Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.102 no.12 Pretoria Jan. 2012
RESEARCH
Avoid adding insult to injury - correct management of sick female endurance athletes
T Hew-ButlerI; J BoulterII; R BhoratIII; T D Noakes
ISchool of Health Science, Oakland University, Rochester, MI, USA
IIChief Medical Officer, Comrades Marathon, Scottsville, Pietermaritzburg
IIIVincent Pallotti Hospital, Cape Town
IVMRC/UCT Research Unit for Exercise Science and Sports Medicine and Department of Biology, University of Cape Town
ABSTRACT
OBJECTIVES: To evaluate the efficacy of Ringer's lactate, isotonic saline and hypertonic saline on the clinical and biochemical recovery of athletes with exercise-associated hyponatraemic encephalopathy caused by fluid overload.
METHODS: We retrospectively reviewed serial blood sodium concentrations (Na+) and qualitative signs of recovery and time to recovery in two healthy menstruant females hospitalised with dilutional exercise-associated hyponatraemic encephalopathy after withdrawal from the 2011 Comrades Marathon (89 km) and Argus Cycle Tour (109 km).
RESULTS: Improvements in blood Na+ did not occur with intravenous administration of Ringer's lactate solution, but did occur with administration of isotonic and hypertonic saline. Qualitative improvements in mental status were not quantitatively related to the biochemical value of blood Na+ or subsequent return to normonatraemia.
CONCLUSIONS: Hyponatraemia should be suspected in all female athletes presenting to the medical area of endurance races with vomiting, altered mental status and a history of high fluid intake. If a diagnosis of exercise-associated hyponatraemia with cerebral encephalopathy is confirmed, the treatment of choice is administration of an intravenous bolus of hypertonic saline. Administration of Ringer's lactate should be discouraged, as this does not correct Na+ and appears to delay recovery.
Exercise-associated hyponatraemia (EAH) in South African endurance athletes had become rare since it was first described in three Comrades Marathon runners in 1985.1 Since that report, educational steps highlighting the potential hazards of overdrinking during endurance exercise minimised the incidence and morbidity of EAH in South African endurance races.2-4 However, recently two severe cases of EAH have come to our attention (case 1 from the Comrades Marathon and case 2 from the Argus Cycle Tour) that highlight the need to disseminate the latest evidence-based information, particularly with regard to optimal treatment strategies for EAH.
Case reports
Case 1
A healthy 28-year-old woman with an unremarkable past medical history and on no medications, running her second 89 km Comrades Marathon, pulled out at 76 km in ~10.5 hours feeling dizzy and weaving across the road. During the race she had followed her normal practice of ingesting a GU packet with 200 ml of water every 45 minutes along with Coke and water ad libitum for an estimated fluid consumption rate of ~550 ml/h. She said that she had passed urine four times during the race of 'good volume', the last time just under half way (40 km). She had trained exactly the same as the year before (when she had completed the race in a time of 11 hours and 48 minutes), was not injured, and did not take any medications immediately before or during the race. Two weeks before the race, however, she was diagnosed with sinusitis and dispensed ciprofloxacin, the last dose of which was taken two days before the start of the race. She felt well enough to run on race day.
She remembers lying down at the aid station before becoming confused; she then vomited and suffered a grand mal seizure. She was transported via ambulance to the local hospital where a diagnosis of hyponatraemia was confirmed, with a serum sodium concentration of 112 mmol/l associated with pulmonary oedema (bilateral lung crackles) and encephalopathy (Glasgow Coma Scale (GCS) score of 9/15). She was quickly intubated, given a 40 mg bolus of furosemide plus 5 mg diazepam intravenously, and transported to the local intensive care unit (ICU).
In hospital she had three more seizures and was given Ringer's lactate (250 ml/h), potassium chloride (KCl: 2 ampoules in 200 ml 0.9% saline) and sodium bicarbonate (8.5% for metabolic acidosis). A chest X-ray showed an infiltrate in the right upper lobe. Initial biochemical analyses revealed the following blood concentrations (reference ranges in brackets): sodium (Na+) 114 mmol/l (136 - 145 mmol/l); potassium (K+) 3.4 mmol/l (3.5 - 5.1 mmol/l); chloride (Cl-) 78 mmol/l (98 - 107 mmol/l); bicarbonate (BIC) 11 mmol/l (22 - 29 mmol/l); urea 3.4 mmol/l (1.7 - 8.3 mmol/l); creatinine (creat) 93 µmol/l (49 - 90 µmol/l), creatine phosphokinase (CK) 2 699 U/l (26 - 192 U/l); and white blood cell count (WBC) 23.7x109/1 (3.9 - 9.8x109/l). Nine hours later, the values were as follows: Na+ 116 mmol/l; K+ 3.8 mmol/l; Cl- 85 mmol/l; BIC 19 mmol/l; urea 2.7 mmol/l; and creat 65 umol/l. The patient was then switched to 0.9% saline rehydration (200 ml/h) on day 2, presumably in response to minimal clinical and biochemical progress.
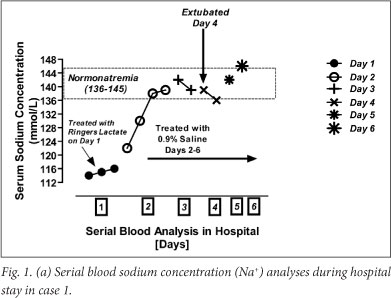
With administration of 0.9% saline, a return to 'normal' blood Na+ was achieved 18 hours later (Fig. 1a), which was associated with an accumulated positive fluid balance of 2.9 litres (Fig. 1b). By day 4, the accumulated positive fluid balance was 6.3 litres (Fig. 1b), in response to which a 20 mg bolus of furosemide was administered every 6 hours. The patient was extubated on day 4, and urinated copiously on day 5 (Fig. 1a); a documented increase in blood Na+ to 146 mmol/l (hypernatraemia) was documented on day 6 (discharge). An overall accumulated fluid balance of 3.7 litres was noted at discharge. Interestingly, blood CK (day 2 = 10 911 U/l, day 3 = 35 731 U/l, and day 4 = 36 832 U/l) continued to increase through day 4 despite normal creatinine and urea concentrations and calculated glomerular filtration rates (eGFR >90 ml/min).

Case 2
A 25-year-old woman with a past medical history of asthma controlled with salbutamol and recurrent migraines controlled with magnesium salts pulled out of the 109 km Argus Cycle Tour at 55 km after ~3 hours of riding. She trained intermittently but had completed a 21 km footrace 2 years earlier. Upon waking, she drank 1 250 ml of fluid and urinated twice before arriving at the race start, where she drank another 1 250 ml of fluid. She continued to drink 1 250 ml/h, mostly bottled water with one glass of Coke, until stopping at the 55 km medical station to rest. She told medical personnel that her arms and legs felt 'tingly' along with a headache, nausea and extreme fatigue. She fell asleep and woke just as the medical crews were preparing to leave. A paramedic agreed to take her home. While being driven, she vomited and experienced mental status change, and was immediately taken to the nearest hospital (hospital 1) (Table 1).
On admission she was diagnosed with 'dehydration' despite no blood parameters being measured and was promptly treated with 1 600 ml of Ringer's lactate. Her level of consciousness on arrival was 8/15 on the GCS, but it deteriorated and she was transported to a larger hospital (hospital 2) 1 hour later. At hospital 2 she had a subnormal temperature, was combative and vomiting, and was intubated to protect her airway. Blood tests confirmed the diagnosis of hyponatraemia (blood Na+ 124 mmol/l) and a computed tomography scan confirmed cerebral oedema. Intravenous fluid therapy was immediately ceased and she was given a 25 ml bolus of 5% saline. The 5% saline was continued at a rate of 75 ml/h for the first 4 hours and then increased to 100 ml/h for the next 12 hours or until normonatraemia was achieved (blood Na+ 135 mmol/l). She began to diurese, producing urine at a rate of 300 - 800 ml/h for the next 48 hours (urine output data not available). She was extubated 4 days after admission and discharged from hospital on the 5th day with short-term memory loss and difficulties in speech (Table 1). She eventually regained full memory and speech and at the time of writing was training for a 10 km race with no apparent residual adverse effects.
Discussion
These two life-threatening cases of EAH with encephalopathy (EAHE) in two signature South African endurance races in 2011 highlight the need to revisit the most appropriate diagnosis and treatment strategies for EAH and EAHE. The EAH Consensus Statement5 and Noakes et at.6 include the two main risk factors for EAHE: (i) menstruant females moving at a pace slower than the average for most competitors; and (ii) a history of high fluid intake during the race. When coupled with signs and symptoms of vomiting, bloating, weight gain and altered mental status, these factors should immediately suggest a diagnosis of dilutional hyponatraemia in endurance athletes. Medical personnel handling such patients should immediately measure the blood electrolyte concentration whenever faced with such 'classic' EAH presentations as these.
When a diagnosis of dilutional EAHE is confirmed, the most appropriate and life-saving treatment strategy is prompt administration of an intravenous bolus of hypertonic saline.5 Such treatment is critical to reduce cerebral oedema and prevent morbidity and mortality associated with brainstem herniation.7 The risk of central pontine myelinolysis (CPM) associated with such treatment is low when EAH is treated in this way. EAH is an acute hyponatraemia, and there have been no reported cases of CPM in athletes. A 1 - 2% reduction in cerebral oedema associated with administration of a bolus of 100 ml 3% hypertonic saline reverses EAHE within a few minutes of treatment.8 The increase in blood Na+ associated with a 100 ml bolus of 3% saline is marginal (1 - 2%), whereas the symptomatic response can be dramatic.
These two cases also illustrate the point that blood sodium concentrations do not always predict the severity of symptoms or response to treatment. Case 1, for example, had a far lower blood Na+ level (112 mmol/l) than case 2 (124 mmol/l) on admission. However, case 2's symptoms were more severe and her recovery more prolonged. Current recommendations are to treat the symptoms first in lieu of treating the actual blood sodium value in athletes diagnosed with EAH and EAHE.5
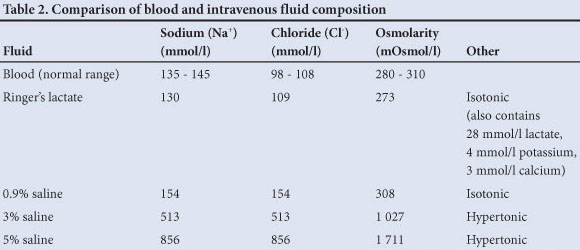
In contrast to these current treatment guidelines for EAHE, administration of isotonic fluids such as Ringer's lactate and isotonic saline (0.9%) has repeatedly been demonstrated to prolong recovery9,10 and result in poorer outcomes.7 Both cases 1 and 2 were initially treated with Ringer's lactate. In case 1 neither symptoms nor blood Na+ improved with such treatment (Fig. 1a), while in case 2 the symptoms worsened appreciably (Table 1), GCS declining from 8/15 to 3T/15). Table 2 compares the ionic composition of commonly used intravenous fluids in critical care settings and highlights the improved mathematical efficacy of hypertonic versus isotonic saline solutions in raising blood Na+. Isotonic fluid administration is further discouraged in hyponatraemic patients with inappropriate arginine vasopressin secretion. In the syndrome of inappropriate antidiuretic hormone secretion (SIADH), most of the sodium that is administered intravenously is promptly excreted because of the natriuresis that accompanies SIADH.11 This concept was hypothetically supported in case 2, in which there was a clear diagnosis of SIADH (as demonstrated with an initial urine Na+ level of 189 mmol/l and urine osmolality of 788 mOsmol/kg H2O) associated with only a modest rise in blood Na+ (11 mmol/l) with administration of 1.3 litres of 5% saline (1 113 mmol Na+ total). Unfortunately urine output data were unavailable for case 2, but from a mathematical standpoint (under the assumption of no water or sodium output) the calculated rise in blood Na+ from administration of 1.3 litres 5% saline would have resulted in a substantial (and lethal) blood Na+ of 208 mmol/l in this 58 kg woman.
Of curious physiological interest were the discrepancies between water and sodium balance calculations in association with actual blood Na+ changes, particularly with regard to case 1, for whom we were able to obtain detailed input and output data from hospital records. These revealed a progressively positive fluid balance associated with the recovery of blood Na+ (Fig. 1b). This was curious because we would have expected that a positive fluid balance, commonly associated with dilutional hyponatraemia, would have normalised during recovery with an associated diuresis-induced negative fluid balance, similar to that seen on day 5 (Fig. 1b). This overall positive fluid balance during recovery was unexpected. This suggests that these discrepancies in actual versus measured changes in blood sodium concentration highlight the complexity of fluid and sodium homeostasis, possibly related to osmotic activation and inactivation of sodium stores under non-steady-state conditions.6 Also unknown were the non-osmotic stimuli to arginine vasopressin secretion, which facilitated fluid retention in these two athletes. Potential non-osmotic stimuli resulting in arginine vasopressin secretion include event stress, heat, plasma volume contraction, ciprofloxacin use (case 1) or many unknown exercise-related stimuli.
In conclusion, female athletes moving relatively slowly and with a history of high fluid intake who present to medical personnel with vomiting and mental status changes should be evaluated promptly for EAH. If symptomatic hyponatraemia is confirmed via a blood test, the recommended treatment is administration of an intravenous dose of hypertonic saline (100 ml 3% or 50 ml 5% saline) to reverse cerebral oedema. Administering Ringer's lactate to symptomatic athletes without a blood test to rule out or confirm a diagnosis of hyponatraemia should be discouraged, as it can result in a fatal outcome.12
Disclosure. The authors have no conflict or competing interests to disclose.
References
1. Noakes TD, Goodwin N, Rayner BL, Branken T, Taylor RK. Water intoxication: a possible complication during endurance exercise. Med Sci Sports Exerc 1985;17(3):370-375. [ Links ]
2. Hew-Butler T, Sharwood K, Boulter J, et al. Dysnatremia predicts a delayed recovery in collapsed ultramarathon runners. Clin J Sport Med 2007;17:289-296. [ Links ]
3. Sharwood K, Collins M, Goedecke J, Wilson G, Noakes T. Weight changes, sodium levels, and performance in the South African Ironman Triathlon. Clin J Sport Med 2002;12(6):391-399. [ Links ]
4. Sharwood K, Collins M, Goedecke J, Wilson G, Noakes T. Weight changes, medical complications and performance during an Ironman triathlon. Br J Sports Med 2004;38(6):718-724. [ Links ]
5. Hew-Butler TD, Ayus JC, Kipps C, et al. Statement of the Second International Exercise-Associated Hyponatremia Consensus Development Conference, New Zealand, 2007. Clin J Sport Med 2008;18(2):111-121. [ Links ]
6. Noakes TD, Sharwood K, Speedy D, et al. Three independent biological mechanisms cause exercise-associated hyponatremia: evidence from 2,135 weighed competitive athletic performances. Proc Natl Acad Sci USA 2005;102(51):18550-18555. [ Links ]
7. Ayus JC, Varon J, Arieff AI. Hyponatremia, cerebral edema, and noncardiogenic pulmonary edema in marathon runners. Ann Intern Med 2000;132(9):711-714. [ Links ]
8. Siegel AJ, Verbalis JG, Clement S, et al. Hyponatremia in marathon runners due to inappropriate arginine vasopressin secretion. Am J Med 2007;120(5):461.e11-467.e17. [ Links ]
9. Hew-Butler T, Noakes TD, Siegel AJ. Practical management of exercise-associated hyponatremic encephalopathy: The sodium paradox of non-osmotic vasopressin secretion. Clin J Sport Med 2008;18(4):350-354. [ Links ]
10. Davis DP, Videen JS, Marino A, et al. Exercise-associated hyponatremia in marathon runners: a two-year experience. J Emerg Med 2001;21(1):47-57. [ Links ]
11. Schwartz WB, Bennett W, Curelop S, Bartter FC. A syndrome of renal sodium loss and hyponatremia probably resulting from inappropriate secretion of antidiuretic hormone. 1957. J Am Soc Nephrol 2001;12(12):2860-2870. [http://dx.doi.org/10.1016/0002-9343(57)90224-3] [ Links ]
12. Thompson JA, Wolff AJ. Hyponatremic encephalopathy in a marathon runner. Chest 2003;124(4):313S. [ Links ]
Accepted 31 July 2012.
Corresponding author: T Hew-Butler (hew@oakland.edu)














