Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.103 n.2 Pretoria Feb. 2013
IZINDABA
MSF again paves the way with ART
Chris Bateman
Médecins Sans Frontières (MSF) has once again paved the way in local HIV/AIDS treatment, this time piloting ART adherence clubs in Khayelitsha outside Cape Town, improving adherence (and thus sustained virological suppression and immunological recovery) over mainstream care by a full 12%.
Not only does the project, now involving 4 505 patients in some 150 'clubs' operating out of nine health facilities, reduce the patient load in mainstream care, enabling clinicians to better concentrate on new and relapsed patients, it also saves the health system and patients invaluable time and money. The collaboration between MSF, the Western Cape Department of Health and the Treatment Action Campaign (TAC) won a platinum award from the prestigious Impumelelo Social Innovations Centre and drew sustained applause when presented at the first-ever Southern African HIV Clinicians Society Conference in Cape Town late last year.
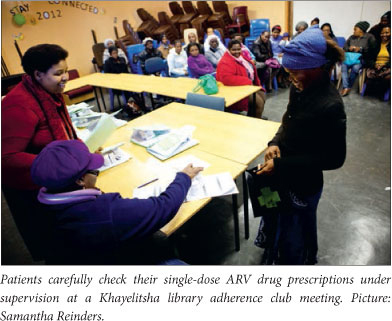
Setting up ART clubs within walking distance of the club members' homes (most often in one of the member's homes) is the end goal, but in the interim community facilities such as church and community halls and libraries are proving to be solid stepping stones and hugely effective. So far the clubs have reached 50% transition to full decentralisation and meet once every two months (the aim for optimal efficiency is to meet every three months).
A major boost for the club model has been the national health department shift to fixed-dose combinations (FDCs) in ART, considerably reducing the burden on clinic pharmacies to pre-pack or check pre-packs from the central dispensing service. MSF medical co-ordinator for South Africa and Botswana, Dr Gilles von Cutsem, said that for South Africa's 1.7 million people on ARVs, the FDC's formulations in the 2012 - 2014 supply tender cut down the daily pill burden of 3 - 5 pills to just 1 pill, hugely enhancing the chances of life-long adherence. By simplifying the first-line adherence regimen not only were adherence clubs made more possible but prevention of mother-to-child HIV transmission (PMTCT) treatment options were expanded. FDC simplified the delivery of ART to pregnant women as soon as they tested positive, eliminating the need for infants to receive nevirapine syrup for the duration of breastfeeding because they were now protected through their mothers taking ARVs. Von Cutsem added that the changes (which include negotiating the world's lowest price for ARVs by a country that consumes 21% of the world's ARVs) made the ambitious target of getting 3 million people on ART by 2015 suddenly seem more achievable.
Success depends on upping staffing levels
Among several vital lessons learnt with the ART adherence clubs first piloted in Khayelitsha two years ago is that the cohort of patients divested into the club model remains the responsibility of the ART service. This requires sufficient human resources to support and run the clubs and cannot drain current facility staffing as the clubs expand. Says Van Cutsem, 'where a facility rolls out more than a few clubs, club preparation and facilitation becomes a substantial role and using existing facility counsellors jeopardises their responsibilities towards ART preparation counselling, counselling non-adherent patients and tracing defaulters. Similarly, increasing your ART patients puts additional pressure on pharmacy staff. We recommend that additional club facilitator and pharmacy assistant posts be created and funded within the facility, NPO or primary healthcare team.' The original pilot programme clearly demonstrated that club participation was associated with sustained virological suppression and immunological recovery and, after 40 months, 97% of club patients remained in care compared with 85% of those who qualified for clubs but remained in mainstream care. Club participants were 67% less likely to experience virological rebound. Von Cutsem said club eligibility centred on an ART patient being stable, clinically well and adhering to treatment. Clinicians used the following criteria: an adult patient of more than 40 kg no longer requiring dosage change according to weight change; on the same ART regimen for at least 12 months; their most recent consecutive viral loads being undetectable; and having no medical condition requiring regular clinical consultations. Club sessions were structured to ensure that blood probes and annual clinical consultation and twice-yearly annual scripting were aligned for all club members, thus optimising efficiency and allowing the hub facility to plan when additional nurse support would be required. Club membership would be ended if the patient was found to have a viral load above 400, other safety blood results were 'significantly abnormal', developed TB, changed their ART regimen for clinical reasons or any other indications in the individual annual clinical follow-up. Membership could be resumed once the patient was adjudged clinically stable again.
A doctor's perspective ...
Dr Musaed Abrahams of the hugely stretched Ubuntu Clinic in Khayelitsha summed up initial clinician sentiment about the club system this way: 'My day is spent seeing many patients who are otherwise well and stable on treatment. My time would be more usefully spent focusing on starting new patients on ART and giving more time to my patients who are not doing well on their treatment. As the pressure on the health system increases, retention in care and adherence of patients on ART decrease.' The national numbers dramatically illustrate his widely shared views: there were 1.79 million patients initiated on ART by mid-2011 - with retention in care estimated at less than 60% at four years. South Africa's National Strategic Plan for 2012 - 2016 targets 80% of all patients eligible on ART by 2016 (more than 3 million people), with 70% retained in care five years after treatment initiation. The escalation of ART initiation over the last five years has shifted South Africa from a lingering global AIDS treatment pariah to universal admiration, but the country does not have the necessary capacity to double patient loads while managing an increasing number of patients at risk of failing their treatment. This is where the MSF intervention is proving to be worth its weight in gold.
From a patient perspective the ART club model is a godsend, enabling job stability (taking a day off work every month to attend the clinic can create touchy employers), with quick access to ART and clinical back-up as needed.
The MSF's Khayelitsha programme was the first in South Africa to provide ART at primary care level in the public sector, flying courageously in the face of government AIDS denialism, obfuscation and treacle-slow concessions during the controversial health ministry tenure of the late Dr Manto Tshabalala-Msimang. It is also one of two pilot projects in the country to provide decentralised care for drug-resistant tuberculosis.















