Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.103 no.2 Pretoria Fev. 2013
FORUM
ISSUES IN MEDICINE
The 2011 United Nations High-Level Meeting on Non-Communicable diseases: The Africa agenda calls for a 5-by-5 approach
G A Mensah; B M Mayosi
Affiliated with the Department of Medicine at Groote Schuur Hospital and the University of Cape Town
ABSTRACT
The High Level Meeting of the 66th Session of the United Nations General Assembly was held in September 2011. The Political Declaration issued at the meeting focused the attention of world leaders and the global health community on the prevention and control of non-communicable diseases (NCDs). The four major NCDs (cardiovascular diseases, cancer, diabetes and chronic respiratory diseases) and their four risk factors (tobacco use, unhealthy diet, physical inactivity and harmful use of alcohol) constitute the target of the '4-by-4' approach, which is also supported by national and international health organisations.
We argue that while preventing these eight NCDs and risk factors is also important in Africa, it will not be enough. A '5-by-5' strategy is needed, addressing neuropsychiatric disorders as the fifth NCD; and transmissible agents that underlie the neglected tropical diseases and other NCDs as the fifth risk factor. These phenomena cause substantial preventable death and disability, and must therefore be prioritised.
The United Nations (UN) General Assembly High Level Meeting (HLM) on Non-Communicable Diseases (NCDs), was held in New York on 19 and 20 September 2011.
It provided a unique opportunity to prioritise NCDs as a global health challenge of enormous proportions, with significant societal, economic and developmental implications.1 This meeting focused attention on the prevention and control of NCDs, especially in low- and middle-income countries, where nearly 80% of global NCD mortality occurs.
The priority actions identified at the HLM could lead to a sustained global movement against preventable death, disease and disability from NCDs, especially cardiovascular diseases, cancer, diabetes and chronic respiratory disease.2,3 Accordingly, the World Health Organization (WHO),4 several health professional associations5 and the Political Declaration6 issued at the end of the HLM on NCDs have all called for a strategy addressing these four diseases and their four shared risk factors (tobacco use, unhealthy diet, physical inactivity and harmful use of alcohol).
It is well established that these major NCDs and their related risk factors are an urgent matter globally. Even in sub-Saharan Africa, where these NCDs and risk factors are not yet the leading causes of death or disability, trends portend a significant increase in NCD burden and related preventable death by 2030.7 Recent improvements in economic development, increasing urbanisation, increasing marketing of tobacco and marked shifts in dietary intake patterns are all likely to fuel the emergence of these chronic NCDs and associated mortality in Africa.8 For example, age-standardised prevalence of hypertension and mortality from stroke are already higher in Africa than in most other WHO regions.9,10
Importantly, Ezzati et al.11 have shown that controlling 20 major risk factors can potentially increase healthy life expectancy by up to 16.1 years (a 43% increase) in parts of sub-Saharan Africa.11
However, preventing cardiovascular diseases, cancer, diabetes, and chronic respiratory disease - and alleviating their related risk factors - will not be enough. Neuropsychiatric and mental disorders must be prioritised as the fifth major NCD; the fifth major risk factor must be acknowledged as the group of infections that predispose to neglected tropical diseases and other NCDs, causing substantial chronic disability, life-long impairments and preventable death. Thus, the Africa agenda calls for a 5-by-5 approach.
Mental health, neurological and substance use disorders in Africa
More than a decade ago, the WHO called attention to the high burden of disease and disability due to neuropsychiatric and mental disorders in Africa.12 In its regional strategy for mental health in the Africa Region for the years 2000 - 2010, the WHO also highlighted the increasing burden of poverty, natural disasters, social upheaval, and wars and other forms of violence as major causes of the growing psychosocial problems, which are often compounded by harmful use of alcohol and other substances.12
In the decade since these observations, little has changed in much of Africa. Most African countries, except South Africa, still have no policies, programmes, or action plans for the prevention and control of neuropsychiatric disorders,13 despite projections that the burden of neuropsychiatric and mental disorders is likely to increase.7
Recently, the extensive challenges Africa faces in preventing and controlling Mental health, neurological and substance use (MNS) disorders were highlighted again, in a workshop jointly organised by the US Institute of Medicine Forum on Neuroscience and Nervous System Disorders and the Uganda National Academy of Sciences Forum on Health and Nutrition.14
MNS disorders are estimated to account for approximately 350 million disability-adjusted life years (DALYs) lost per year in sub-Saharan Africa - a burden that is significantly greater than that seen in developed countries at 150 million DALYs per year.14 Yet the infrastructure and manpower to address prevention, detection, evaluation and treatment is inadequate.
Most sub-Saharan African countries have less than 1 psychiatrist per 1 million people, and even fewer neurologists.15 A similarly grim manpower scarcity exists for psychiatric nurses, psychologists and trained social workers. Appropriate medications are scarce and, in the rare cases that they are available, access and affordability remain very limited. These challenges are compounded by weak primary healthcare and treatment systems and a high level of stigmatisation of mental health disorders, in a policy environment that continues to neglect NCDs.
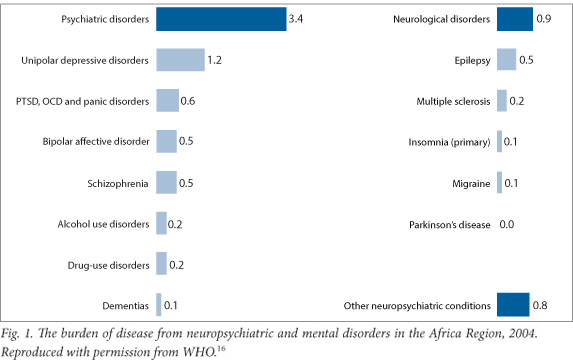
As shown in Fig. 1, the leading psychiatric disorders underlying Africa's disease burden include unipolar depressive disorders, post- traumatic stress, panic disorders, bipolar affective disorders and schizophrenia.16 Among the neurological disorders, by far the most prevalent cause of disability is epilepsy, typically caused by birth trauma, childhood infections and head injury in later life.14,16
While these MNS disorders are not leading causes of mortality, they do cause significant disability. To adequately tackle the inherent challenges, the UN HLM should facilitate substantial investments, allowing effective and strategic integration of mental healthcare into overall national health sector reform plans.13 Recently Jenkins et al.17 pointed out that it will be crucial to engage professionals with expertise in MNS disorders, and to intensively mobilise resources to address these disorders as economic and developmental challenges.17
Although significant new resources will have to be invested, the absolute amount is not large when viewed in light of other health investment strategies.18 Chisholm et al. have shown that the cost per capita (in US dollars) of providing the core package of interventions at target coverage levels ranged from $1.85 to $2.60 per year in low-income countries, compared with $3.20 to $6.25 per year in lower-middle-income countries.18 In a more recent analysis, the authors demonstrate the cost-effectiveness of a wide range of possible interventions that could be undertaken in sub-Saharan Africa, with the cost per year of healthy life varying from many multiples to just a fraction of average per capita income.19 More importantly, their data show that reallocating current resources to more cost-effective intervention strategies would not only save money, but also increase the health gain and help expand much-needed neuropsychiatric services in the sub-Saharan African setting.19
The UN HLM has a unique opportunity to foster a broader view of MNS disorders as a major cause of morbidity and an impediment to economic and social development in Africa. To do this requires: facilitating the development or renewal and enforcement of mental health legislation in Africa; working to secure the human rights of persons with MNS disorders; raising awareness and education about MNS disorders in order to dispel myths and associated stigmas; supporting partnerships between African national and international neurologic and psychiatric associations and their affiliation to the World Psychiatric Association; and identifying appropriate roles for traditional healers while supporting appropriate integration of the prevention and control of MNS disorders within the primary healthcare setting.
To integrate mental health into national healthcare programmes, a pivotal step will be acknowledging the links between MNS disorders and infections since, in many African countries, cerebral complications of malaria, typhoid fever, and HIV are the most frequent causes of acute or subacute psychoses. Although typically causing only temporary disability, these complications can lead to significant disability and death if not promptly and adequately treated. Such integration would recognise the human, laboratory and other technical expertise in communicable diseases that Africa has developed over the past two decades and, importantly, would leverage them for the prevention and control of NCDs.
Infections as major risk factors for NcDs in Africa
Infections play a primary aetiological role in many chronic NCDs that are endemic in sub-Saharan Africa, such as rheumatic heart disease, liver cancer, cervical cancer and HIV-related dementia. Taken together, these infections cause substantial chronic disability, life-long impairments and lost national income. It is therefore appropriate to prioritise them as the fifth major risk factor for the post-UN HLM agenda, to be addressed by the WHO and the public health community.
The neglected tropical diseases (NTD) afflict an estimated 1 billion people, most of whom live in Africa and are among the poorest in the world,20,21 causing significant disability and impairing quality of life. In the Global Burden of Disease assessment, the major NTDs include trypanosomiasis, Chagas disease, schistosomiasis, leishmaniasis, lymphatic filariasis, onchocerciasis, intestinal nematode infections, Japanese encephalitis, dengue and leprosy. These accounted for an estimated 177 000 deaths worldwide in 2002, mostly in sub-Saharan Africa, and about 20 million DALYs, or 1.3% of the global burden of disease and injuries.22 NTDs have largely been ignored on the global health policy agenda,23 despite effective prevention, treatment and control programmes.
Recurrent streptococcal infection, the cause of rheumatic fever and rheumatic heart disease (RHD) and kidney disease, represents another major infectious risk factor for NCD in Africa. As pointed out in the Drakensberg Declaration,24 as many as half of the 2.4 million children globally affected by RHD live in Africa, and a major proportion of all cardiovascular disease in children and young adults in Africa is attributable to rheumatic fever. The impact on economic productivity in African countries is substantial.25
Many infections are also important contributors to the burden and sequelae of major NCDs through triggering acute exacerbations and hospitalisations.26,27 For example, tuberculosis (TB) can aggravate blood glucose control and trigger diabetes,27 as well as aggravating the social and financial stress that contributes to substance abuse and mental illness.28
In some settings, infections may also be causally linked to NCDs.29 For example, malaria in pregnancy is an important cause of fetal malnutrition and intrauterine growth retardation in Africa, and can indirectly serve as a risk factor for the development of obesity, type 2 diabetes, cardiovascular diseases and sickle cell disease.29 Appropriate prenatal care can therefore be an effective intervention for the prevention of NCDs.
Population-wide vaccination interventions can be another effective strategy for NCD prevention in Africa. For example, vaccination against hepatitis B, a major cause of liver cancer, is now considered a 'best buy' and vaccination against human papillomavirus (HPV), the main cause of cervical cancer, is also recommended.9
A history of pulmonary tuberculosis (PTB) is among the leading causes of bronchiectasis, and a powerful risk factor for chronic obstructive pulmonary disease (COPD) in Africa.13 In a national household survey of adults in South Africa, Ehrlich et al.30 showed that a history of PTB is the strongest predictor of chronic bronchitis, with an odds ratio of 4.9 (95% CI 2.6 - 9.2) for men and 6.6 (95% CI 3.7 - 11.9) for women.30 While the overall prevalence of chronic bronchitis was 2.3% in men and 2.8% in women, the risk of chronic bronchitis was more strongly associated with TB than with tobacco smoking or exposure to smoke from biomass fuel. This suggests that, in Africa, PTB is a powerful risk factor for COPD.30
As previously noted, infections also play an important role in MNS disorders.14
Conclusion
Sub-Saharan African populations are in the midst of a health transition characterised by the simultaneous occurrence of epidemic infectious diseases and a rise in NCDs. There is direct interaction between infectious risk factors and chronic diseases, such as HPV and cervical cancer; Streptococcus pyogenes and rheumatic heart disease; TB and chronic lung disease; and HIV and dementia.
The link between infectious risk factors, NCDs and neuropsychiatric illness has a direct bearing on the appropriate agenda for the prevention and control of chronic diseases in sub-Saharan Africa. There is a need to add the fifth risk factor (transmissible agents) and a fifth condition (neuropsychiatric illness) to the agenda for the prevention and control of NCDs in Africa. A 5-by-5 strategy that recognises 5 risk factors (tobacco smoking, unhealthy diet, physical inactivity, excessive alcohol use and transmissible agents) and 5 diseases (cardiovascular disease, chronic lung disease, diabetes, cancer and neuropsychiatric illness) is required to combat NCDs in sub-Saharan Africa.
This 5-by-5 approach is consistent with the language and intent of the WHO Africa regional ministerial consultation on the prevention and control of NCDs, held in Brazzaville, Congo, in the months leading up to the UN HLM.31,32
References
1. United Nations. High-level Meeting on Non-communicable Diseases. New York: UN, 2011. http://www.un.org/en/ga/president/65/issues/ncdiseases.shtml (accessed 31 August 2012). [ Links ]
2. Beaglehole R, Bonita R, Horton R, et al. Priority actions for the non-communicable disease crisis. Lancet 2011;377(9775):1438-1447. [http://dx.doi.org/10.1016/S0140-6736(11)60393-0] [ Links ]
3. The NCD Alliance. Proposed Outcomes Document for the United Nations High-Level Summit on Non-Communicable Diseases. New York: NCD Alliance, 2011. http://www.ncdalliance.org (accessed 10 June 2011). [ Links ]
4. World Health Organization. 2008-2013 Action Plan for the Global Strategy for the Prevention and Control of Noncommunicable Diseases. Geneva: WHO, 2008. http://www.who.int/nmh/publications/ncd_action_plan_en.pdf (accessed 31 August 2012). [ Links ]
5. The NCD Alliance. NCD Alliance Plan for the United Nations Summit on Non-Communicable Diseases. New York: NCD Alliance, 2010. http://www.idf.org/webdata/NCD-Alliance-Plan.pdf (accessed 31 August 2012). [ Links ]
6. United Nations. Political Declaration of the High-level Meeting of the General Assembly on the Prevention and Control of Non-Communicable Diseases. New York: UN, 2011. [ Links ]
7. Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 2006;3(11):e442. [http://dx.doi.org/10.1371/journal.pmed.0030442] [ Links ]
8. Bourne LT, Lambert EV, Steyn K. Where does the black population of South Africa stand on the nutrition transition? Public Health Nutr 2002;5(1A):157-162. [http://dx.doi.org/10.1079/PHN2001288] [ Links ]
9. World Health Organization. Global Status Report on Noncommunicable Diseases 2010. Geneva: WHO, 2011. [ Links ]
10. Strong K, Mathers C, Bonita R. Preventing stroke: saving lives around the world. Lancet Neurol 2007;6(2):182-187. [http://dx.doi.org/10.1016/S1474-4422(07)70031-5] [ Links ]
11. Ezzati M, Hoorn SV, Rodgers A, Lopez AD, Mathers CD, Murray CJ. Estimates of global and regional potential health gains from reducing multiple major risk factors. Lancet 2003;362(9380):271-280. [ Links ]
12. World Health Organization Regional Office for Africa. Regional Strategy for Mental Health 2000-2010. Brazzaville: WHO, 2000. [ Links ]
13. Mayosi BM, Flisher AJ, Lalloo UG, Sitas F, Tollman SM, Bradshaw D. The burden of non- communicable diseases in South Africa. Lancet 2009;374(9693):934-947. [http://dx.doi.org/10.1016/S0140-6736(09)61087-4] [ Links ]
14. Institute of Medicine (US) Forum on Neuroscience and Nervous System Disorders, Uganda National Academy of Sciences Forum on Health and Nutrition. Mental, Neurological, and Substance Use Disorders in Sub-Saharan Africa: Reducing the Treatment Gap, Improving Quality of Care: Workshop Summary. Washington DC: National Academies Press, 2010. [ Links ]
15. Okasha A. Mental health in Africa: the role of the WPA. World Psychiatry 2002;1(1):32-35. [ Links ]
16. World Health Organization. Regional Office for Africa. Health Situation in the African Region: Atlas of Health Statistics. Geneva: WHO, 2011. [ Links ]
17. Jenkins R, Baingana F, Belkin G, et al. Mental health and the development agenda in Sub-Saharan Africa. Psychiatr Serv 2010;61(3):229-234. [http://dx.doi.org/10.1176/appi.ps.61.3.229] [ Links ]
18. Chisholm D, Lund C, Saxena S. Cost of scaling up mental healthcare in low- and middle-income countries. Br J Psychiatry 2007;191:528-535. [http://dx.doi.org/10.1192/bjp.bp.107.038463] [ Links ]
19. Chisholm D, Saxena S. Cost effectiveness of strategies to combat neuropsychiatric conditions in sub- Saharan Africa and South East Asia: mathematical modelling study. BMJ 2012;344:e609. [http://dx.doi.org/10.1136/bmj.e609] [ Links ]
20. World Health Organization. First WHO Report on Neglected Tropical Diseases: Working to Overcome the Global Impact of Neglected Tropical Diseases. Geneva: WHO, 2010. http://whqlibdoc.who.int/ publications/2010/9789241564090_eng.pdf (accessed 31 August 2012). [ Links ]
21. Zhang Y, MacArthur C, Mubila L, Baker S. Control of neglected tropical diseases needs a long-term commitment. BMC Med 2010;8:67. [http://dx.doi.org/10.1186/1741-7015-8-67] [ Links ]
22. Mathers CD, Ezzati M, Lopez AD. Measuring the burden of neglected tropical diseases: the global burden of disease framework. PLoS Negl Trop Dis 2007;1(2):e114. [http://dx.doi.org/10.1371/journal.pntd.0000114] [ Links ]
23. Liese B, Rosenberg M, Schratz A. Programmes, partnerships, and governance for elimination and control of neglected tropical diseases. Lancet 2010;375(9708):67-76. [http://dx.doi.org/10.1016/S0140-6736(09)61749-9] [ Links ]
24. Mayosi B, Robertson K, Volmink J, et al. The Drakensberg declaration on the control of rheumatic fever and rheumatic heart disease in Africa. S Afr Med J 2006;96(3):246. [ Links ]
25. Robertson KA, Mayosi BM. Rheumatic heart disease: social and economic dimensions. S Afr Med J 2008;98(10):780-781. [ Links ]
26. Creswell J, Raviglione M, Ottmani S, et al. Tuberculosis and noncommunicable diseases: neglected links and missed opportunities. Eur Respir J 2011;37(5):1269-1282. [http://dx.doi.org/10.1183/09031936.00084310] [ Links ]
27. World Health Organization, International Union Against Tuberculosis and Lung Disease, World Diabetes Foundation. Report from the Expert Meeting on Tuberculosis and Diabetes Mellitus. Geneva: WHO, 2009. [ Links ]
28. Sweetland A, Acha A, Guerra D. Enhancing Adherence: the Role of Group Psychotherapy in the Treatment of MDR-TB in Urban Peru. In: Cohen A, Kleinman A, Saraceno B, eds. World Mental Health Casebook: Social and Mental Health Programmes in Low-Income Countries. New York: Kluwer Academic Press, 2002:57-85. [ Links ]
29. Ogoina D, Onyemelukwe GC. The role of infections in the emergence of non-communicable diseases (NCDs): Compelling needs for novel strategies in the developing world. J Infect Public Health 2009;2(1):14-29. [http://dx.doi.org/10.1016/j.jiph.2009.02.001] [ Links ]
30. Ehrlich RI, White N, Norman R, et al. Predictors of chronic bronchitis in South African adults. Int J Tuberc Lung Dis 2004;8(3):369-376. [ Links ]
31. World Health Organization Regional Office for Africa. WHO African Regional Ministerial Consultation on Non-Communicable Diseases; Brazzaville, Congo, 4 - 6 Apri 2011; Background Document. Brazzaville: WHO, 2011. [ Links ]
32. World Health Organization Regional Office for Africa. The Brazzaville Declaration on Noncommunicable Diseases Prevention and Control in the WHO African Region. Brazzaville: WHO, 2011. [ Links ]
Accepted 4 October 2012
 Corresponding author:
Corresponding author:
B M Mayosi (bongani.mayosi@uct.ac.za)














