Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.104 no.1 Pretoria ene. 2014
RESEARCH
Diabetes mellitus in HIV-infected patients receiving antiretroviral therapy
D MoyoI; G TanthumaII; O MushishaIII; G KwadibaIV; F ChikuseV; M S Cary,VI, VII; A P Steenhoff,VIII-XII; M J A Reid,XIII, XIV, XV
IBPharm (Hons), PGDPH. Institute for Health Sciences, Gaborone, Botswana
IIBSc, PGDE, MA. Institute for Health Sciences, Gaborone, Botswana
IIIBPharm (Hons). Institute for Health Sciences, Gaborone, Botswana
IVPharmD. Institute for Health Sciences, Gaborone, Botswana
VHBMLS. Institute for Health Sciences, Gaborone, Botswana
VIPhD. Center for Clinical Epidemiology and Biostatistics, University of Pennsylvania, Philadelphia, USA
VIIPhD. Perelman School of Medicine, University of Pennsylvania, Philadelphia, USA
VIIIMB BCh, DCH (UK), FCPaed (SA), FAAP. Perelman School of Medicine, University of Pennsylvania, Philadelphia, USA
IXMB BCh, DCH (UK), FCPaed (SA), FAAP. Botswana/UPenn Partnership, Gaborone, Botswana
XMB BCh, DCH (UK), FCPaed (SA), FAAP.Center for AIDS Research, University of Pennsylvania, Philadelphia, USA
XIMB BCh, DCH (UK), FCPaed (SA), FAAP. Department of Pediatrics, Division of Infectious Diseases, The Children's Hospital of Philadelphia, USA
XIIMB BCh, DCH (UK), FCPaed (SA), FAAP. School of Medicine, University of Botswana, Gaborone, Botswana
XIIIMD, MA, MRCP (UK) Perelman School of Medicine, University of Pennsylvania, Philadelphia, USA
XIVMD, MA, MRCP (UK) Botswana/UPenn Partnership, Gaborone, Botswana
XVMD, MA, MRCP (UK) School of Medicine, University of Botswana, Gaborone, Botswana
ABSTRACT
BACKGROUND: There is little in the literature on HIV and diabetes mellitus (DM) in sub-Saharan Africa.
OBJECTIVE: To assess the characteristics of HIV and DM in patients receiving antiretroviral therapy (ART) in Botswana.
METHODS: A retrospective case-control study was conducted at 4 sites. Each HIV-infected patient with DM (n=48) was matched with 2 HIV-infected controls (n=108) by age (±2 years) and sex. Primary analysis was conditional logistic regression to estimate univariate odds and 95% confidence intervals (CIs) for each characteristic.
RESULTS: There was no significant association between co-morbid diseases, tuberculosis, hypertension or cancer and risk of diabetes. DM patients were more likely to have higher pre-ART weight (odds ratio (OR) 1.09; 95% CI 1.04 - 1.14). HIV-infected adults >70 kg were significantly more likely to have DM (OR 12.30; 95% CI 1.40 - 107.98). Participants receiving efavirenz (OR 4.58; 95% CI 1.44 - 14.57) or protease inhibitor therapy (OR 20.7; 95% CI 1.79 - 240.02) were more likely to have DM. Neither mean pre-ART CD4 cell count (OR 1.0; 95% CI 0.99 - 1.01) nor pre-ART viral load >100 000 copies/ml (OR 0.71; 95% CI 0.21 - 2.43) were associated with a significant risk of diabetes.
CONCLUSIONS: These findings suggest a complex interrelation among traditional host factors and treatment-related metabolic changes in the pathogenesis of DM inpatients receiving ART. Notably, pre-ART weight, particularly if >70 kg, is associated with the diagnosis of diabetes in HIV-infected patients in Botswana.
The unequivocal success of antiretroviral therapy (ART) in controlling HIV replication and restoring immunity has been tempered by the recognition that metabolic diseases, such as diabetes mellitus (DM), are increasing in incidence among people living with HIV. Studies from high-income countries have reported that the incidence of diabetes in HIV-infected adults receiving ART is between 1% and 10%.[1] Conventional risk factors, such as obesity, ageing and male sex, are important determinants of diabetes.[2,3] However, specific antiretrovirals (ARVs)[3] and ARV-related weight gain and lipodystrophy[4,5] are recognised risk factors. High pre-ART viral loads and low baseline CD4+ counts may also increase the risk of insulin resistance and accelerate the pathogenesis of diabetes.[5]
The association between HIV infection and DM in sub-Saharan Africa (SSA) has not been well documented.[6,7] While diabetes incidence is increasing in the general population in southern Africa,[8,9] there is very little describing the incidence and determinants of diabetes among HIV-infected adults in this region.
Objective
To assess the characteristics associated with HIV and DM at the time of ART initiation in patients in Botswana.
Methods
A retrospective case-control study was conducted at 4 sites between February 2011 and November 2012. DM was defined according to the World Health Organization criteria.[10] Cases were identified by searching the medical records of patients who had accessed care at diabetes clinics at 2 semi-urban facilities (in Orapa and Kanye) and 2 urban facilities (in Gaborone and Francistown). Patients who developed diabetes receiving ART or who had pre-existing DM before initiating ART were included if they had either 5 consecutive CD4+ count measurements post-ART initiation or had been taking ART for at least 2 years. Those with confirmed insulin-dependent type 1 diabetes were excluded. At each site, controls were selected by a systematic process - every 20th file in the adult HIV clinic registry was retrieved.
Two controls per case were matched preferentially for age (±2 years) and sex. The medical records of all cases and controls were reviewed to extract demographic and clinical data including weight, ART regimen, ART adherence, co-morbid disease and baseline pre-ART CD4+ counts and viral loads.
Primary analysis using conditional logistic regression was employed to estimate univariate odds ratios (ORs) for each characteristic. Conditioning was based on 6 age-sex categories (gender within 3 age groups: <40, 40 - 49, and >50 years). Statistical analyses were performed using STATA software version 12. All tests of significance were 2-sided with p<0.05 designated as statistically significant.
This study was approved by the Institutional Review Boards of Princess Marina and Nyangabgwe Referral Hospitals and the Botswana Ministry of Health.
Results
In total, there were 48 cases (28 females, 20 males, age mean 46.4years ± standard deviation (SD) 9.9) and 108 controls (57 females, 51 males, age mean ±SD 43.6±8 years) who had initiated ART between January 2001 and February 2011. Data were available on prescribed anti-diabetic medications in the majority of cases (n=28): 21% (n=6) were receiving metformin, 60% (n=17) receiving metformin and glibenclamide and 18% (n=5) receiving an insulin-based regimen. Cases were matched with 108 HIV-infected control patients without DM. Table 1 summarises the baseline characteristics of both cohorts.
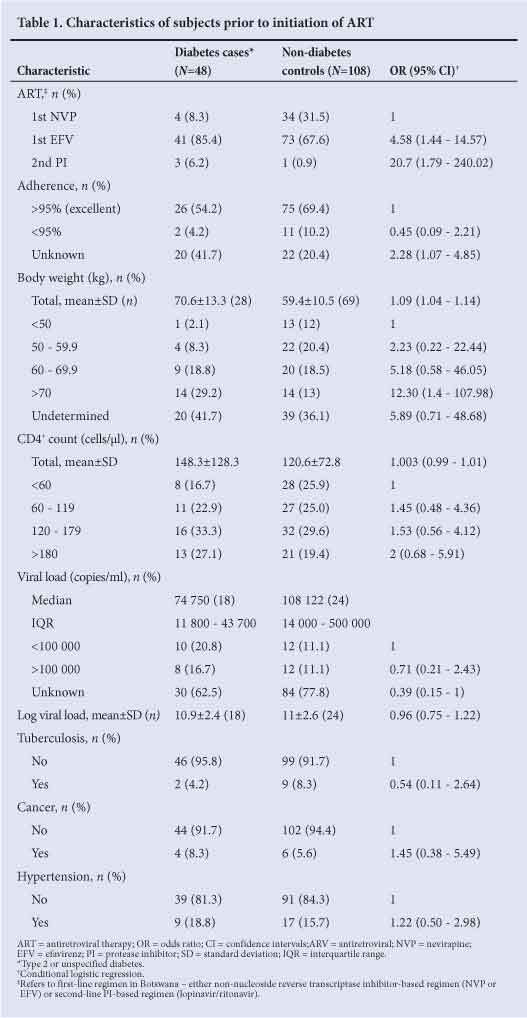
There was no significant association between the risk of having DM and either hypertension, active tuberculosis, cancer or reported adherence of <95%. However, undocumented adherence to ART was associated with an increased diabetes risk.
Weight at initiation of ART was significantly associated with increased risk of diabetes. Furthermore, the odds of DM with a pre-ART body weight of >70 kg was over 12 times that for a body weight of <50 kg. Univariate analysis demonstrated that both efavirenz (EFV) and protease inhibitor (PI) therapies were associated with increased odds of diabetes. While multivariate analysis suggested that weight was confounding the effect of the drug regimen, the sample size was too small to draw firm conclusions.
Mean CD4+ count at the time of ART initiation was not significantly higher in individuals with DM than controls. However, there was a non-significant trend towards increased risk of diabetes at a higher CD4+ count - patients with pre-ART CD4+ counts of >180 cells/µl were twice as likely to have DM compared with those with pre-ART CD4+ counts of <60 cells/µl. Baseline viral load >100 000 copies/ml was not associated with an increased risk of diabetes.
Discussion
In this case-control study, there were several notable findings. Firstly, diabetic patients with HIV had higher baseline weight compared with non-diabetics. Individuals with pre-ART weights of >70 kg had significantly higher risk of having diabetes, compared with those with baseline weights of <50 kg. This finding is consistent with established data that insulin resistance correlates with increased weight gain and obesity.[5] However, it is an important finding in this population since initiation of ART is itself associated with rapid weight gain. [2] Furthermore, the importance of targeted risk reduction strategies for overweight and obese individuals starting ART is highlighted.
Secondly, there were associations between both EFV and PI exposures and DM. While there is substantial literature indicating that ART plays a causative or permissive role in the pathogenesis of DM in HIV-infected patients, most research has demonstrated a link between DM and thymidine analogues[3] and PI therapy.[3,11] Our finding that EFV was associated with diabetes is especially notable given that EFV is part of first-line ART regimens across SSA because of its perceived lower toxicity compared with nevirapine. Researchers in Cape Town, South Africa found that EFV was significantly associated with impaired glucose tolerance even after controlling for body mass index and waist circumference.[7] Participants in that study had all been receiving EFV for at least 6 months at the time of enrolment, suggesting that EFV may accelerate insulin resistance. We speculate that the effect of EFV in our analysis was mediated by weight - those with a priori obesity receiving EFV were more likely to have DM. Unfortunately, our sample size was not large enough to prove conclusively that this was the case. More prospective research is warranted to elucidate how EFV influences diabetogenesis, especially in individuals with pre-ART weights >70 kg.
Thirdly, our analysis failed to demonstrate an association between HIV-specific factors and DM. Neither baseline CD4+ count, nor pre-ART viral load was associated with risk of diabetes. These findings are consistent with data from prospective analyses that have failed to demonstrate associations between CD4+ nadir or baseline viraemia and diabetes.[2,3] Nevertheless, more research is required to explore the relationship between immune reconstitution and insulin resistance.
Our analysis did not demonstrate any association between specific co-morbidities, tuberculosis, hypertension and malignancy, and diabetes. Data concerning co-morbidities such as dyslipidaemia, cardiovascular disease or hepatitis C co-infection that may have provided insights into the pathogenesis of DM in our setting were not collected.
No relationship between diabetes and ART adherence emerged. While there is clear evidence that psychosocial factors are important in the pathogenesis of DM in HIV-uninfected adults in southern Africa,[9] more rigorous investigation is necessary to determine the role of psychosocial determinants in both ART adherence and diabetogenesis in HIV-infected adults.
The study has several limitations. Because of the cross-sectional study design we were able only to evaluate associations between the examined variables and diabetes. Given the retrospective nature of this study, we were also unable to determine whether patients had developed diabetes before or after the initiation of ART. Consequently, we could not assess whether HIV infection or ARV drug exposure played a causal role in the pathogenesis. Furthermore, despite excluding all confirmed type 1 diabetics, we could not exclude those in whom diabetes may have developed secondary to the use of drugs such as pentamidine or corticosteroids.
There were several traditional risk factors for the development of DM, such as family history, waist circumference, ethnicity, sedentary lifestyle, which were not included in our analysis. It would be valuable to assess the impact of these determinants in our setting, particularly given the increasing number of older, overweight persons living with HIV in southern Africa.[6] We were also unable to assess the potential impact of nucleoside reverse transcriptase inhibitors such as zidovudine and stavudine, both of which have been associated with an increased risk of diabetes.[2,11] Increased visceral fat and lipodystrophy, caused indirectly and directly by ARVs, may also contribute to disordered glucose homeostasis. The impact of lipodystrophy on the development of DM was not evaluated, given the retrospective nature of the study.
Conclusions
This case-control study suggests a complex interrelation among traditional host factors and treatment-related metabolic changes in the pathogenesis of DM. Patients with higher pre-ART weight and those exposed to EFV or a PI were more likely to have DM. Larger prospective studies are needed to delineate the relative contribution of other factors among people living with diabetes in southern Africa.
Acknowledgements. The Ministry of Health for granting us access to clinical data in our continued collaboration towards improving our understanding of the HIV epidemic in Botswana. This publication was made possible through assistance from the Institute of Health Sciences in Gaborone and core services and support provided by the Penn Center for AIDS Research (CFAR), a NIH-funded programme (P30 AI 045008).
References
1. Yoon C, Gulick RM, Hoover DR, Vaamonde CM, Glesby MJ. Case-control study of diabetes mellitus in HIV-infected patients. J Acquir Immune Defic Syndr 2004;37(4):1464-1469. [http://dx.doi.org/10.1097/01.qai.0000137373.26438.18] [ Links ]
2. Capeau J, Bouteloup V, Katlama C, et al; the ANRS CO8 APROCO-COPILOTE Cohort Study Group. Ten-year diabetes incidence in 1046 HIV-infected patients started on a combination antiretroviral treatment. AIDS 2012;26(3):303-314. [http://dx.doi.org/10.1097/QAD.0b013e32834e8776] [ Links ]
3. De Wit S, Sabin CA, Weber R, et al. Incidence and risk factors for new-onset diabetes in HIV-infected patients: The Data Collection on Adverse Events of Anti-HIV Drugs (D:A:D) study. Diabetes Care 2008;31(6):1224-1229. [http://dx.doi.org/10.2337/dc07-2013] [ Links ]
4. Hadigan C, Meigs JB, Corcoran C, et al. Metabolic abnormalities and cardiovascular disease risk factors in adults with human immunodeficiency virus infection and lipodystrophy. Clin Infect Dis 2001;32(1):130-139. [http://dx.doi.org/10.1086/317541] [ Links ]
5. Samaras K. The burden of diabetes and hyperlipidemia in treated HIV infection and approaches for cardiometabolic care. Curr HIV/AIDS Rep 2012;9(3):206-217. [http://dx.doi.org/10.1007/s11904-012-0124-x] [ Links ]
6. Reid MJA, Mosepele M, Tsima BM, Gross R. Addressing the challenge of the emerging NCD epidemic: Lessons learned from Botswana's response to the HIV epidemic [unresolved issues]. Public Health Action 2012;2(3):47-49. [http://dx.doi.org/10.5588/pha.12.0014] [ Links ]
7. Dave JA, Lambert EV, Badri M, West S, Maartens G, Levitt NS. Effect of nonnucleoside reverse transcriptase inhibitor-based antiretroviral therapy on dysglycemia and insulin sensitivity in South African HIV-infected patients. J Acquir Immune Defic Syndr 2011;57(4):284-289. [http://dx.doi.org/10.1097/QAI.0b013e318221863f] [ Links ]
8. Levitt NS, Steyn K, Dave J, Bradshaw D. Chronic noncommunicable diseases and HIV-AIDS on a collision course: Relevance for health care delivery, particularly in low-resource settings - insights from South Africa. Am J Clin Nutr 2011;94(6):1690S-1696S. [http://dx.doi.org/10.3945/ajcn.111.019075] [ Links ]
9. Peer N, Steyn K, Lombard C, Lambert EV, Vythilingum B, Levitt NS. Rising diabetes prevalence among urban-dwelling black South Africans. PLoS One 2012;7(9):e43336. [http://dx.doi.org/10.1371/journal.pone.0043336] [ Links ]
10. World Health Organization. Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycemia: Report of a WHO/IDF Consultation. Geneva: WHO, 2006. http://www.who.int/diabetes/publications/Definition%20and%20diagnosis%20of%20diabetes_new.pdf (accessed 23 July 2013). [ Links ]
11. Brown TT, Li X, Cole SR, et al. Cumulative exposure to nucleoside analogue reverse transcriptase inhibitors is associated with insulin resistance markers in the Multicenter AIDS Cohort Study. AIDS 2005;19(13):1375-1383. [http://dx.doi.org/10.1097/01.aids.0000181011.62385.91] [ Links ]
 Correspondence:
Correspondence:
M J A Reid
(michael.j.a.reid@gmail.com)
Accepted 4 July 2013














