Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.103 no.12 Pretoria Dez. 2013
RESEARCH
Poverty, AIDS and child health: Identifying highest-risk children in South Africa
L CluverI, II, III; M BoyesIV; M OrkinV; L SherrVI
IDPhil.Centre for Evidence-Based Intervention, Department of Social Policy and Intervention, University of Oxford, UK
IIDPhil. Department of Psychiatry and Mental Health, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
IIIDPhil. Health Economics and AIDS Research Division, University of KwaZulu-Natal, Durban, South Africa
IVPhD. Centre for Evidence-Based Intervention, Department of Social Policy and Intervention, University of Oxford, UK
VPhD. School of Public and Development Management, University of the Witwatersrand, Johannesburg, South Africa
VIPhD. Royal Free and University College Medical School, University College London, UK
ABSTRACT
BACKGROUND: Identifying children at the highest risk of negative health effects is a prerequisite to effective public health policies in Southern Africa. A central ongoing debate is whether poverty, orphanhood or parental AIDS most reliably indicates child health risks. Attempts to address this key question have been constrained by a lack of data allowing distinction of AIDS-specific parental death or morbidity from other causes of orphanhood and chronic illness.
OBJECTIVES: To examine whether household poverty, orphanhood and parental illness (by AIDS or other causes) independently or interactively predict child health, developmental and HIV-infection risks.
METHODS: We interviewed 6 002 children aged 10 - 17 years in 2009 - 2011, using stratified random sampling in six urban and rural sites across three South African provinces. Outcomes were child mental health risks, educational risks and HIV-infection risks. Regression models that controlled for socio-demographic co-factors tested potential impacts and interactions of poverty, AIDS-specific and other orphanhood and parental illness status.
RESULTS: Household poverty independently predicted child mental health and educational risks, AIDS orphanhood independently predicted mental health risks and parental AIDS illness independently predicted mental health, educational and HIV-infection risks. Interaction effects of poverty with AIDS orphanhood and parental AIDS illness were found across all outcomes. No effects, or interactions with poverty, were shown by AIDS-unrelated orphanhood or parental illness.
CONCLUSIONS: The identification of children at highest risk requires recognition and measurement of both poverty and parental AIDS. This study shows negative impacts of poverty and AIDS-specific vulnerabilities distinct from orphanhood and adult illness more generally. Additionally, effects of interaction between family AIDS and poverty suggest that, where these co-exist, children are at highest risk of all.
Child public health policy in Southern Africa faces a key question in decisions regarding targeting of interventions and resources, namely which indicators most reliably identify child vulnerability? Debate has centred on the question of whether household poverty, or orphanhood and household illness (AIDS-related or otherwise), are the best criteria to use.[1,2]
An important contribution to this question was published by the United Nations Children's Fund (UNICEF) in 2010.[3] This paper analysed pre-2008 Demographic and Household Survey (DHS) and Multiple Indicator Cluster Survey (MICS) data (with some AIDS Indicator Survey (AIS) data) from 36 countries to determine whether orphanhood, or living with an HIV-positive or chronically ill adult, predicted child vulnerability in three outcomes: wasting among 0 - 4-year-olds, school attendance among 10 - 14-year-olds, and early sexual debut among 15 - 17-year-olds. Results were summarised: 'In terms of wasting, early sexual debut, and to a lesser extent, school attendance, in the majority of surveys there were few significant differences between orphans and non-orphans or children living with chronically ill or HIV-positive adults and children not living with chronically ill or HIV-positive adults. Importantly, besides household wealth, no other potential markers of vulnerability consistently showed association or power to differentiate across the age-disaggregated outcomes.' (p.1078). The authors concluded that 'In many countries, targeting resources to children based solely on orphan status or co-residence with a chronically ill or HIV-positive adult in the household is not the most effective way of identifying vulnerable children'.
However, these valuable findings, and those of other contributions to the debate, were constrained by several limitations of the datasets that were available. Firstly, data such as DHS, MICS and AIS identify whether children are orphaned, but do not distinguish between orphanhood by AIDS and by non-AIDS causes. Secondly, some datasets identify chronic illness (and sometimes HIV status) of someone in the household, but none identify AIDS illness, or identify the child's primary caregiver. These are important limitations as evidence has subsequently demonstrated negative effects on children related to AIDS orphanhood and parental AIDS illness but not to asymptomatic HIV-positive status, other causes of orphanhood or chronic parental illness.[4-6] Thirdly, broad national household surveys are of great value in providing representative and comparable crosscountry data, but can only measure a limited set of child outcomes. These may not reflect the range of child vulnerabilities recently shown to be associated with parental AIDS, particularly mental health risks,[4,7] educational risks such as missing school to care for sick family members,[5] and specific HIV-infection risks such as transactional sex.[6] Indeed, some of these risks cannot be accurately assessed in surveys that use the household head as the respondent; adults are often unaware of the extent of some child risks, particularly internalising psychological distress and sexual behaviour.[8] Finally, the UNICEF paper notes that 'the analysis did not examine the interaction effects of some variables, in particular the interaction of wealth and orphan status'[3] and recommends that this be conducted in future analyses: 'As a whole, the data speak to the need for a multivalent approach to defining child vulnerability, such as combining wealth indicators with dimensions of AIDS-related vulnerability'.
Objectives
To (i) determine whether household poverty, orphanhood (by AIDS or other causes), and parental illness (by AIDS or other causes) independently predict child mental health, educational and HIV-infection risks; and (ii) to identify whether poverty interacts with orphanhood and/or parental illness status to exacerbate child risks.
For the purposes of this paper, 'orphanhood' refers to death of a biological parent, and 'parental AIDS-illness' refers to a parent or primary caregiver of the child.
Methods
Participants and procedures
Between 2009 and 2011, we interviewed 6 002 children (56% female) aged 10 - 17 years, using door-to-door household sampling of entire census enumeration or designated tribal areas. These were randomly selected from six health districts with >30% antenatal HIV-prevalence, in three SA provinces - Mpumalanga, Western Cape and KwaZulu-Natal. Health districts comprised deep rural, dense rural, commercial farming, peri-urban, urban and urban-homeland areas. One randomly selected child per household completed a 60 - 70 min face-to-face interview. All interviewers were trained and had prior experience of working with vulnerable children. Voluntary informed consent was obtained from both children and primary caregivers (response rate 97.2% of those approached). All questionnaires, information and consent forms were translated into Xhosa, Zulu, Sotho, SiSwati and Tsonga and back-translated, and children participated in the language of their choice. Confidentiality was maintained, except where participants were at risk of significant harm or requested assistance. Where participants reported abuse, rape or risk of significant harm, immediate referrals were made to child protection and health services. For past abuse or rape, referrals were made to support and counselling services and to HIV/AIDS testing and treatment services where appropriate.
Ethical protocols were approved by Oxford University, University of Cape Town, University of KwaZulu-Natal and Provincial Health and Education Departments of the Western Cape, Mpumalanga and KwaZulu-Natal. No participant incentives were given, apart from refreshments and certificates of participation.
Potential predictors
Household poverty
Household poverty was measured using an index of access to the eight highest socially-perceived necessities for children in SA. These were identified through focus groups,[9] followed by corroboration by >80% of the population in the nationally representative South African Social Attitudes Survey.'101 Necessities comprised: 3 meals/day, a visit to the doctor and medicines when needed, enough clothes to remain warm and dry, soap to wash every day, money for school fees, school uniform and one pair of shoes. This index was combined into a dichotomised variable of lacking more than half of child necessities to identify severe poverty.
Orphanhood status
The United Nations definition of orphanhood was used - i.e. loss of one or both parents.[11] In SA, death certificates rarely define AIDS mortality and retrospective clinical data are limited.[12] Cause of parental death was therefore determined using the verbal autopsy method,[13] validated in SA with sensitivity of 89% and specificity of 93%.[14] Determination of AIDS-related parental death required a conservative threshold of ≥3 AIDS-defining illnesses; e.g. Kaposi's sarcoma or shingles.
Parent/primary caregiver illness status
For current, chronic illness, self-report of HIV/AIDS is also unreliable due to low levels of HIV-testing, with an estimated two-thirds of HIV-positive people unaware of their current status.[15] Parental AIDS illness was thus determined using a verbal symptom checklist, parallel to the verbal autopsy method, to identify stage 4 AIDS illness through opportunistic infections such as diarrhoea, oral candidiasis and Kaposi's sarcoma, as well as a range of other chronic illnesses such as diabetes. In this study, determination of parental AIDS illness required either (i) a conservative threshold of ≥3 AIDS-defining illnesses; or (ii) parent self-identification of symptomatic AIDS or CD4+ count of <300 cells/ml.
Socio-demographic co-factors
Socio-demographic co-factors were child age, gender, urban/rural location and formal/informal housing following census definitions.
Child outcome measures
Mental health disorder
Mental health disorder was measured by standardised scales used previously with children in SA. Depression was measured using the ten-item Child Depression Inventory (CDI) short form,[16] which is highly correlated with the full CDI, has strong psychometric properties and showed reliability in the current sample of α=0.73. Anxiety was measured using the Revised Children's Manifest Anxiety Scale[17] which has been validated for use in SA,[18] and reduced using factor analysis to 14 items (current sample reliability α=0.84).[19] Suicidal planning or attempts were measured with the Mini-International Neuropsychiatric Interview for Children and Adolescent Suicidality subscale[20] (current sample reliability α=0.80). Each scale was dichotomised using standardised clinical cut-offs into 0 = no disorder or 1 = presence of disorder and combined into an overarching scale of number of disorders.
Negative educational outcomes
Negative educational outcomes were school non-enrolment, extended periods (>1 week) of past-year school non-attendance, being ≥2 years behind age-appropriate school grade and inability to concentrate in school due to worry about home circumstances.[21] The dichotomies were combined into an overarching scale of number of educational risks.
HIV-infection risks
HIV-infection risks were measured using a checklist of items from the National Survey of HIV and Risk Behaviour among Young South Africans and the South African DHS.[22,23] Items included transactional sexual exploitation (sex in exchange for food, shelter, school fees, transport or money), sexual debut at age <15 years, ≥3 past-year sexual partners, more than half of sexual acts unprotected in past month, pregnancy/making someone pregnant and having a sexual partner >5 years older than the child. The dichotomies were combined into an overarching scale of number of HIV-infection risks.
Analysis strategy
Analyses were conducted in three stages. First, descriptive statistics summarising mental health, educational and HIV-infection risks as a function of orphanhood and parental health status were calculated. Second, multivariate regressions were conducted for each risk domain, controlling for child age, gender, rural/urban location and formal/informal dwelling. Household poverty, AIDS orphanhood, other orphanhood, parental AIDS illness and parental other illness were entered as independent predictors applying dummy coding, alongside four hypothesised interaction terms: poverty with AIDS orphanhood, other orphanhood, parental AIDS illness and parental other illness. Main effects for all independent variables, as well as any interactions between poverty, orphanhood and parental illness status are reported for each outcome. Dummy coding was retained for ease of interpretation, after checking that the pattern of effects was unchanged compared with contrast coding.[24]
Results
Sample characteristics
Descriptive statistics for all socio-demographic and risk outcome variables (as a function of orphanhood and parental sickness status) are summarised in Table 1. We noted differences associated with cause of orphanhood: among AIDS-orphaned children, 54% were maternally bereaved and 22% double orphaned (both maternally and paternally bereaved), while among other orphaned children, 32% were maternally bereaved and 12% double orphaned. There was also notable overlap between relevant groups: 35% of AIDS-orphaned children lived with a surviving, AIDS-unwell parent or primary caregiver. Risk outcomes showed gender differences, with girls reporting more mental health and concentration problems, transactional sex and older sexual partners and boys reporting more school grade delay. All childhood risks increased with child age. Therefore, gender and age were controlled for in all further analyses.
Associations of poverty, orphanhood status and caregiver sickness status on child risks
Mental health risks
Multivariate regression confirmed that poverty, AIDS orphanhood and parental AIDS illness all predicted increased likelihood of mental health disorder independently of each other and of socio-demographic co-factors (Table 2). Other orphanhood and other chronic parental illness were not significant predictors of mental health risks. Exacerbating interaction effects were shown between poverty and AIDS orphanhood (p<0.001; ß=0.06) and between poverty and parental AIDS illness (p<0.001; ß=0.06): children who were simultaneously AIDS-orphaned or living with an AIDS-ill parent, and living in severe poverty, reported more mental health disorders (Fig. 1A). There was no interaction between poverty and other orphanhood or parental other chronic illness. Fig. 2A shows that presence of poverty alone increases mental health disorder risk by 0.08 standard deviations (SDs). The middle point on the topmost line shows that this would increase to 0.20 SDs if the main effects only of both parental AIDS illness and poverty were at work. However, the regression indicated two significant interactions, between poverty and AIDS illness and between poverty and AIDS orphanhood. The far point on the topmost line shows the combined effect - an increase up to 0.30 SDs in mental health risk.
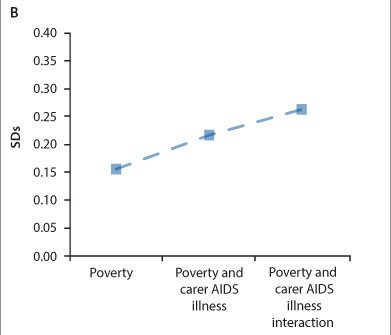
Educational risks
Poverty and parental AIDS illness predicted increased likelihood of educational risks independently of each other and of socio-demographic co-factors. Orphanhood status (by AIDS or other causes) and other parental chronic illness were not significant predictors of educational risk. There were no interactions between poverty and orphanhood status. An exacerbating interaction effect of poverty and parental AIDS illness was shown - children who were simultaneously living with an AIDS-ill parent and in severe poverty reported more educational risks (Figs 1B and 2B). There was no interaction effect between poverty and other parental chronic illness.
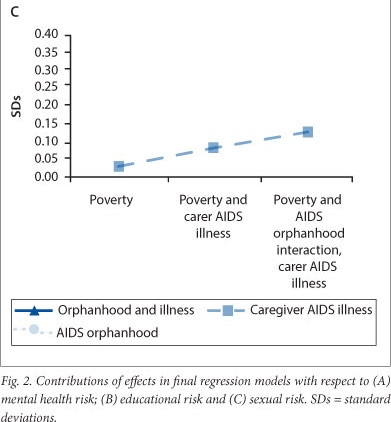
HIV-infection risks
Parental AIDS illness was the only independent predictor of increased HIV-infection risks, controlling for socio-demographic co-factors. Poverty, orphanhood status (by AIDS or other causes) and other parental chronic illness did not independently predict likelihood of HIV-infection risks. However, an exacerbating interaction effect of poverty and AIDS orphanhood was also shown - children who were simultaneously AIDS orphaned and living in severe poverty reported more HIV-infection risks (Figs 1C and 2C). There was no interaction effect between poverty and parental illness status.
Discussion
This research is the first known to allow simultaneous disaggregation of children living in households below and above a poverty line, in urban and rural, formal and informal settlements, as well as involving six (frequently overlapping) groups of children: those non-orphaned, orphaned by AIDS or by non-AIDS causes; living with healthy parents, AIDS-ill or other-ill parents. We measured a wide range of child health and developmental outcomes, allowing investigation of mental health risks (depression, anxiety, suicidality); educational risks (non-enrolment, low school attendance, grade delay and concentration difficulties); and HIV-infection risks (trans-actional sex, childhood pregnancy or making someone pregnant, multiple sexual partners, early debut, low condom use, and having sexual partners ≥5 years older than the child).
These findings demonstrate five key implications for our understandings of child vulnerability in a high HIV-prevalence context.
First, they show both poverty-specific and AIDS-specific vulnerabilities for children. In this study, severe household poverty independently predicted child mental health and educational risks, AIDS orphanhood independently predicted mental health risks and parental AIDS illness independently predicted all three child outcomes of mental health, educational and HIV-infection risk. In other words, both poverty and family AIDS illness will lead us to the most vulnerable children, but a focus restricted to one or the other will exclude some of those most vulnerable.
Second, these findings demonstrate that there are indeed parental AIDS-specific health vulnerabilities for children. They support previous findings that orphanhood and parental chronic illness per se do not consistently predict child risks; indicators of orphanhood and parental illness that were not AIDS-related showed no predictive value for any child risk. For these children, poverty is a more important indicator of their vulnerability and using orphanhood or chronic illness alone as an indicator would exclude some children who may be vulnerable, and include others who may not be. However, disaggregation by AIDS-related illness and death showed that AIDS orphanhood and parental AIDS illness do predict child risks. Family AIDS has impacts on child health and development that are not only independent of the impacts of poverty, but also independent of illness and orphanhood more generally.
Third, analyses suggest that living with an AIDS-ill parent has stronger negative impacts than AIDS orphanhood on child mental health, educational and HIV-infection risks. This needs to be interpreted in the context of high levels of overlap between AIDS orphanhood and parental AIDS illness, but supports arguments that children may be at highest risk when a parent is alive but extremely unwell.[25]
Fourth, when poverty is co-present in a family with either parental AIDS illness or death, the result is an even greater threat to children than the additive effect of the two indicators. Findings indicate that severe poverty interacts variously with AIDS orphanhood and parental AIDS illness to exacerbate child mental health, educational, and HIV-infection risks. As would be expected in a non-experimental setting, interaction effects are not large, but given the adequate sample they are strongly significant.[26] No interactions were found between poverty and other-orphanhood or other chronic parental illness.
Lastly, these findings have implications for the data that we collect on child vulnerability. They demonstrate the value of including broad, validated and sensitive measures of child outcomes - in particular, mental health risks such as depression and suicidality that are closely linked with traumatic child experiences. They support the measurement of household poverty as an important indicator of child outcomes. They also suggest that indicators focusing on orphanhood per se and household adult chronic illness may require additional 'AIDS sensitivity' to identify child vulnerability. It could be of great value in future national surveys to collect data that allow disaggregation of the cause of orphanhood and of primary caregiver illness and thus identify key indicators of AIDS orphanhood and parental AIDS illness.
Study limitations
This study had a number of limitations. First, it would be important to conduct similar studies or analyses in additional countries.
Second, all cross-sectional data are limited in determining causality, although in this case, reverse causality is extremely unlikely (i.e. child mental health, educational and HIV-infection risks do not cause household poverty or parental AIDS illness or death).[27]
Third, there are no validated clinical cut-offs for child mental health disorder in Africa, although all scales had been extensively used or validated in SA.
Fourth, the study did not measure whether children were themselves infected with HIV. Only a small proportion of this sample would have been peri-natally HIV infected, owing to their birth 4 - 14 years before the beginning of the antiretroviral rollout in SA and low rates of survival in the pre-antiretroviral period,[28] but others could have been infected during childhood or adolescence. Future research could valuably examine whether childhood HIV infection interacts with family factors to further exacerbate child risks.
Fifth, the measure of household poverty in this sample was primarily identifying 'severe' poverty, as all six of the study sites were in low-income areas.
Lastly, while many child risks can only be accurately reported by children themselves (such as sexual behaviour and mental health), child self-reporting should ideally be supplemented by adult reporting and administrative data such as school registers, where this is available and reliable.
Conclusion
Despite these limitations, the findings of this study strongly support international policies and research emphasising the need for accurately targeted 'AIDS-sensitive' health and social protection programmes for children.[29,30] They also suggest a re-framing of some debates that posit poverty, orphanhood or family AIDS as competing indicators of child vulnerability in sub-Saharan Africa. If we are to identify children at high risk, it is essential that both poverty and parental AIDS are recognised and measured. And where poverty and AIDS interact - as is so often seen - we find the children at the highest risk of all.
Acknowledgements. The authors wish to thank our fieldwork teams in the Western Cape, KwaZulu-Natal and Mpumalanga. Most importantly, we thank the all the participants and their families. This study was funded by the UK Economic and Social Research Council, the SA National Research Foundation, the Health Economics AIDS Division at the University of KwaZulu-Natal, the SA National Department of Social Development, the Claude Leon Foundation, the John Fell Fund and the Nuffield Foundation.
References
1. A new agenda for children affected by HIV/AIDS. Lancet 2009;373(9663):517. [http://dx.doi.org/10.1016/S0140-6736(09)60174-4] [ Links ]
2. Temin M. HIV-sensitive Social Protection: What Does the Evidence Say? Geneva: UNAIDS, 2010. [ Links ]
3. Akwara PA, Noubary B, Lim Ah Ken P, et al. Who is the vulnerable child? Using survey data to identify children at risk in the era of HIV and AIDS. AIDS Care 2010;22(9):1066-1085. [http://dx.doi.org/10.1080/09540121.2010.498878] [ Links ]
4. Sherr L, Mueller J. Where is the evidence base? Mental health issues surrounding bereavement and HIV in children. J Public Ment Health 2008;7(4):31-39. [http://dx.doi.org/10.1108/17465729200800027] [ Links ]
5. Guo Y, Li X, Sherr L. The impact of HIV/AIDS on children's educational outcome: A critical review of global literature. AIDS Care 2012;24(8):993-1012. [http://dx.doi.org/10.1080/09540121.2012.668170] [ Links ]
6. Cluver L, Orkin M, Boyes M, Gardner F, Meinck F. Transactional sex amongst AIDS-orphaned and AIDS-affected adolescents predicted by abuse and extreme poverty. J Acquir Immune Defic Syndr 2011;58:336-343. [http://dx.doi.org/10.1097/QAI.0b013e31822f0d82] [ Links ]
7. Nyamukapa C, Gregson S, Lopman B, et al. HIV-associated orphanhood and children's psychosocial distress: Theoretical framework tested with data from Zimbabwe. Am J Public Health 2008;98(1):133-141. [http://dx.doi.org/10.2105/AJPH.2007.116038] [ Links ]
8. Ivens C, Rehm L. Assessment of childhood depression: Correspondence between reports by child, mother and father. J Am Acad Child Adolesc Psychiatry 1988;27:738-741. [http://dx.doi.org/10.1097/00004583-198811000-00012] [ Links ]
9. Barnes H, Wright G. Defining Child Poverty in South Africa Using the Socially Perceived Necessities Approach. In: Minujin A, ed. Global Child Poverty and Well-Being: Measurement, Concepts, Policy and Action. University of Bristol: The Policy Press, 2012. [ Links ]
10. Pillay U, Roberts B, Rule S, eds. South African Social Attitudes: Changing Times, Diverse Voices. Cape Town: HSRC Press, 2006. [ Links ]
11. UNAIDS. Children on the Brink 2004: A Joint Report of New Orphan Estimates and a Framework for Action. New York: UN, 2004. [ Links ]
12. World Health Organisation. Global TB Control Report 2011. Geneva: WHO, 2011. [ Links ]
13. Lopman B, Barnabas R, Boerma T, et al. Creating and validating an algorithm to measure AIDS mortality in the adult population using verbal autopsy. PLoS Med 2006;3(8):e312. [http://dx.doi.org/10.1371/journal.pmed.0030312] [ Links ]
14. Kahn K, Tollman S, Garenne M, Gear J. Validation and application of verbal autopsies in a rural area of South Africa. Trop Med Int Health 2000;5(11):824-831. [http://dx.doi.org/10.1046/j.1365-3156.2000.00638.x] [ Links ]
15. Peltzer K, Matseke G, Mzolo T, Majaja M. Determinants of knowledge of HIV status in South Africa: Results from a population-based HIV survey. BMC Public Health 2009;9(1):174. [http://dx.doi.org/10.1186/1471-2458-9-174] [ Links ]
16. Kovacs M. Children's Depression Inventory. Niagra Falls, NY: Multi-health Systems, 1992. [ Links ]
17. Reynolds C, Paget K. National normative and reliability data for the Revised Children's Manifest Anxiety Scale. School Psychol Rev 1983;12(3):324-336. [ Links ]
18. Boyes M, Cluver L. Performance of the Revised Children's Manifest Anxiety Scale in a sample of children and adolescents from poor urban communities in Cape Town. Eur J Psychol Assess 2013;29(2):113-120. [http://dx.doi.org/10.1027/1015-5759/a000134] [ Links ]
19. Cluver L, Orkin M, Gardner F, Boyes M. Persisting mental health problems among AIDS-orphaned children in South Africa. J Child Psychol Psychiatry 2012;53(4):363-370. [http://dx.doi.org/10.1111/j.1469-7610.2011.02459.x] [ Links ]
20. Sheehan D, Shytle D, Milo K. MINI-KID: Mini International Neuropsychiatric Interview for Children and Adolescents. English Version 4.0. Tampa: University of South Florida, Paris: Hopital de la Salpetriere, 2004. [ Links ]
21. Cluver L, Operario D, Lane T, Kganakga M. 'I can't go to school and leave her in so much pain' Educational shortfalls among adolescent young carers in the South African AIDS epidemic. J Adolescent Res 2012;27(5):581-605 [http://dx.doi.org/10.1177/0743558411417868] [ Links ]
22. Pettifor A, Rees H, Kleinschmidt I, et al. Young people's sexual health in South Africa: HIV prevalence and sexual behaviors from a nationally representative household survey. AIDS 2003;19(14):1525-1534. [ Links ]
23. National Department of Health, South African Medical Research Council. Demographic and Health Survey 2003. Pretoria: NDoH, 2007. [ Links ]
24. Cohen J, Cohen P, West S, Aiken L. Applied Multiple Regression/Correlation Analysis for the Behavioural Sciences. London: Lawrence Erlebaum Associates, 2003. [ Links ]
25. Richter L, Foster G, Sherr L. Where the Heart Is: Meeting the Psychosocial Needs of Young Children in the Context of HIV/AIDS. Toronto: Bernard van Leer Foundation, 2006. [ Links ]
26. McClelland G, Judd C. Statistical difficulties of detecting interactions and moderator effects. Psychol Bull 1993;114(2):376-390. [ Links ]
27. Davis J. The Logic of Causal Order. Beverley Hills, CA: Sage, 1985. [ Links ]
28. Newell M-L, Coovadia H, Cortina-Borja M, Rollins N, Gaillard P, Dabis F. Mortality of infected and uninfected infants born to HIV-infected mothers in Africa: A pooled analysis. Lancet. 2004;364(9441):1236-1243. [http://dx.doi.org/10.1016/S0140-6736(04)17140-7] [ Links ]
29. UNAIDS. HIV and Social Protection Guidance Note. New York: UN, 2011. [ Links ]
30. Robertson L, Mushati P, Eaton JW, et al. Household-based cash transfer targeting strategies in Zimbabwe: Are we reaching the most vulnerable children? Soc Sci Med 2012;75(12):2503-2508. [http://dx.doi.org/10.1016/j.socscimed.2012.09.031] [ Links ]
 Correspondence:
Correspondence:
L Cluver
(lucie.cluver@spi.ox.ac.uk)
Accepted 30 September 2013