Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.102 n.11 Pretoria Jan. 2012
RESEARCH
Safety of nevirapine in HIV-infected pregnant women initiating antiretroviral therapy at higher CD4 counts: a systematic review and meta-analysis
Ebrahim BeraI; Rafiq MiaII
IMB BCh, FCOG (SA). Department of Obstetrics and Gynaecology, University of the Witwatersrand and Rahima Moosa Mother-and-Child Hospital, Johannesburg
IIMB BCh, FCOG (SA). Department of Obstetrics and Gynaecology, University of the Witwatersrand and Rahima Moosa Mother-and-Child Hospital, Johannesburg
ABSTRACT
BACKGROUND: The package insert for nevirapine (NVP) cautions against use in HIV-infected women (including pregnant women) with CD4 counts >250 cells/ΐ. However, recent studies showed that the CD4 count of pregnant women receiving antiretroviral therapy (ART) was not predictive of NVP toxicity.
OBJECTIVES: To determine whether ART-naive pregnant women initiating NVP-based ART at higher CD4 counts experience greater toxicity compared with pregnant women at lower CD4 counts.
METHODS: We reviewed studies comparing serious adverse NVP-related events among ART-naive pregnant women who commenced therapy at higher v. lower CD4 counts. Relevant studies were extracted from PubMed, SCOPUS and EMBASE, major journals and conference proceedings prior to December 2011. Authors were contacted for additional data. Data were independently extracted and entered into Review Manager.
RESULTS: Fourteen studies (2 663 participants) were included for analysis. The odds ratio (OR) for overall NVP toxicity among pregnant women with CD4 <250 cells/! was 0.61 (95% confidence interval (CI) 0.43 - 0.85). When analysis was restricted to prospective studies only (7 studies, 1 318 participants), the results were consistent for overall NVP toxicity (OR 0.43; 95% CI 0.25 -0.73) and severe hepatotoxicity (OR 0.45; 95% CI 0.22 - 0.90), but not for severe cutaneous reaction (OR 0.53; 95% CI 0.26 - 1.10).
CONCLUSION: Initiating NVP-based ART during pregnancy at CD4 >250 cells/! increases toxicity risk and should be avoided, necessitating urgent revision of current guidelines supporting this practice.
In January 2005, the United States (US) Food and Drug Administration (FDA) issued a public health advisory recommending against initiating nevirapine (NVP) in HIV-infected women (including pregnant women) with CD4 counts >250 cells/!.1 The NVP package insert was revised accordingly to warn about risks, with further revision in November 2011 to comply with FDA recommendations on product labelling safety.2
The initial warning followed a meta-analysis of hepatotoxicity in over 600 women, stratified by CD4 count (risk ratio 9.8 with a CD4 count >250 cells/^.3 However, results from several subsequent studies with larger datasets demonstrated no association between CD4 count and NVP toxicity.4-6 Current World Health Organization (WHO) guidelines recommend NVP as part of first-line antiretroviral therapy (ART) for pregnant women with CD4 <350 cells^l,7 based on their own analysis of 836 pregnant women, which showed no increased hepatotoxicity risk at CD4 >250 cells^l (relative risk 1.04; 95% confidence interval (CI) 0.22 - 4.93).8
The 2010 South African Prevention of Mother-to-Child Transmission (PMTCT) guidelines recommend lifelong NVP-based ART for HIV-infected pregnant women with WHO clinical stage 3 or 4 disease, regardless of CD4 count.9 In contrast, the 2011 perinatal guidelines from the US Department of Health and Human Services recommend a protease inhibitor as part of the ART regimen for pregnant women with a CD4 count >250 cells/^ while cautioning against starting NVP above this count.10 The British HIV Association 2012 draft guidelines recommend either efavirenz (EFV) or NVP (with a CD4 count <250 cells/l) or a boosted protease inhibitor as the third drug for pregnant women requiring ART for their own health.11 The recommendation of EFV is a departure from previous guidelines discouraging its use in pregnancy. Furthermore, women who conceived on EFV-based ART need not switch to another drug in the first trimester, following analysis of recent data showing no increased risk of birth defects after first-trimester EFV exposure.11
Reports of NVP-related maternal deaths have surfaced in South Africa, generating renewed concerns about the drug's safety, notably among ART-naive pregnant women. The Eastern Cape Province recently amended its PMTCT guidelines following an analysis of 45 HIV-related maternal deaths, 6 due to liver failure and Stevens-Johnson Syndrome (SJS). The use of NVP in pregnancy since then has been limited to a single dose at delivery (M Shweni, personal communication).
To address the uncertainty about the safety of initiating NVP-based ART in pregnancy, we aimed to determine whether ART-naive pregnant women initiating NVP at higher CD4 counts experience greater toxicity.
Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed.12 All studies except case reports were evaluated for inclusion without consideration of their results. ART-naive pregnant women initiating NVP-based ART during the index pregnancy for maternal health or infant prophylaxis were included. For studies that included both ART-naive and -experienced pregnant women, only the data of ART-naive participants were extracted. ART-experienced pregnant women were excluded, including those naive to NVP. Combination ART studies which included NVP use for 7 days or longer were included only if liver transaminases at baseline were <1.25 times the upper limit of normal (ULN). For inclusion, women had to be followed up until delivery.
The primary outcome measure was overall NVP toxicity (severe hepatotoxicity and severe cutaneous reaction). National Institutes of Health Division of AIDS (NIH-DAIDS) guidelines13 were followed for grading severity. Severe hepatotoxicity was defined as: grade 3 or 4 elevation of liver transaminases (>5 and >10 times ULN, respectively); rash-associated hepatotoxicity; or clinical hepatitis accompanied by elevated liver transaminases. Severe cutaneous reaction was defined as: diffuse maculopapular rash with vesicles, limited number of bullae or superficial ulceration of mucous membranes limited to one site (grade 3); or the presence of generalised bullous lesions, SJS, or toxic epidermal necrolysis (grade 4). Cases of concurrent rash and hepatotoxicity were assigned to 'severe hepatotoxicity'.
We performed electronic searches of PubMed, SCOPUS and EMBASE from inception to 25 November, 5 December and 31 December 2011, respectively. Search terms used included 'nevirapine' and 'pregnancy or pregnant' and 'toxicity or safety or adverse effects or side-effects'. An extensive hand-search of major infectious diseases journals published prior to December 2011 was performed. Article reference lists and AIDS conference proceedings were also hand-searched.
Abstracts were reviewed and potentially relevant full-text articles were retrieved based on consensus and discussion. All articles from the WHO meta-analysis which included pregnant women were also retrieved. Data were extracted using a previously prepared data extraction form. For duplicate publications, the more informative study was used. Authors from 13 articles were contacted for additional data or clarity regarding datasets; 9 responded.
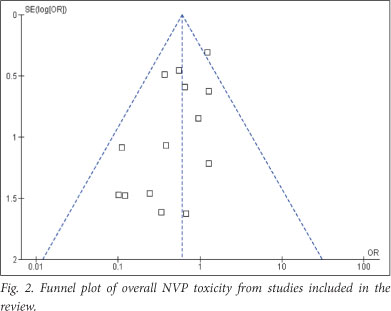
Review Manager 5.1 (RevMan 2011) was used for statistical analyses. The Mantel-Haenszel method was used for comparisons of dichotomous data. Results were presented as odds ratios (ORs) with 95% CIs. Heterogeneity was quantified using the I2 statistic (the proportion of variation due to study heterogeneity).14 In the absence of substantial heterogeneity (I2<30%) results were pooled using a fixed-effects model. Funnel plots were visually examined to explore possible publication bias.
Results
Data retrieval, exclusion and inclusion are summarised in Fig. 1. We excluded some of the largest studies on PMTCT (including several thousand women from around the globe) primarily because NVP use was restricted to women with CD4 counts <250 cells/l.15,16 In many of these studies, toxicity data were not routinely collected (C Townsend, personal communication). Routine collection of toxicity data was also absent in a number of African PMTCT studies with fairly large cohorts.
Among reasons for the exclusion of certain antenatal studies (Table 1),6,15-26 the most common reason was the absence of data dichotomised by CD4 count. Two studies with CD4 cut-offs of 500and 200 cells/ìl, respectively,22,25 were also excluded as CD4 count relative to NVP toxicity was not available.
At data entry, we excluded 1 of 5 serious adverse events (SAEs) reported by Hitti et al.,27 as the subject (CD4 count 259 cells/ìl) reportedly developed clinical hepatitis, but alanine transaminase (ALT) was 41 U/l at diagnosis. Three further participants were excluded from the data of Natarajan et al.;2 CD4 counts were unknown in 2, and the third (CD4 count 332 cells/l) developed elevated liver transaminases >3 times the ULN. From Peters et al., we only extracted the data for the women who initiated NVP-based ART.29
Fourteen studies were reviewed, including a total of 2 663 participants (Table 2).4,5,27-38 One study was funded by the NVP manufacturer Boehringer Ingelheim.30 The studies, mostly undertaken between 2001 and 2006, were predominantly observational with participant numbers ranging from 17 to 703. Average female participant age was 28 years, and ART was initiated at an average of 27 weeks' gestation. The mean baseline CD4 count varied (113 - 545 cells/!). Participants with hepatitis B or C infection were excluded from 2 studies,4,27 whereas 7 studies reported the prevalence of hepatitis co-infection.28-30,34,36-38 NVP was initially commenced at 200 mg daily for 14 days in all women. The CD4 cut-off was 250 cells/ìl for toxicity analyses in all studies, except for one (CD4 cut-off of 200 cells/ ìl).35 Mean time to toxicity ranged from 27 to 74 days. The overall frequency of NVP toxicity was 8.3%, driven mostly by hepatotoxicity.
Additional unpublished data were obtained from Coffie et al.,31 Lyons et al.36 and Marazzi et al.5 There was a significant reduction in overall NVP toxicity among women with CD4 <250 cells/ìl (OR 0.61; 95% CI 0.43 - 0.85; I2 8%). One study35 was excluded from analysis as it used a CD4 cut-off of 200 cells/ìl; the result following exclusion was unaltered (OR 0.62; 95% CI 0.44 - 0.87; I2 12%).
Severe hepatotoxicity was not significantly reduced with NVP use at CD4 <250 cells/! (OR 0.75; 95% CI 0.48 - 1.15; I2 0%). Risk for severe cutaneous reaction was analysed from 13 studies (2 572 participants). There was a statistically significant reduction in severe skin rash among pregnant women with CD4 <250 cells^l (OR 0.57; 95% CI 0.35 - 0.94; I2 0%).
All studies except Aaron et al. included mortality data.30 The cumulative mortality rate was 0.5% (14 of 2 584 women), with at least 4 maternal deaths directly attributable to NVP use.5,27,36 We could not perform an NVP-related mortality analysis stratified by CD4 count due to data limitations.
For the 7 prospective studies reviewed, involving 1 318 participants, the OR for overall NVP toxicity among women with CD4 <250 cells/ was 0.43 (95% CI 0.25 - 0.73; I2 0%), and 0.45 for severe hepatotoxicity (95% CI 0.22 - 0.90; I2 0%). NVP use at CD4 <250 cells^l did not significantly reduce the odds of severe cutaneous reaction (OR 0.53; 95% CI 0.26 - 1.10; I2 0%).
The Funnel plot (Fig. 2) showed no gross asymmetry to suggest overt publication bias.
Discussion
Commencing NVP in ART-naive pregnant women with CD4 counts >250 cells^l significantly increased the odds of toxicity. Our results are consistent with the findings of a previous meta-analysis that informed the current FDA safety alert on NVP use.3 An important finding of our review was that NVP-related SAEs seem to occur fairly soon after ART initiation (within 10 weeks). Relative risks of toxicity may be lower than previously estimated. For every 200 women who commenced NVP-based ART at CD4 >250 cells^l, 7 additional women experienced severe side-effects. Strengths of our review include the size of the dataset (the largest to date), robust methods, and that most included studies were published after the FDA advisory in 2005.
Our results vary with those of several recently published studies on the risks of NVP-related toxicity in pregnancy, for which there may be numerous reasons. Firstly, in many studies the toxicity data of ART-naive and -experienced pregnant women were combined.6,19,23,24 The appropriateness of combining such data deserves scrutiny. Mocroft et al. demonstrated that the risk of NVP discontinuation due to toxicity was significantly lower in ART-experienced women compared with ART-naive women at CD4 counts >250 cells/^.39 In another study, stable virologically suppressed women who switched to NVP-based ART did not experience higher rates of hepatotoxicity.40 Complete plasma viral load suppression appears to be protective of NVP hepatotoxicity. These findings suggest that combining data of ART-naive and -experienced women may underestimate the true risks of NVP toxicity. For example, in the analysis by Ouyang et al., only 91 of 1 229 pregnant women were ART-naive and initiated NVP-based ART, suggesting that the majority of women were already taking ART at conception.6 In their study, the rate of severe hepatotoxicity was 0.5%. A separate analysis comparing ART-naive and -experienced women was not performed. Also, the median time from ART initiation to toxicity was 163 days, considerably longer than the time reported by studies in our review.
Secondly, in some of the recently published studies the data on hepatotoxicity - stratified by CD4 count - were performed as a single analysis for women on NVP and those on nelfinavir (NFV).24,29,30 Nelfinavir use is rarely associated with hepatotoxicity.11 Combining hepatotoxicity data for NFV and NVP may potentially dilute the association between NVP and hepatotoxicity at higher CD4 counts. As an example, in the study by Peters et al.,29 only 1 of 208 women with CD4 >250 cells^l initiated NVP during the second enrolment period. The remaining 207 women started NFV. An analysis of adverse events for the second period adjusted for CD4 count may not have been appropriate.
Thirdly, the endpoints in our systematic review were limited to severe or life-threatening adverse events. Several papers included comparisons of all NIH-DAIDS grades of toxicity.4,5,28,30,33,35-38 In the WHO meta-analysis, the authors did not evaluate cutaneous reactions in pregnancy, and NVP hepatotoxicity was analysed for all grades of severity.8 They correctly emphasised the need for cautious interpretation of their results based only on grades 3 and 4 toxicities, given limited cohort numbers and open-labelled designs of included studies. However, 3 important studies considered in their meta-analysis merit discussion. In the study by Jamisse et al.,33 the overall rates of hepatotoxicity among women with CD4 counts lower and higher than 250 cells^l were similar (6% and 9%, respectively), but severe hepatotoxicity occurred in 0% and 6% (p=0.02) in the 2 groups, respectively. In the study by Kondo et al.,4 severe hepatotoxicity occurred exclusively in women with CD4 >250 cells^l. The study by Marazzi et al. showed no differences in grade 3 and 4 hepatotoxicity rates by CD4 count (250 cells^l), but their unpublished results for severe cutaneous reaction among women with CD4 counts less or greater than 250 cells/, were 2% and 4%, respectively.5 While we certainly share the WHO authors' concerns around the interpretation of results based on limited numbers, their meta-analysis did not provide reassurance on treatment-limiting toxicities above this CD4 threshold.
It remains unclear why women with better immunological reserves are more vulnerable to the hazards of NVP. The mechanism is believed to be an immune-mediated hypersensitivity reaction. Some investigators have found a higher frequency of allele HLA-DRB1*01 in patients who developed a cutaneous reaction to NVP or EFV.41 Others demonstrated increased expression of HLA-Cw8 among those who developed NVP hypersensitivity.42 In a case-control study performed in South Africa, investigators found that the MDR1 position 3435 T allele was associated with a decreased risk of NVP-related hepatotoxicity.43 A recent systematic review showed that pregnancy itself may be an additional risk factor for NVP hepatotoxicity.44 Predisposition to NVP toxicity may be multifactorial and, at present, there is no simple reliable way to predict such outcomes among women initiating NVP-based ART.
Study limitations
A number of studies did not report the use of drugs with overlapping toxicity profiles (e.g. rifampicin, isoniazid and cotrimoxazole). The reporting of hepatitis B and C and alcohol and illicit drug use varied considerably, and few studies reported the prevalence of pre-eclampsia and HELLP syndrome in pregnancy. The latter is known to mimic drug toxicity and lead to NVP withdrawal.
Finally, only one study was a randomised trial, and it was prematurely terminated.27 All others were observational, and therefore prone to several forms of bias. Confounding variables which cannot be measured are usually addressed through random allocation of participants to an intervention arm. A randomised study comparing NVP with EFV during pregnancy seems to be the way forward, but is unlikely to receive ethics approval until the 'teratogenicity' concerns surrounding EFV use in pregnancy are resolved.
Conclusion
We observed an absence of new data to support the safe initiation of NVP among ART-naive pregnant women with a CD4 count >250 cells^l. Rather, NVP initiation in these women significantly increased the frequency of SAEs. We strongly recommend urgent revision of guidelines supporting this practice. Pharmacovigilance programmes on ART use in pregnancy should be strengthened nationally.
Acknowledgements. Contacted study authors are acknowledged for their prompt response and provision of data. Vivian Black, Edgardo Bottaro, Didier Ekouevi, Risa Hoffman, Esau Joao, Giuseppe Liotta, Fiona Lyons, David Ouyang and Claire Townsend are acknowledged.
References
1. United States Food and Drug Administration (FDA). FDA Advisory on nevirapine. AIDS Treat News 2005;2205(409):7. [ Links ]
2. FDA. Center for Drug Evaluation and Research. Rockville, USA: FDA, 2011. http://www.accessdata.fda.gov/drugsatfda_docs/label/2011/020636s039_020933s030lbl.pdf (accessed 13 December 2011). [ Links ]
3. Baylor MS, Johann-Liang R. Hepatotoxicity associated with nevirapine use. J Acquir Immune Defic Syndr 2004;35(5):538-539. [ Links ]
4. Kondo W, Carraro EA, Prandel E, et al. Nevirapine-induced side-effects in pregnant women -experience of a Brazilian University hospital. Braz J Infect Dis 2007;11(6):544-548. [ Links ]
5. Marazzi MC, Germano P, Liotta G, et al. Safety of nevirapine-containing antiretroviral triple therapy regimens to prevent vertical transmission in an African cohort of HIV-1-infected pregnant women. HIV Med 2006;7:338-344. [http://dx.doi.org/10.1111/j.1468-1293.2006.00386.x] [ Links ]
6. Ouyang DW, Brogly SB, Lu M, et al. Lack of increased hepatotoxicity in HIV-infected pregnant women receiving nevirapine compared with other antiretrovirals. AIDS 2010;24(1):109-114. [http://dx.doi.org/10.1097/QAD.0b013e3283323941] [ Links ]
7. WHO. Antiretroviral drugs for treating pregnant women and preventing HIV infections in infants. Recommendations for a public health approach - 2010 version. Geneva, Switzerland: WHO, 2010. [ Links ]
8. WHO. Summary of available safety data for nevirapine, stavudine, zidovudine and tenofovir. Geneva, Switzerland: WHO, 2009. http://www.who.int/hiv/topics/treatment/neveriapine_stavudine_zidovudine_tenofovir.pdf (accessed 21 November 2011). [ Links ]
9. Department of Health. Clinical Guidelines: PMTCT 2010. Pretoria: Department of Health, 2010. [ Links ]
10. Panel on treatment of HIV-infected pregnant women and prevention of perinatal transmission. Recommendations for use of antiretroviral drugs in pregnant HIV-1-infected women for maternal health and interventions to reduce perinatal HIV transmission in the United States. September 14, 2011. Available at: http://aidsinfo.nih.gov/contentfiles/PerinatalGL.pdf. Accessed November 2011. [ Links ]
11. de Ruiter A, Taylor GP, Palfreeman A, et al. British HIV Association Guidelines for the management of HIV infection in pregnant women 2012. Consultation draft. http://www.bhiva.org/documents/Guidelines/Pregnancy/Pregnancy_Guidelines_for_Consultation1201 25.pdf (accessed 24 February 2012). [ Links ]
12. Liberati A, Altmann DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700. [http://dx.doi.org/10.1136/bmj.b2700]
13. National Institutes of Health. Division of AIDS table for grading the severity of adult and pediatric adverse events. Bethesda, USA: NIH, 2004. http://www.niaid.nih.gov/labsandresources/resources/daidsclinrsrch/documents/daidsaegradingtable. pdf (accessed 21 November 2011). [ Links ]
14. Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539-1558. [http://dx.doi.org/10.1002/sim.1186] [ Links ]
15. European Collaborative Study. The mother-to-child HIV transmission epidemic in Europe: evolving in the East and established in the West. AIDS 2006;20(10):1419-1427. [http://dx.doi.org/10.1097/01.aids.0000233576.33973.b3] [ Links ]
16. Townsend CL, Cortina-Borja M, Peckham CS, de Ruiter A, Lyall H, Tookey PA. Low rates of mother-to-child transmission of HIV following effective pregnancy interventions in the United Kingdom and Ireland, 2000 - 2006. AIDS 2008;22(8):973-981. [http://dx.doi.org/10.1097/QAD.0b013e3282f9b67a] [ Links ]
17. Bersoff-Matcha SJ, Rourke D, Blank J. Evaluation of the safety of nevirapine during pregnancy. J Acquir Immune Defic Syndr 2010;54(5):560-562. [http://dx.doi.org/10.1097/QAI.0b013e3181d36024] [ Links ]
18. Black V, Hoffman RM, Sugar CA, et al. Safety and efficacy of initiating highly active antiretroviral therapy in an integrated antenatal and HIV clinic in Johannesburg, South Africa. J Acquir Immune Defic Syndr 2008;49(3):276-281. [http://dx.doi.org/10.1097QAI.0b013e318189a769] [ Links ]
19. Bottaro EG, Huberman MJ, Iannella M del Carmen, et al. Nevirapine-associated toxicity in clinical practice in Buenos Aires, Argentina. J Int Assoc Physicians AIDS Care 2010;9(5):306-312. [http://dx.doi.org/10.1177/1545109710376250] [ Links ]
20. Edwards SG, Larbalestier N, Hay P, et al. Experience of nevirapine use in a London cohort of HIV-infected pregnant women. HIV Med 2001;2:89-91. [http://dx.doi.org/10.1046/j.1468-1293.2001.00059.x] [ Links ]
21. Joao EC, Calvet GA, Menezes JA, et al. Nevirapine toxicity in a cohort of HIV-1-infected pregnant women. Am J Obstet Gynecol 2006;194:199-202. [http://dx.doi.org/10.1016/j.ajog.2005.05.015] [ Links ]
22. Kramer F, Stek A, Du WB, et al. Nevirapine tolerability in HIV-infected women in pregnancy. 11th Conference on Retroviruses and Opportunistic Infections, 8 - 11 February 2004, San Francisco (CA). [ Links ]
23. Manfredi R, Calza L. Safety issues about nevirapine administration in HIV-infected pregnant women. J Acquir Immune Defic Syndr 2007;45(3):365-368. [http://dx.doi.org/10.1097/QAI.0b013e318050d879; [ Links ]
24. Ouyang DW, Shapiro DE, Lu M, et al. Increased risk of hepatotoxicity in HIV-infected pregnant women receiving antiretroviral therapy independent of nevirapine exposure. AIDS 2009;23(18):2425-2430. [http://dx.doi.org/10.1097/QAD.0b013e32832e34b1] [ Links ]
25. Timmermans S, Tempelman C, Godfried MH, et al. Nelfinavir and nevirapine side effects during pregnancy. AIDS 2005;19(8):795-799. [ Links ]
26. Weinberg A, Forster-Harwood J, Davies J, et al. Safety and tolerability of antiretrovirals during pregnancy. Infect Dis Obstet Gynecol 2011;e867674. [http://dx.doi.org/10.1155/2011/867674] [ Links ]
27. Hitti J, Frenkel LM, Stek AM, et al. Maternal toxicity with continuous nevirapine in pregnancy. Results from PACTG 1022. J Acquir Immune Defic Syndr 2004;36(3):772-776. [ Links ]
28. Natarajan U, Pym A, McDonald C, et al. Safety of nevirapine in pregnancy. HIV Med 2007;8:64-69. [http://dx.doi.org/10.1111/j.1468-1293.2007.00433.x] [ Links ]
29. Peters PJ, Polle N, Zeh C, et al. Nevirapine-associated hepatotoxicity and rash among HIV-infected pregnant women in Kenya. J Int Assoc Physicians AIDS Care 2011; [http://dx.doi.org/10.1177/1545109711423445] [ Links ]
30. Aaron E, Kempf M, Criniti S, et al. Adverse events in a cohort of HIV infected pregnant and non-pregnant women treated with nevirapine versus non-nevirapine antiretroviral medication. PLoS ONE 2010;5(9):e12617. [http://dx.doi.org/10.1371/journal.pone.0012617] [ Links ]
31. Coffie PA, Tonwe-Gold B, Tanon AK, et al. Incidence and risk factors of severe adverse events with nevirapine-based antiretroviral therapy in HIV-infected women. MTCT-Plus program, Abidjan, Cote d'Ivoire. BMC Infect Dis 2010;10:188. [http://dx.doi.org/10.1186/1471-2334-10-188] [ Links ]
32. Gonzales-Garcia A, Fernandez MI, Cotter A. Nevirapine toxicity in the obstetrical population when used in combination of other antiretrovirals. The XV International AIDS Conference, 11 - 16 July 2004, Bangkok, Thailand. [ Links ]
33. Jamisse L, Balkus J, Hitti J, et al. Antiretroviral-associated toxicity among HIV-1-seropositive pregnant women in Mozambique receiving nevirapine-based regimens. J Acquir Immune Defic Syndr 2007;44(4):371-376. [http://dx.doi.org/10.1097/QAI.0b013e318032bbee] [ Links ]
34. Joy S, Poi M, Hughes L, et al. Third trimester maternal toxicity with nevirapine use in pregnancy. Obstet Gynecol 2005;106(5):1032-1038. [http://dx.doi.org/10.1097/01.AOG.0000180182.00072.e3] [ Links ]
35. Kilewo C, Karlsson K, Ngarina M, et al. Prevention of mother-to-child transmission of HIV-1 through breastfeeding by treating mothers with triple antiretroviral therapy in Dar es Salaam, Tanzania: the Mitra Plus Study. J Acquir Immune Defic Syndr 2009;52(3):406-416. [http://dx.doi.org/10.1097/QAI.0b013e3181b323ff] [ Links ]
36. Lyons F, Hopkins S, Kelleher B, et al. Maternal hepatotoxicity with nevirapine as part of combination antiretroviral therapy in pregnancy. HIV Med 2006;7:255-260. [http://dx.doi.org/10.1111/j.1468-1293.2006.00369.x] [ Links ]
37. Phanuphak N, Apornpong T, Teeratakulpisarn S, et al. Nevirapine-associated toxicity in HIV-infected Thai men and women, including pregnant women. HIV Med 2007;8:357-366. [http://dx.doi.org/10.1111/j.1468-1293.2007.00477.x] [ Links ]
38. van Schalkwyk JE, Alimenti A, Khoo D, et al. Serious toxicity associated with continuous nevirapine- based HAART in pregnancy. BJOG 2008;115:1297-1302. [http://dx.doi.org/10.1111/j.1471-0528.2008.01820.x] [ Links ]
39. Mocroft A, Staszewski S, Weber R, et al. Risk of discontinuation of nevirapine due to toxicities in antiretroviral-naive and -experienced HIV-infected patients with high and low CD4 T-cell counts. Antivir Ther 2007;12:325-333. [ Links ]
40. De Lazzari E, Leon A, Arnaiz JA, et al. Hepatotoxicity of nevirapine in virologically suppressed patients according to gender and CD4 cell counts. HIV Med 2008;9:221-226. [http://dx.doi.org/10.1111/j.1468-1293.2008.00552.x] [ Links ]
41. Vitezica ZG, Milpied B, Lonjou C, et al. HLA-DRB1*01 associated with cutaneous hypersensitivity induced by nevirapine and efavirenz. AIDS 2008;22(4):540-541. [http://dx.doi.org/10.1097/QAD.0b013e3282f37812] [ Links ]
42. Gatanaga H, Yazaki H, Tanuma J, et al. HLA-Cw8 primarily associated with hypersensitivity to nevirapine. AIDS 2007;21(2):264-265. [http://dx.doi.org/10.1097/QAD.0b013e32801199d9] [ Links ]
43. Haas DW, Bartlett JA, Andersen JW, et al. Pharmacogenetics of nevirapine-associated hepatotoxicity: an adult AIDS Clinical Trials Group Collaboration. Clin Infect Dis 2006;43:783-786. [http://dx.doi.org/10.1058-4838/2006/4306-0021] [ Links ]
44. McKoy JM, Bennett CL, Scheetz MH, et al. Hepatotoxicity associated with long-versus short-course HIV-prophylactic nevirapine use: a systematic review and meta-analysis from the Research on Adverse Drug Events And Reports (RADAR) project. Drug Saf 2009;32(2):147-158. [http://dx.doi.org/10.2165/00002018-200932020-00007] [ Links ]
Accepted 27 June 2012.
 Corresponding author:
Corresponding author:
E Bera
(drebera@hotmail.com)














