and opportunities for strengthening and unifying these activities into a coherent national pharmacovigilance plan.
Status of pharmacovigilance activities in SA
Before the workshop, we conducted a survey of non-regulatory pharmacovigilance programmes run by government, academic and other non-governmental institutions. We identified pharmacovigilance systems for the immunisation, HIV and tuberculosis (TB) programmes (four provincial systems and two co-ordinated by the NDoH) and for specific clinical specialties (paediatric HIV and dermatology). Surveillance methods included targeted spontaneous reporting (TSR) for specific drugs or patient groups, active surveillance for adverse reactions nested within existing cohort studies (two provincial systems) and cohort event monitoring (CEM) (two systems for patients receiving antiretroviral (ARV) medicines).
While these pharmacovigilance programmes generate potentially useful information, there is little collaboration between programmes, even where the same approach, medicines and patient populations were targeted. Case definitions for solicited adverse events and pharmacovigilance terms differ so that data could not be meaningfully pooled. Case record forms, criteria for reporting and the purposes of reporting differ between similar TSR systems. The two CEM projects initiated for ARVs in two provinces were suspended owing to resource constraints. An active hospital surveillance system at one tertiary hospital contributes data to a multicentre, international dermatology registry but there were no links between this system and provincial and national custodians of pharmacovigilance. Generally, outputs of existing systems are limited and were rarely used in policy decision-making. The TSR programmes for HIV and TB medicines in four provinces provide some feedback to reporters by means of annual newsletters, periodic multidisciplinary case audits or telephonic feedback. Improved analysis and communication of the data was recognised as an important area for strengthening in all cases. The survey highlighted the need for greater collaboration between the pharmacovigilance programmes so that expertise, experience and resources can be shared and data pooled and compared.
There was acknowledgement that other pharmaco-epidemiological approaches, e.g. nesting drug safety studies within existing sentinel cohorts and case control studies, have improved our understanding of medicines safety in SA. Local studies exploring safety of stavudine, which contributed to changes in policy, highlighted the value of such investigator-initiated research.[2-8] Cohort studies are an important source of pharmacovigilance data as they determine ADR incidence, which is needed to inform policy.
National pharmacovigilance plan
The meeting agreed that a national pharmacovigilance plan should be underpinned by five key principles:
- Regulatory, programmatic and institutional pharmacovigilance (see box below) should be incorporated into a cohesive national system.To ensure complementarity between different pharmacovigilance programmes, including those of the Medicines Regulatory Authority (MRA), lines of data and communication flow must be clearly defined. An organogram that defines the roles, responsibilities of the MRA and pharmaceutical industry, the EDP and public health programmes and their relationship to each other is needed.
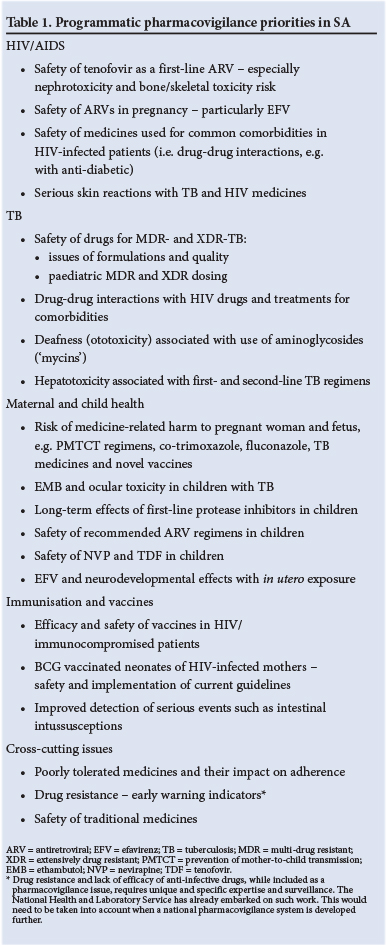
- The national pharmacovigilance system should contribute to treatment policy decision-making and improved patient care. The pharmacovigilance system should prioritise safety issues that significantly impact on the health of South Africans. The meeting identified priority pharmacovigilance issues facing the HIV, TB, maternal and child health and immunisation programmes (Table 1). Existing SA pharmacovigilance programmes should be reviewed in terms of their performance in meeting their objectives, the scientific validity of the approach adopted and whether outputs address priority safety concerns. There was agreement that in the short-to-medium term pharmacovigilance surveillance should comprise the following approaches:
- spontaneous reporting for all medicines co-ordinated by the MRA
- TSR for public health programmes including HIV, TB and immunisation
- Regulatory pharmacovigilance focuses on developing a greater understanding of the risk-benefit profile of all registered medicines, the focus being on assessing the merit of the products on the market.
- Public health pharmacovigilance programmes target their activities towards minimising the risk of preventable harms associated with recommended treatments or regimens and maintaining public trust.
- Institutional/clinical pharmacovigilance aims to minimise medicines-related morbidity and mortality and the costs incurred in managing ADRs at clinical institutions (i.e. clinics and hospitals).
- improved collection of medicines safety data within existing cohorts (e.g. HIV cohorts)
- a pregnancy exposure registry, which will be a sentinel surveillance system for medicines used in pregnancy.
- The national pharmacovigilance system should incorporate both passive and active surveillance methods and should build on what already exists and has shown success. Both active and passive surveillance systems provide important medicines safety information. Policy-makers and stakeholders need to appreciate the strengths and limitations of each approach. Passive surveillance systems for spontaneous reports of ADRs are useful in detecting signals of unknown or poorly understood ADRs and are important for improving patient care at institutional level. However, they cannot provide epidemiological information, such as incidence of ADRs, or compare the relative safety of two medicines, which is essential for changing public health policy. Active surveillance within sentinel cohorts can determine the incidence and risk factors for specific ADRs. The CEM system requires that a cohort of at least 20 000 patients per treatment regimen be monitored over time.[9] There was general agreement that this costly and labour-intensive approach was not appropriate for the SA context. Instead, drug safety analyses should be nested within existing cohorts and cohort collaborations.
- Investment in capacity building and training in pharmacovigilance and pharmaco-epidemiology is critical to the success of the system. The NDoH, training institutions and partners need to support clinical staff by providing drug information support and training. Training of relevant stakeholders (e.g. EDP, pharmacy and therapeutic committees, disease programme managers) in the analysis, interpretation and communication of pharmacovigilance data is a priority. Academic institutions should be supported to develop postgraduate courses in pharmacovigilance and pharmaco-epidemiology.
- Feedback and communication to stakeholders (from community to government) must be prioritised to ensure success and sustainability of the pharmacovigilance programme. The survey identified poor communication and feedback as major weaknesses of the existing pharmacovigilance systems. Platforms, such as a national pharmacovigilance website, that facilitate information sharing between researchers, policy-makers, pharmaceutical industry, clinicians, patients and the public should be created and supported. The NDoH requires a robust data management system that can respond to the requirements of the national pharmacovigilance plan. The data management system should allow for routine analysis and reporting of data, including feedback to reporters and other relevant stakeholders.
Progress to date
The NDoH has already embarked on addressing the recommendations that arose from the workshop and has appointed a co-ordinator to facilitate implementation.
A national decentralised TSR system for HIV and TB is being established and is at various phases of implementation in six provinces. Spontaneous reports are reviewed by a sub-district multidisciplinary health team to identify important reporting trends and preventable factors, including medication errors and system errors. It is hoped that this non-punitive multidisciplinary approach to reviewing ADR cases at institutional level will encourage spontaneous reporting, support clinical governance and improved management of patients with ADRs.
The NDoH is implementing a national pregnancy exposure registry and birth defect surveillance programme at sentinel sites throughout the country to assess the safety of medicines commonly- used in pregnancy. Instances of serious ADRs in pregnant woman and the incidence of adverse birth outcomes such as stillbirth, low birth weight, and congenital anomalies will be determined.[10] The first site is currently being initiated in KwaZulu-Natal province.
Way forward
The relationship between the MRA, public health programmes and clinical services management within the NDoH needs to be clarified and operationalised. A key recommendation of the workshop was the creation of a national pharmacovigilance policy that will underpin the SA pharmacovigilance system. Such a policy would set the stage for an ethical and scientifically sound national pharmacovigilance programme that could significantly benefit public health and patient care.
Acknowledgements
The authors are grateful to the attendees of the meeting who contributed to the discussions and recommendations that are reflected in this report. The participants represented the following organisations: KwaZulu-Natal Department of Health, Management Sciences for Health, Medicines Control Council, MEDUNSA, Mpumalanga Department of Health, NDoH, Right to Care, the Joint United Nations Programme on HIV/AIDS, the CDC, US Agency for International Development, UCT, the University of KwaZulu-Natal, the University of the Free State, VP Health Systems, Wits Reproductive Health and HIV Research Institute, and the WHO. The national survey and meeting was jointly funded by the office of the Deputy Director
General: HIV/AIDS, TB and Maternal and Child Health of the NDoH and by the US President's Emergency Plan for AIDS Relief through the CDC under the terms of the Cooperative Agreement #GH000371. The content of the report is solely the responsibility of the authors and does not necessarily represent the official views of the CDC.
1. WHO Collaborating Centre for International Drug Monitoring. The Importance of Pharmacovigilance. UK: WHO, 2002. http://apps.who.int/medicinedocs/en/d/Js4893e/ (accessed 3 December 2013). [ Links ]
2. Bolhaar MG, Karstaedt AS. A high incidence of lactic acidosis and symptomatic hyperlactatemia in women receiving highly active antiretroviral therapy in Soweto, South Africa. Clin Infect Dis 2007;45(2):254-260. [http://dx.doi.org/10.1086/518976] [ Links ]
3. Geddes R, Knight S, Moosa MYS, Reddi A, Uebel K, Sunpath H. A high incidence of nucleoside reverse transcriptase inhibitor (NRTI)-induced lactic acidosis in HIV-infected patients in a South African context. S Afr Med J 2006;96(8):722-724. [ Links ]
4. Boulle A, Orrell C, Kaplan R, et al. Substitutions due to antiretroviral toxicity or contraindication in the first 3 years of antiretroviral therapy in a large South African cohort. Antivir Ther 2007;12(5):753-760. [ Links ]
5. Westreich DJ, Sanne I, Maskew M, et al. Tuberculosis treatment and risk of stavudine substitution in first-line antiretroviral therapy. Clin Infect Dis 2009;48(11):1617-1623. [http://dx.doi.org/10.1086/598977; [ Links ]
6. Perez EH, Dawood H, Chetty U, Esterhuizen TM, Bizaare M. Validation of the Accutrend lactate meter for hyperlactatemia screening during antiretroviral therapy in a resource-poor setting. Int J Infect Dis 2008;12(5):553-556. [http://dx.doi.org/10.1016/jjjid.2008.03.007] [ Links ]
7. Maskew M, Westreich D, Fox MP, Maotoe T, Sanne IM. Effectiveness and safety of 30 mg versus 40 mg stavudine regimens: A cohort study among HIV-infected adults initiating HAART in South Africa. J Int AIDS Soc 2012;15:13. [http://dx.doi.org/10.1186/1758-2652-15-13] [ Links ]
8. Schutz C, Boulle A, Stead D, Rebe, Osler M, Meintjies G. Reduced referral and case fatality rates for severe symptomatic hyperlactataemia in a South African public sector antiretroviral programme: A retrospective observational study. AIDS Res Ther 2010;7:13. [http://dx.doi.org/10.1186/1742-6405-7-13] [ Links ]
9. World Health Organization. A Practical Handbook on the Pharmacovigilance of Antiretroviral Medicines. Geneva: WHO, 2009. http://www.who.int/medicines/areas/quality_safety/safety_efficacy/ HIVhandbook.pdf (accessed 3 December 2013). [ Links ]
10. Mehta U, Clerk C, Allen E, et al. Protocol for a drugs exposure pregnancy registry for implementation in resource limited settings. BMC Pregnancy Childbirth 2012;12:89. [http://dx.doi.org/10.1186/1471-2393-12-89] Accepted 17 September 2013. [ Links ]
 Correspondence:
Correspondence:
K Cohen
karen.cohen@uct.ac.za














