Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.103 no.8 Pretoria Jan. 2013
RESEARCH
Review of causes of maternal deaths in Botswana in 2010
S RayI; F D MadzimbamutoII; D Ramagola-MasireIII; R PhillipsIV; K D MogobeV; M HaverkampVI; M MokatediVII; M MotanaVIII
IMB BS, Bsc, MSc, MPH FFPHM (UK). School of Medicine, University of Botswana, Gaborone, Botswana
IIBSc, MB ChB, MMed (Anaes), FRCA. School of Medicine, University of Botswana, Gaborone, Botswana
IIIMD, FCOG (SA). School of Medicine, University of Botswana, Gaborone, Botswana
IVMD. Government of Botswana/University of Pennsylvania (Botswana-UPenn) Partnership, Gaborone, Botswana
VMD, MPH. Government of Botswana/University of Pennsylvania (Botswana-UPenn) Partnership, Gaborone, Botswana
VIRN, PhD. School of Nursing, University of Botswana, Gaborone, Botswana
VIIRN, MSc (Nursing). School of Nursing, University of Botswana, Gaborone, Botswana
VIIIRGN, BEd Nursing, MSc (Nursing). Medical Education Partnership Initiative (MEPI) Maternal Mortality Project, Gaborone, Botswana
ABSTRACT
BACKGROUND: In Botswana the maternal mortality ratio in 2010 was 163 per 100 000 live births. It is a priority to reduce this ratio to meet Millennium Development Goal 5 target of 21 per 100 000 live births.
OBJECTIVE: To investigate the underlying circumstances of maternal deaths in Botswana.
METHOD: Fifty-six case notes from the 80 reported maternal deaths in 2010 were reviewed. Five clinicians reviewed each case independently and then together to achieve a consensus on diagnosis and underlying cause(s) of death.
RESULTS: Sixty-six percent of deaths occurred in Botswana's two referral hospitals. Cases in which death had direct obstetric causes were fewer than cases in which cause of death was indirect. The main direct causes were haemorrhage (39%), hypertension (22%), and pregnancy-related sepsis (13%). Thirty-six (64%) deaths were in HIV-positive women, of whom 21 (58%) were receiving antiretroviral (ARV) therapy. Nineteen (34%) deaths were attributable to HIV, including 4 from complications of ARVs. Twenty-nine (52%) deaths were in the postnatal period, 19 (66%) of these in the first week. Case-note review revealed several opportunities for improved quality of care: better teamwork, communication and supportive supervision of health professionals; earlier recognition of the seriousness of complication(s) with more aggressive case-management; joint management between HIV and obstetric clinicians; screening for, and treatment of, opportunistic infections throughout the antenatal to postnatal periods; and better supply management of medications, fluids, blood for transfusion and laboratory tests.
CONCLUSION: Integrating HIV management into maternal healthcare is essential to reduce maternal deaths in the region, alongside greater efforts to improve quality of care to avoid direct and indirect causes of death.
Although the Government of Botswana has made considerable inputs into health services delivery, the country's maternal mortality ratio (MMR) has not declined sufficiently to meet the 2015 Millennium Development Goal 5 target of 21 per 100 000 (Fig. 1).[1-3] The rise in deaths between 1995 and 2000 is attributed to the corresponding rise in HIV prevalence in women[1-3] and to improved notifications following the establishment of the maternal mortality monitoring system in 1998.[4] Research in Southern Africa now shows the emerging predominance of indirect causes of maternal deaths over direct causes, mainly linked to HIV and non-pregnancy-related infections. This calls for radical changes in the approach to preventing maternal mortality.[5-7] The UNAIDS Global Plan has now set a target of halving HIV-related maternal deaths by 2015.[8]
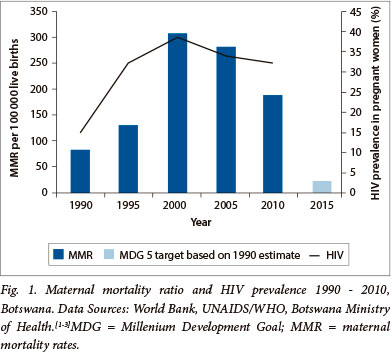
Botswana has achieved impressive levels of service engagement for pregnant women. In 2007, 73% of women attended at least 4 antenatal care (ANC) visits, while 95% of all reported deliveries occurred in health facilities, suggesting relatively complete identification of maternal deaths.[9] A high proportion of deliveries were attended by skilled health professionals: 97% of deliveries in cities, towns and urban villages and 90% of deliveries in rural areas.[9] There were 49 853 institutional live births and 475 non-institutional live births in 2010. There were 82 maternal deaths reported to the Ministry of Health (MoH), giving an MMR of 163 per 100 000 live births, v. the government-stated target of 130 for that year.[10] HIV prevalence in pregnant women was estimated at 28.7% in 2010,[11] with 94% of eligible HIV-positive pregnant women receiving antiretroviral (ARV) therapy.[12]
Botswana has an estimated 0.58 doctors and 4.51 nurses and midwives (or 4.19 doctor equivalents) per 1 000 population. It is 1 of 8 countries in sub-Saharan Africa that exceeds the World Health Organization (WHO) estimate of 2.28 health professionals per 1 000 population needed to achieve 80% coverage for deliveries by skilled birth attendants.[13] Botswana was also found to be an 'extreme outlier' in 2008, since it received US$427.8 per live birth for maternal and newborn health in development aid, compared with US$46.1 in Zambia and US$16.5 in Ethiopia.[14] Since resources were not the main constraint during this period, the challenge of reducing the MMR lies in identifying the underlying causes of maternal deaths, with a view to identifying possible solutions.
Confidential enquiries conducted in South Africa (SA) since 1999 have documented avoidable factors, missed opportunities and examples of substandard care contributing to maternal deaths.[15] Similar enquiries have been carried out in Botswana since 2007. However, these enquiries have not led to any significant changes in practices, as demonstrated by negligible declines in mortality. This study aims to review the circumstances of each death and reveal weaknesses in the health system, the correction of which would have a discernible impact on the MMR.
Botswana, a middle-income country, has a population of 2 million served by 2 referral hospitals (which also provide district functions for the populations of Gaborone and Francistown), 31 district and primary hospitals, 263 clinics (92 with maternity facilities) and 342 health posts. Over 95% of the Botswana population live within a radius of 8 km to 15 km of a health facility.[9]
The WHO defines maternal death as the death of a woman while pregnant or within 42 days of termination of pregnancy, from any cause related to, or aggravated by, the pregnancy or its management, but not from accidental or incidental causes.[16]
Methodology
The study was approved by the University of Botswana Institutional Review Board, the Botswana MoH and the individual hospitals from which notes were obtained.
Of the 82 notified deaths, the case notes of 58 were provided by MoH facilities for review in this study; 24 case notes were missing. Two cases were discounted: 1 death occurred in 2009 and 1 was an incidental death, resulting from a stab wound. The total number of records reviewed was 56. Each record was reviewed independently by two pairs of clinicians and an HIV specialist, who then discussed each case to achieve consensus. Data items from the notes were entered onto a standardised data-entry form.
Authors SR and FM analysed data manually. Descriptive statistics such as number, percentages and means with standard deviation (SD) were calculated.
Results
The analysis (involving the 56 patients whose case notes were available) accounted for 70% of the 80 maternal deaths that occurred in 2010.
The mean age (±SD) was 29.4 (±6.5) with a range of 18 to 45 years. The mean gravidity (±SD) was 2.8 (±1.6) with a range of 1 - 6; 13 (23%) were primigravida, 32 (57%) were multigravida, and 11 (20%) were grand multigravida (gravida 5 and 6).
Six of the women (11%) suffered miscarriages prior to 24 weeks, 4 at home and 2 at a referral hospital. Six women (11%) delivered at home, unattended by skilled health professionals, and were transferred to hospital in the postpartum period. Two women delivered at a clinic and 1 at a private facility. Twelve women (21%) delivered at a district hospital and 22 (39%) delivered at a referral hospital. Six women (11%) died undelivered at referral hospitals. Thirty-seven deaths (66%) occurred at the 2 referral hospitals while 16 (29%) occurred at district hospitals. One woman was brought to hospital having died at home. Data were missing on the place of death for 2 women who had been admitted to a referral hospital.
Eighteen women (32%) died in the antenatal period. Five died during delivery and 4 died during caesarean section. There were 29 deaths (52%) in the postpartum period: 12 (41%) died within 24 hours of delivery, 14 (48%) died within 7 days of delivery, 6 died in the second week, 2 died in the third week and 1 died in the fourth week. While the majority (27) were kept in hospital after delivery because of their poor clinical condition, two women left the facility soon after delivery but required readmission prior to death. Of the total, 24 women (43%) died within 24 hours of admission, indicating the seriousness of their condition at time of admission.
Thirty-six (64%) women were HIV-positive. Of these, 20 (56%) were on antiretroviral therapy (ART), 4 (11%) received zidovudine (AZT) for prevention of mother-to-child transmission (PMTCT), and 12 (33%) were not receiving ARVs. Eleven (20%) women were HIVnegative. In 9 (16%) women, HIV status was unknown.
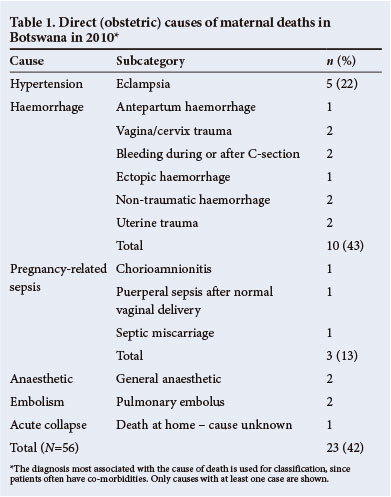
Tables 1 and 2 show the direct and indirect causes of death for 55 of the 56 women (data missing on 1 death). Cause of death was related to a direct obstetric cause in 23 (42%) women, to haemorrhage in 10 (43%), hypertension in 5 (22%) and pregnancy-related sepsis in 3 (13%). In 32 (58%) women, death was due to indirect causes. Death was attributable to HIV in 19 (34%) cases, of whom 12 (63%) had clinical AIDS.
Of the 6 women who died following transfer to hospital after delivery, 3 had AIDS, 2 suffered postpartum haemorrhage at home, and 1 was in diabetic coma.
Review of the 56 records revealed that there was considerable overlap between healthworker- and health system-related factors contributing to the deaths. Overall, 25 deaths (45%) were considered unavoidable at the point of presentation to hospital, though there were preventable factors earlier in the pregnancies. Care was substandard in all cases. (Selected cases, shown in Table 3, serve to elaborate on opportunities for the improvement of maternity services.)
Patient-related factors
Eleven women failed to attend clinics for any ANC. Seven of the ten women who died in the first trimester, died of complications related to sepsis and haemorrhage. Four women presented late to hospital with meningitis, pre-eclampsia and heart failure. One patient delayed presentation for10 hours while consulting a traditional healer.
Healthworker-related factors
In all cases, there were opportunities to improve teamwork between health professionals and between speciality teams. In 17 (30%) cases there was evidence of poor communication between doctors and nurses, with separate, unrelated entries in the patients' records. These notes were used in place of face-to-face discussion or joint ward-rounds. Different teams failed to consult one another when reviewing patients. Occasionally medical officers were called to review urgent cases but were busy in theatre or with accident and emergency (A&E) cases, so no action followed. Thirty-two women died of indirect causes which were deserving of joint obstetric, medical, surgical or intensive care. In 15 (47%) cases, joint management was inadequate. Six women (11%) died at term in the referral hospitals, with no plans for salvage of the babies, who died undelivered.
In 30 (54%) cases, staff did not recognise the severity of the women's illnesses and failed to act promptly on evidence of their worsening conditions. In some cases, nursing notes recorded the deteriorating condition of patients without indicating actions taken. Junior medical officers were slow to intervene, to order urgent investigations or to ask for help from senior staff.
There was insufficient precision in recording history and examination findings. In 17 (30%) records there was no differential diagnosis, leading to missed alternative diagnoses. In 18 cases (32%) the wrong diagnosis was made. There were long intervals between investigations being ordered, being carried out and being reported on without the reasons for delay being noted. In 21 (36%) cases, there was inadequate monitoring of the patient's condition. There was little evidence of adherence to national protocols, such as the referral of grand multigravida to higher levels for delivery, or management of pregnancy-induced hypertension. Sometimes the laboratory result was treated rather than the patient, e.g. a woman who was in a critical and unstable condition had blood withheld because her haemoglobin was above the 8 g/dl threshold for transfusion in stable cases.
Twenty-five (68%) of the 37 women who died in the 2 referral hospitals, each of which has an intensive care unit (ICU), were ill enough to warrant earlier consultation with anaesthetists regarding transfer to the ICU. However, there were delays in requesting physician, anaesthetist or ICU consultations. Eleven (20%) women were in district hospitals, but may have benefitted from specialist advice given by telephone or email.
Health system-related factors
Case notes did not reveal whether advice on preventing pregnancy was given to women at high risk of complications, such as grand multigravida and those with known severe underlying disease. Where pregnant women were severely ill with AIDS or cardiac disease, termination of the pregnancy could have been offered on medical grounds, which is permissible under Botswana law.
In Botswana, HIV management is carried out on an outpatient basis at infectious disease care clinics (IDCCs), while pregnancy is managed by ANC clinics. Each is a separate pathway with separate documentation. Parameters for monitoring HIV progression, such as weight, clinical symptoms and CD4+ counts, were rarely recorded in ANC records. There was no documentation of patient education regarding danger signs related to pregnancy and HIV, (for instance, recommendations to seek urgent care if symptoms such as severe headaches, vomiting, persistent cough or neck pain developed). There was clear evidence of substandard management of women presenting at ANC with symptoms, e.g. cases of a chronic cough or dyspnoea (despite the high risk of tuberculosis (TB) and HIV co-infection), or diarrhoea and dehydration, were not investigated further.
Sixteen (44%) of the HIV-positive women may have benefited from jointly managed IDCC and ANC care, or consultations with HIV specialists. There was under-investigation, under-diagnosis and late treatment of tuberculosis, but over-diagnosis of Pneumocystis carinii pneumonia. Adherence to ART on the part of patients was not recorded. Several supply problems were recorded, e.g. normal saline solution was reported as out of stock. Other shortages included intravenous potassium (two patients had persistent severe hypokalaemia), magnesium sulphate at district hospitals, inotropic drugs in ICU, appropriate antibiotics, reagents for laboratory tests, fluid-giving sets and sterile procedure packs such as those used for uterine evacuation. Several equipment failures were reported, involving X-ray, blood cross-match and blood gas machines.
Of 12 patients who needed blood transfusion peri-operatively, 6 did not receive it, while a further 6 received only 1 unit despite recorded blood losses of 2 litre.
Discussion
Poorly functioning health systems have compromised efforts to improve health in sub-Saharan Africa,[17] even in those better-resourced middle-income countries such as SA and Botswana. This case review shows how maternal deaths highlight opportunities for key institutions - particularly Ministries of Health, but also training and professional bodies - to address underlying deficiencies in the health system.
A culture of continual quality improvement, through regular audits and the implementation of solutions, is crucial for a responsive, strengthened health system. Prevention of maternal deaths in areas with a high HIV-prevalence requires skills development in two directions: first, obstetric skills are required for management of childbirth, prevention of haemorrhage and sepsis, and identifying hypertension early and second, there is increasing need for medical management of HIV in pregnancy and vigilance for medical complications, including those related to ARVs.[18]
In Botswana, most pregnant women have a known HIV status, (except for non-citizens, who are not eligible for free healthcare apart from emergencies). Twenty-one (58%) of the women in the study were already on ART, which, in 2010, was given to those whose CD4+ counts were <250 cells/µl. These women were already very ill during their pregnancy. Many suffered opportunistic infections that had not been detected during antenatal screening. Just over half the deaths occurred in the immediate postnatal period, mainly from indirect causes, showing the need for continued monitoring from antenatal to postnatal periods. In SA there are proposals to reduce maternal deaths through intensified antenatal HIV testing, strengthened HIV services, and providing ART to all HIV-positive pregnant women, regardless of CD4 status;[5,6] this latter has been the revised policy in Botswana since 2012.[19]
This review shows, however, that such intervention alone would be insufficient. It is essential to integrate HIV management for pregnant women into maternal health services, with joint management and co-ordination of pregnancy plans, rather than relying on vertical programmes that rarely intersect. Because cases are more complex, better communication, teamwork and interspeciality consultation is required to anticipate and resolve problems as they develop. The higher mortality experienced by HIV-positive pregnant women in Africa is attributed more to weaknesses in health-service delivery than to the direct biological effects of HIV.[20]
Measures aimed at preventing these avoidable maternal deaths would benefit the health system as a whole, not just HIV or maternal services. In Mozambique, the integration of HIV management into ANC services, and the use of HIV resources to strengthen infrastructure has led to 'system efficiency' through reduced workforce gaps, and improved supervision, patient flows and co-ordination between laboratories, pharmacies and clinics, in ways that have benefited all programmes.[21] In addition, there is a case for the abolition of discriminatory policies which disallow the treatment of non-citizens in pregnancy, so that all pregnant women receive HIV counselling, testing and ART if they are HIVpositive.
Botswana is justifiably proud that more than 90% of pregnant women deliver in health facilities, in the hands of skilled health professionals. However, the WHO definition[14] of 'skilled birth attendant' includes not only proficiency in managing uncomplicated deliveries, but also management and referral of complications as they arise.
Schoon[22] argues that the entity of the skilled midwife, as defined above, is scarce in SA, and moreover, that many medical officers lack the skills to manage obstetric emergencies. Equating all health professionals to skilled birth attendants is incorrect, and those who have received some obstetric training need to update their skills regularly.The current review demonstrates that poor clinical practice will not be resolved through didactic classroom teaching, but requires problem-solving techniques, practical emergency obstetric care training and follow-up mentoring.
Clinical audit and critical incident methods are useful as non-judgemental appraisals of a unit's own experience of errors. As a priority, improving quality of care in the referral hospitals, where the majority of deaths occur, would have an impact on Botswana's MMR. In district facilities, obstetric emergencies are uncommon events, so district health staff could be trained using case studies (such as those in this review) as training scenarios, or using practice drills to determine what actions staff would take.
Conclusion
Preventing maternal deaths requires a new approach that takes account of the impact of HIV in high-prevalence areas. Changing treatment protocols to include all HIV-positive pregnant women in ART programmes may mean that women will not present with AIDS in pregnancy, but this would require well-co-ordinated services that integrate HIV management into maternal health services. Improvements in quality of care and clinical practice, through repeated enquiries into underlying causes of death, are essential. This can be accomplished within existing resources, through improved communication, supervision, teamwork and training, and by ongoing monitoring of the specific underlying causes for each maternal death through a critical incident approach.
Acknowledgements. The study was conducted at the University of Botswana with funding from the US President's Emergency Plan for AIDS Relief (PEPFAR) and the Health Resources and Services Administration (HRSA) under the Medical Education Partnership Initiative (MEPI). The authors thank the health facilities for providing the patient case notes that formed the basis of the study.
References
1. World Bank. Reproductive Health at a Glance. Gaborone, Botswana 2011. Washington, DC: 2004. http://siteresources.worldbank.org/INTPRH/Resources/376374-1282255445143/Botswana52411web.pdf (accessed 11 May 2013). [ Links ]
2. UNAIDS/WHO Working Group on Global HIV/AIDS and STI Surveillance. Botswana 2004 Update: Epidemiological Fact Sheet. Geneva: UNAIDS UNICEF WHO, 2004. http://data.unaids.org/Publications/Fact-Sheets01/botswana_en.pdf (accessed 11 May 2013). [ Links ]
3. Botswana HIV/AIDS Programme. Botswana Sentinel Surveillance, 2001-2009. Gaborone: Ministry of Health, 2012. http://www.hiv.gov.bw/content/hiv-and-aids-statistics (accessed 20 April 2013). [ Links ]
4. Botswana Safe Motherhood Initiative. National Maternal Mortality Audit Committee 2007 Report. Gaborone: Ministry of Health, 2008. [ Links ]
5. Moodley J, Pattinson RC, Baxter C, et al. Strengthening HIV services for pregnant women: An opportunity to reduce maternal mortality rates in southern Africa/sub-Saharan Africa. BJOG 2011;118(2):219-225. [http://dx/doi.org/10.1111/j.1471-0528.2010.02726.x. [ Links ]]
6. Ramogale MR, Moodley J, Sebitloane MH. HIV-associated maternal mortality - primary causes of death at King Edward VIII Hospital Durban. S Afr Med J 2007;97(5):363-366. [ Links ]
7. Grange J, Adhikari M, Ahmed Y, et al. Tuberculosis in association with HIV/AIDS emerges as a major non-obstetric cause of maternal mortality in Sub-Saharan Africa. Int J Gynaecol Obstet 2010;108(3):181-183. [http://dx.doi.org/10.1016/j.ijgo.2009.12.005. [ Links ]]
8. UNAIDS. Countdown to Zero: Global Plan Towards the Elimination of New HIV Infections Among Children by 2015 and Keeping Their Mothers Alive, 2011-2015. Geneva: UNAIDS, 2011. http://www.unaids.org/en/media/unaids/contentassets/documents/ unaidspublication/2011/20110609_JC2137_ Global-Plan -Elimination-HIV-Children_en.pdf (accessed 11 May 2013). [ Links ]
9. Botswana Central Statistical Office and UNICEF. 2007 Botswana Family Health Survey IV Report. Gaborone: Botswana Central Statistical Office and UNICEF, 2009. [ Links ]
10. Botswana Central Statistical Office. Stats Brief Maternal Mortality No.2011/12. Gaborone: Botswana Central Statistical Office, 2011. [ Links ]
11. United Nations Children's Fund. Countdown to Zero: Botswana Report. Geneva: UNICEF, 2012. http://www.unicef.org/aids/files/hiv_pmtctfactsheetBotswana.pdf (accessed 11 May 2013). [ Links ]
12. National AIDS Coordinating Agency & UNAIDS. Progress Report of the National Response to the 2001 Declaration of Commitment on HIV and AIDS, 2008-2009: Botswana Country Report 2010. http://data.unaids.org/pub/Report/2010/botswana_2010_country_ progress_report_en.pdf (accessed 11 May 2013). [ Links ]
13. Scheffler RM, Mahoney CB, Fulton BD, Dal Poz MR, Preker AS. Estimates of health care professional shortages in sub-Saharan Africa by 2015. Health Aff 2009;28(5)w849-w862. [http://dx.doi.org/10.1377/hlthaff.28.5.w849] [ Links ]
14. Pitt C, Greco G, Powell-Jackson T, Mills A. Countdown to 2015: Assessment of official development assistance to maternal, newborn, and child health, 2003-08. Lancet 2010;376(9751):1485-1496. [http://dx.doi.org/10.1016/S0140-6736(10)61302-5] [ Links ]
15. South African Department of Health. Saving Mothers 2008-2010: Fifth report on the confidential enquiry into maternal deaths in South Africa. Pretoria: Government Printer; 2012. http://www.doh.gov.za/docs/reports/2012/Report_on_Confidential_Enquiries_i nto_Maternal_Deaths_in_South_Africa.pdf (accessed 11 May 2013). [ Links ]
16. World Health Organization. Making Pregnancy safer: The critical role of the skilled attendant. Joint statement by WHO, ICM and FIGO. Geneva:WHO, 2004. [ Links ]
17. Thomas LS, Jina R, Tint KS, Fonn S. Making systems work: The hard part of improving maternal health services in South Africa. Reprod Health Matters 2007;15(30):38-49 [http://dx.doi.org/10.1016/S0968-8080(07)30314-5] [ Links ]
18. Chweneyagae D, Delis-Jarrosay N, Farina Z, et al The impact of HIV infection on maternal deaths in South Africa. South African Journal of Obstetrics and Gynaecology 2012;18(3):70-76. [http://dx.doi. org/10.7196/SAJOG.581] [ Links ]
19. Botswana Ministry of Health. 2012 Botswana National HIV&AIDS Treatment Guidelines. Gaborone: Ministry of Health, 2012. [ Links ]
20. Gray GE, McIntyre JA. HIV and pregnancy. BMJ 2007;334(7600):950-953. [http://dx.doi.org/10.1136/bmj.39176.674977.AD] [ Links ]
21. Pfeiffer J, Montoya P, Baptista AJ et al Integration of HIV/AIDS services into African primary health care: Lessons learned for health system strengthening in Mozambique - a case study. J Int AIDS Soc 2010;13:3. [http://dx.doi.org/10.1186/1758-2652-13-3] [ Links ]
22. Schoon MG, Motlolometsi MW. Poor maternal outcomes: A factor of poor professional systems design. S Afr Med J 2012;102(10):784-786. [http://dx.doi.org/10.7196/SAMJ.6130] [ Links ]
Accepted 14 May 2013
 Correspondence: S Ray (sunanda28@hotmail.com)
Correspondence: S Ray (sunanda28@hotmail.com)














