Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.104 no.1 Pretoria ene. 2014
RESEARCH
Patient-initiated sexual partner notification in Botswana and time taken for sexual contacts to report for treatment
T A TafumaI; B C NtwayagaeII; C K MoalafhiIII; J M BolebantsweIV
IMB ChB, MPH. Department of HIV/AIDS Prevention and Care, STI/HIV Control Programme, Ministry of Health, Gaborone, Botswana
IIRN, RM, BSc. Department of HIV/AIDS Prevention and Care, STI/HIV Control Programme, Ministry of Health, Gaborone, Botswana
IIIRN, RM, BCur Ed et Adm. Department of HIV/AIDS Prevention and Care, STI/HIV Control Programme, Ministry of Health, Gaborone, Botswana
IVRN, FNP. Department of HIV/AIDS Prevention and Care, STI/HIV Control Programme, Ministry of Health, Gaborone, Botswana
ABSTRACT
BACKGROUND: Sexually transmitted infections (STIs) are an important public health concern because of their impact on reproductive and other health problems. Initiating treatment at an early stage for both index patients and their partners reduces the risk of reinfections and prevents serious short- or long-term complications for the infected individuals. Sexual partner tracing is one of the means available for reaching and treating asymptomatic sexual partners of index patients.
OBJECTIVES: To determine the time taken by sexual partners to report to a health facility after they had been notified by the index patient, and the distribution of STI syndromes among the treated index patients who had their sexual partners treated.
METHODS: All available contact slips of the treated sexual partners from 19 health districts in Botswana were reviewed. The study period was July 2010 to June 2011 inclusive.
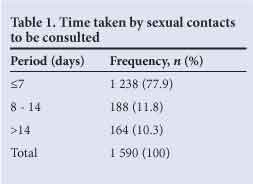
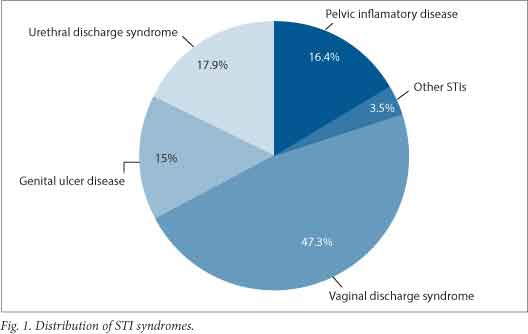
RESULTS: The partner notification slips showed that 77.9% (1 238/1 590) of sexual contacts sought medical attention at government health facilities within 7 days of treating the index patient. Records showed that 47.3% (752/1590) of the index patients were treated for vaginal discharge syndrome.
CONCLUSION: A high proportion of sexual contacts were treated within 7 days of treating the index patient. Considering this short period, we conclude that Botswana's recommended 30-day period for consulting sexual partners needs to be revised downwards, so as to reduce the chances of reinfections, complications and transmission of STIs in the community.
Sexually transmitted infections (STIs) are an important public health concern because of their negative impact on reproductive and other health problems.[1] Sexual partner tracing (SPT), also referred to as partner notification (PN), is the process by which the sexual contacts of a patient treated for a STI, referred to as the index patient (IP), are informed of their risk of an STI and seek medical examination, treatment, care and support at a health facility.[2-4] Prevention and control of STIs, primarily treatable ones such as gonorrhea and chlamydia, rely heavily on the timely identification, diagnosis and treatment of infected individuals.[1,5] In most developing countries these conditions are treated syndromically. SPT is a very important component of comprehensive STI management and control,[5-7] although the US Centers for Disease Control and Prevention's (CDC) Sexually Transmitted Disease Treatment Guidelines note that it's uncertain to what extent PN effectively decreases the prevalence and incidence of these infections.[3] However, SPT is the only means available for reaching and treating asymptomatic sexual partners of IPs.[6] It is important to note that sexual contacts have a high likelihood of similar STIs, and that therefore treating them empirically provides a significant opportunity to reduce the risk of reinfection and transmission in the community.[5] This becomes very relevent to developing countries, where the syndromic approach is still being used.
Initiating treatment at an early stage for both contacts and IPs reduces the risk of reinfections and prevents serious short- or longterm complications for the infected individuals.[2,7] It is, however, difficult to select the infected individuals for whom the syndromic approach should be used. In developing countries, the patient-oriented method is the most-used model, despite evidence suggesting that only around half of sexual contacts informed in this way receive treatment.[5,8] Among other challenges, the stigma and discrimination attached to STIs makes partner notification difficult.[9] As a result, most sexual contacts do not seek medical help despite being informed by IPs, and in some cases IPs will be afraid to notify their contacts.[7] Furthermore, there are difficulties in identifying and contacting non-regular contacts,[5] especially for commercial sex workers.
There are 3 main approaches to PN for STIs: (i) the provider-oriented notification method, which uses third parties who specialise in contact tracing (public health personnel); (ii) patient-oriented notification methods that rely on IPs to notify their partners, with or without the medication to actually treat the partner(s) for the putative infection or infectious exposure; and (iii) a contractual approach that enlists IPs to notify their partners, with an understanding that healthcare personnel will notify those partners who do not present for treatment within a given time.[2,7] Between the 3, the provider-oriented method was found to be the most effective in reaching partners and getting them treated.[7] However, this is only practical in developed countries[7] due to its associated cost. In developing countries, the World Health Organization (WHO) recommends patient-oriented partner notification.[2,4,7]
Botswana provides syndromic STI services in all health facilities and recommends the patient-oriented approach, without the IP delivering medications to the partner.[4] STIs are notifiable conditions in this country and approximately 70 000 and 80 000 new cases were treated in 2010 and 2011 respectively.[12] The patient-oriented approach is relatively cheap and easier to implement.[9]
Even though developing countries rely on patient referral, the effectiveness of this approach has not been adequately investigated.[1,3] Furthermore, most studies have not documented the time taken by contacts to report to health facilities after the IP notifies them. Botswana considers contact notification to be successful when contacts are notified within 30 days,[4] but on an anecdotal basis, the evidence to support this recommendation is not clear. The national contact notification rate has been in the range of 8% - 16%.[4] This study aims to establish the time taken by sexual partners to report to a health facility following notification by the IP, and to determine the distribution of STI syndromes among those IPs whose sexual contacts were seen at a government health facility.
Methods
This was a retrospective descriptive study that analysed the contact slips collected from 19 government health districts (each with approximately 15 health facilities) in Botswana between July 2010 and end of June 2011. These contact slips were collected when consulting sexual contacts who had been notified by the relevant IP. The pooled slips from each government health facility within a district were sent to the Community Health Nurse at the District Health Management Team offices. At the end of each month, the slips were taken to the STI Control Programme at the Ministry of Health head office (STI Control Programme).
All contact slips received within the study period were considered for the study as long as they contained the dates of treatment of both the IP and the sexual contact, and a clear diagnosis of the IP. Those missing this information were excluded. The time that contacts took to report to a health facility was calculated as number of days from the date on which healthworkers consulted the IP to the date on which they consulted the contact. The authors formulated 3 categories for the time of presentation: i) within 7 days; ii) 8 to 14 days and iii) >14 days. The patients' conditions were categorised according to the common syndromes treated in the country.
The data were captured on an Excel spreadsheet and Epi-Info 6.3 version was used for descriptive statistical analyses. Ethics approval was obtained from the Health Research Development Division of the Ministry of Health (Botswana).
Results
During the study period, a total of 3048 contact slips were received and recorded, of which 1590 slips met all the inclusion criteria. Out of these, 77.9% (1238) showed that sexual contacts sought medical attention within 7 days and 10.3% (164) after 2 weeks (Table 1). Vaginal discharge syndrome was recorded on 47.3% (752) of the contact slips and other STIs on 3.5% (55/1 590) (Fig. 1).
Discussion
This study shows that the majority of sexual contacts sought medical attention within a week of the IP receiving treatment. Healthcare workers in Botswana are trained in sexual partner management during STI syndromic management training. It has been observed that to discuss an STI diagnosis, individuals need to have confidence in themselves and in their relationship.[10] As such, the quality and appropriateness of the counselling that IPs receive increases the success of contact notification by eliminating the fear and stigma associated with STIs.[7] Such counselling should be encouraged in both private and public health facilities.
Botswana also has a highly mobile population, which might have contributed to some contacts being consulted more than 7 days after seeing the IP. It is recommended that all sexual partners within the past 1 to 3 months be contacted and referred for STI treatment,[3] but SPT is less effective over this timeframe as they might have already spread their infections or developed complications. However, this should not deter healthcare workers from practising SPT.
The most-treated condition in the study was vaginal discharge syndrome (VDS). Although this is not necessarily related to an STI, most women who present with the symptoms are labelled as having an STI. There is anecdotal evidence that clinicians perform risk assessment poorly in patients presenting with VDS. In addition, physical examination is often missed due to lack of appropriate equipment (e.g. examination lamps and speculums), leading clinicians to base their diagnosis on the patient's symptoms. As a result, a significant number of women with other non-STI conditions end up being treated for STIs that they probably do not have. However, to reduce this massive overtreatment would require specific diagnostic tests.[11] Given the higher costs associated with laboratory investigations, developing countries such as Botswana will be forced to continue using the syndromic approach.
Study limitations
This study used data which had been used for routine reporting. As such, some of the slips might have been missing or incomplete at the time of analysis, leading to selection bias. Secondly, the files were not research specific, thus limiting the strength of the study. Significant confounding variables such as stable relationships and presence of symptoms among the contacts who presented to the facilities within a week were not considered because there was no provision for them in the data-collecting tool. Nevertheless, as the first of its kind in Botswana, this study has provided important information that can be used by clinicians and STI control programs.
Conclusion
Since the majority of contacts reported to health facilities within a short period (1 week), we conclude that the consultation period (30 days) of sexual contacts in Botswana needs to be shortened. This will reduce the chances of reinfections, complications and transmission of STIs in the community. The study recommends the revision of VDS algorithms. Those in current use contribute to the overdiagnosis of STIs, which might expose women, or their partners, to unnecessary risk of violence, psychological stress and overtreatment.
Acknowledgements. We acknowledge the support of Dr L Chonzi, who assisted with the review of this manuscript. Ms P T Mogolwane assisted with the data entry.
References
1. Wilson TE, Hogben M, Malka ES, et al. A randomized controlled trial for reducing risks for sexually transmitted infections through enhanced patient-based partner notification. Am J Public Health 2009;99(S1):104-110. [http://dx.doi.org/10.2105/AJPH.2007.112128] [ Links ]
2. World Health Organisation. Global Strategy for the Prevention and Control of Sexually Transmitted Infections: 2006 - 2015. Geneva: WHO, 2007. http://whqlibdoc.who.int/hq/2006/WHO_RHR_06.10_eng.pdf (accessed 3 September 2013). [ Links ]
3. Workowski K, Berman S. Sexually Transmitted Diseases Treatment Guidelines. Recommendations and Reports. Atlanta: Centers for Disease Control and Prevention, 2010. http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5912a1.htm (accessed 3 September 2013). [ Links ]
4. Botswana Ministry of Health. Botswana National Sexual Partner Tracing Guide. Gabarone: MoH, 2012. [ Links ]
5. Khan A, Fortenberry JD, Juliar BE, et al. The prevalence of chlamydia, gonorrhea, and trichomonas in sexual partnerships: Implications for partner notification and treatment. Sex Transm Dis 2005;32(4):260-264. [http://dx.doi.org/10.1097/01.olq.0000161089.53411.cb] [ Links ]
6. Turner K, Adams E, Grant A, et al. Costs and cost effectiveness of different strategies for chlamydia screening and partner notification: An economic and mathematical modelling study. BMJ 2010;341:c7250. [http://dx.doi.org/10.1136/bmj.c7250] [ Links ]
7. Alam N, Chamot E,Vermund SH, Streatfield K, Kristensen S. Partner notification for sexually transmitted infections in developing countries: A systematic review. BMC Public Health 2010;10:19. [http://dx.doi.org/10.1186/1471-2458-10-19] [ Links ]
8. Shackleton T, Sutcliffe L, Estcourt C. Is Accelerated Partner Therapy partner notification for sexually transmissible infections acceptable and feasible in general practice? Sexual Health 2011;8(1):17-22. [http://dx.doi.org/10.1071/SH10031] [ Links ]
9. Trelle S, Shang A, Nartey L, Cassell JA, Low N. Improved effectiveness of partner notification for patients with sexually transmitted infections: Systematic review. BMJ 2007;334(7589):354-357. [http://dx.doi.org/10.1136/bmj.39079.460741.7C] [ Links ]
10. Gursahaney PR, Jeong K, Dixon BW, Wiesenfeld HC. Partner notification of sexually transmitted diseases: Practices and preferences. Sexually Transm Dis 2011;38(9):821-827. [http://dx.doi.org/10.1097/OLQ.0b013e31821c390b] [ Links ]
11. Romoren M, Sundby J, Velauthapillai M, et al. Chlamydia and gonorrhoea in pregnant Batswana women: Time to discard the syndromic approach? BMC Infectious Diseases 2007;7:27. [http://dx.doi.org/10.1186/1471-2334-7-27] [ Links ]
12. Botswana Ministry of Health. Integrated Disease Surveillance and Response Monthly Reports. Gabarone: MoH, 2012. [ Links ]
 Correspondence:
Correspondence:
T A Tafuma
(tauadd@gmail.com)
Accepted 14 May 2013














