Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.103 no.10 Pretoria ene. 2013
IZINDABA
Leadership, commitment and core values garner national award
Chris Bateman
Careworn, skeletally-staffed and under-equipped: that was Zithulele Hospital, snagged in a dusty web of rutted roads atop a coastal hill near Coffee Bay, 99 km from Mthatha, eight years ago. Today the hospital is a rare beacon of hope, efficiency and delivery in a sea of rural public healthcare apathy, dysfunction and maladministration.
The 'miracle' was wrought by a committed multidisciplinary team built by young University of Cape Town (UCT)-trained doctor couple, Ben and Taryn Gaunt, whose leadership, dedication and persistence have won the admiration of their rural colleagues countrywide.[1] In July they jointly won the prestigious Pierre Jacques Rural Doctor of the Year Award. Named after a doyen of rural medical practice and founding member of the Rural Doctors Association of Southern Africa (RUDASA), the award is jointly presented by RUDASA, the Southern African HIV Clinicians' Society and the Rural Health Advocacy Project. It perpetuates Dr Jacques' tireless advocacy for rural health and the role of the rural doctor in South Africa.
When the Gaunts arrived in what is officially listed as one of the most poverty-stricken rural districts in the country, the 146-bed hospital was serving the health needs of some 143 000 people with just one senior medical officer and two community service doctors - something far too many rural district hospitals countrywide still regard as 'about the usual'. Zithulele is now among the few shining exceptions, with a clinical team of 29 people, consisting of 10 full-time and three part-time doctors, three physiotherapists, two occupational therapists, a speech therapist, an audiologist, a social worker, a dentist, two pharmacists and two dieticians. This core group has partnered with five NGOs to bring the professional skills of over 50 people to the community. The Jabulani Rural Health Foundation, an NGO started by the Gaunts and a second husband-and-wife UCT-trained doctor couple, Karl and Sally le Roux, bolsters their work by providing them with translators, counsellors and assistants while assisting with antiretroviral (ARV) down-referrals.

From humble beginnings, Jabulani has raised over R3 million from major corporates and other donors. Among other things, this has been used to expand accommodation options for professional staff (including for local teachers), as lack of accommodation and shoddy housing are significant barriers to healthcare worker recruitment and retention in rural areas. The NGO's other community developmental work includes starting two pre-schools and opening a library. Additionally, the Gaunts provide those core rural recruitment and retention ingredients: solid and committed vocational leadership, backed by a deep and appropriate array of general clinical skills.
It was Karl le Roux who nominated the Gaunts for the Pierre Jacques award. The two couples were classmates in both high school and medical school, and he says that the Gaunts will be 'the first to insist that the achievements of the past year are entirely due to the remarkable team of doctors, nurses and therapists and many others who work at Zithulele. Yet the very existence of this team is in large part due to their obedience to what they felt was God's call for them to work in rural medicine when they were still students.'
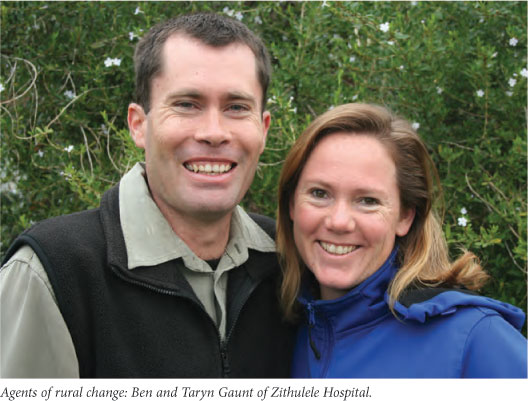
He described Ben Gaunt as 'an excellent clinician and visionary clinical manager, a gifted administrator with incredible drive and focus'. Taryn Gaunt he characterised as 'the perfect foil to Ben's workaholism, as a home-schooling mom of four kids and a compassionate clinician with a love for paediatrics and impressive expertise in paediatric tuberculosis (TB) and HIV.
In the past year alone the first-ever cataract operations at Zithulele were performed as part of the Mercy Ships Eastern Cape Mercy Vision Project. The hospital now offers cataract surgery every fortnight as well as clinic-based primary eyecare, including the provision of spectacles. The year-on-year perinatal mortality rate has dropped to under 20 deaths per 1 000 (remarkably low for a rural district hospital), and for the first time extremely premature babies with birth-weights of under 1 000 g are beginning to survive (five since September last year, with the record at 900 g). The ARV programme has been expanded to more than 3 500 patients (with 90% collecting their prepacked, individually-labelled medicines at their nearest clinic), and the first hearing aids have been fitted at the hospital. Paediatric ward mortality has dropped from over 10% in 2007/8 to below 2%. In the year the Gaunts arrived just over 10 000 people received help from the hospital; outpatient numbers last year topped 27 000, while the clinical team see over 5 000 people at outlying clinics.
Ben Gaunt told Izindaba that his doctors visit all 10 clinics either weekly or monthly, depending on their size, while the dentist and allied health professionals attend the clinics regularly. 'We also have a reasonably good level of support for our community-based multidrug-resistant TB patients -everyone gets a home visit and child contacts are actively traced.'
He added, 'I think the future makes me more excited than the past. We obviously still have lots of challenges around budgeting and procurement, but there's the prospect of some progress. Also, the national department look like they'll fulfil their promise of the final phase of revitalisation here. We have much work still to do, including improving primary healthcare, and especially our data systems. We are exploring working with a sixth NGO to better support people with disabilities.'
The five NGOs already involved with Zithulele include the Philani programme's Mentor Mothers Zithulele, a community-based maternal and child health project that is anchored on 60 local 'motherhood veterans' between Zithulele and Coffee Bay, and whose footprint is growing annually. Meanwhile, Axium Education focuses on teaching local children maths, science and English from Grade 10 - 12. Some children are now 'shadowing' doctors at the hospital and accessing bursaries - one is studying nursing and another is on the Cuban doctor-training programme. Elsewhere, the Donald Woods Foundation is helping to expand the hospital's ARV programme to the clinics, with an emphasis on quality care.
Concludes Gaunt, 'We certainly haven't even got halfway yet, and like most rural hospitals we face plenty of challenges and have quite a significant staff turnover, though we've managed to keep one-year folk for two and sometimes three or more years.' This includes Liz Gatley, winner of the Pierre Jacques Provincial Rural Doctor of the Year award in 2011, who completed her community service year at Zithulele in 2009 and stayed on,[2] and whom Gaunt describes as 'a stalwart.'
Asked how he stays afloat in what is so often a sea of provincial healthcare dysfunction, Gaunt responded: 'Having a long-term vision is helpful. You have to pick your battles in the public sector; often we just don't have the emotional energy or the resource capacity to fight a particular battle right then. One of our strategies is to say, "a little better tomorrow than today". Some things take a long time to change. Our main focus is to provide high-quality healthcare to rural people and our clinicians haven't let go of that student dream - it's not always gold-standard care, but that remains the goal. You don't give up, you carry on doing your best.'
Zithulele's six core values bear repeating in an age where abuse of the Remunerative Work Outside the Public Service (RWOPS) programme has come dangerously close to the norm in many more urban environments. They are:
- prioritising patients by providing quality care with compassion and respect
- valuing interdependence by sharing responsibility for patient care in a non-competitive environment
- respectful relationships (communicating respectfully in an open and honest, but constructive, way with colleagues)
- building people up by recognising, acknowledging and encouraging their strengths
- seeking continual learning (from one another and the community, and staying up to date with relevant health research and developments)
- a hopeful attitude (looking for the positive in challenging situations and encouraging one another to avoid cynical talk).
It is the dream of bringing hope to their rural community that sustains the Gaunts and Zithulele Hospital, and provides an example of what is possible in challenging situations.
1. Bateman C. Multidisciplinary teams - the rural way forward. S Afr Med J 2008;98(1):19-22. [ Links ]
2. Bateman C. Rural E-Cape award winner: "My motivation - seeing medicine change lives'. S Afr Med J 2012;102(1):17-18. [ Links ]














