Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.102 n.9 Pretoria Sep. 2012
RESEARCH
Case fatality of patients with stroke over a 12-month period post stroke
W MudziI; A StewartII; E MusengeIII
IPhD. Department of Physiotherapy, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg
IIPhD. Department of Physiotherapy, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg
IIIMSc, MMed. Biostatistics and Epidemiology Division, School of Public Health, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg
ABSTRACT
INTRODUCTION: Stroke is among the top 4 causes of death in South Africa and the top 10 leading causes of disability worldwide. There is a dearth of literature on stroke incidence, prevalence and outcome in sub-Saharan Africa. We aimed to establish the case fatality of stroke patients over a 12-month period post discharge from hospital.
METHODS: A total of 200 patients with first-time ischaemic stroke were recruited from Chris Hani Baragwanath Academic Hospital and followed up for 12 months. The Barthel Index (BI) and Rivermead Mobility Index (RMI) were used to establish patient functional ability and, by inference, stroke severity. Follow-up assessments were performed at 3, 6 and 12 months post discharge. Data analysis was largely descriptive in nature.
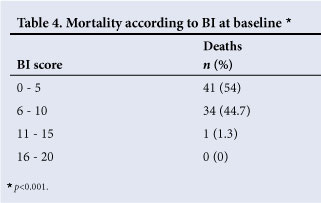
RESULTS: Thirty-eight per cent of patients died within the 12 month follow-up period; 25.5% within 3 months of discharge. The average length of hospital stay was 6 days. Low BI scores at discharge were observed in the majority of patients who died.
CONCLUSION: The 12-month cumulative mortality was high (highest at the 3-month follow-up). The short hospital stay and poor functional ability of the patients post stroke possibly left them vulnerable to bed-rest complications, such as chest infections and pressure sores.
Aside from the devastating effects of HIV/AIDS, neurological disability (stroke included) is one of the most important future healthcare challenges.1 Stroke is among the top 4 causes of death in South Africa (SA) and the top 10 causes of disability worldwide.2,3 Most stroke-related studies in sub-Saharan Africa are hospital-based, many of them retrospective case-note reviews. Consequently, there is a dearth of literature on stroke incidence, prevalence and outcome.4 A study in SA found a high prevalence of hypertension and postulated an emerging vascular disease epidemic.5 A systematic review of stroke mortality, prevalence, incidence and case fatality in sub-Saharan Africa6 noted a stroke prevalence of less than half of that of high-income countries, but an equivalent disabling stroke prevalence. As a consequence of the lack of community-based incidence studies, stroke incidence remains largely unknown.7
Furthermore, mortality post stroke is largely unknown in subSaharan Africa. The only applicable SA study found reported 18% and 23% cumulative mortality at 3 and 6 months post stroke, respectively.8 This work aimed to establish the case fatality of stroke patients over a 12-month period post discharge from Chris Hani Baragwanath Academic Hospital (CHBAH).
Methods
A total of 200 consecutive consenting patients with first-time ischaemic stroke were recruited from CHBAH between 2006 and 2010 and followed up for 12 months. Patients were recruited after admission for suspected or confirmed ischaemic stroke. Diagnosis was confirmed with computed tomography (CT)/magnetic resonance imaging (MRI) and a neurologist performed stroke subtype classification according to the Oxfordshire Community Stroke Project (OCSP) system.9 The study was approved by the Human Research Ethics Committee of the University of the Witwatersrand.
Prior to discharge, a baseline assessment was performed to determine demographic data, stroke cause and subtype, and resultant neurological deficits. The Barthel Index (BI) and Rivermead Mobility Index (RMI) were administered to establish patient functional ability. The EuroQol (EQ)-5D visual analogue scale (VAS) was used to establish perceived health-related quality of life. Caregivers provided information in the event of patient speech problems. Follow-up assessments were performed, mainly at home, at 3, 6 and 12 months post discharge.
Data analysis was largely descriptive in nature and performed using STATA software (version 12). Data were represented as means with standard deviation (SD) or error (SE). The effect of BI on mortality was established using the Log-rank test.
Results
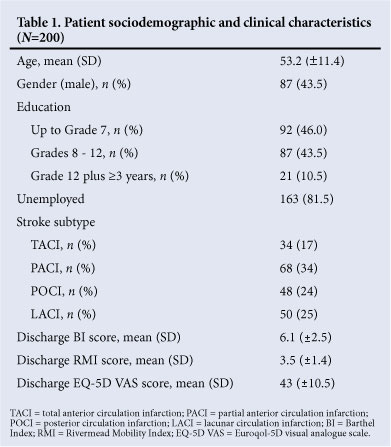
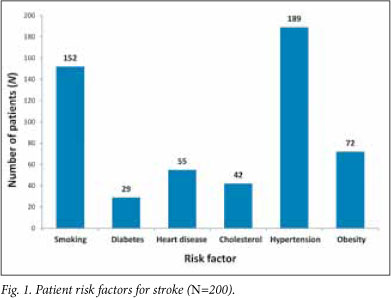
All 200 recruited patients were black. Ten patients were untraceable at their given addresses. Mean length of hospital stay was 6 days (SD ±4 days). Average number of physiotherapy sessions during hospitalisation was 1. More than 90% of patients had access to electricity and running water at home. Patient sociodemographic and baseline characteristics are summarised in Tables 1 and 2. Fig. 1 shows the distribution of risk factors for stroke.
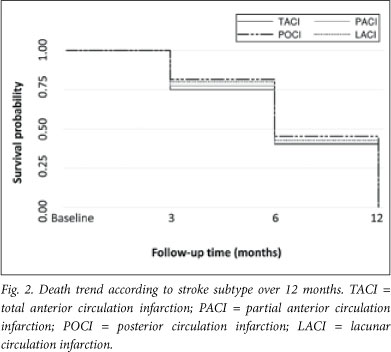
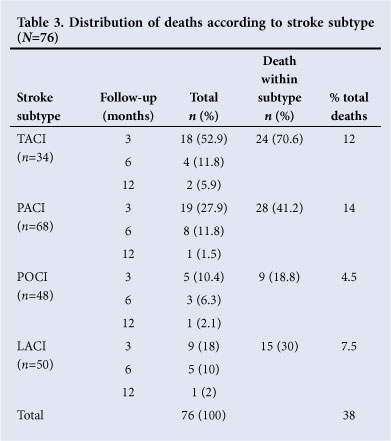
The cumulative mortality was 25.5% at 3 months, 35.5% at 6 months and 38.0% at 12 months post discharge. Cause of death was not established. Case fatality according to stroke subtype is presented in Fig. 2 and Table 3. The highest contribution to the overall mortality rate originated from the partial anterior circulation infarction (PACI) subtype (14%). Within subtypes, the total anterior circulation infarction (TACI) group had the highest mortality rate (70.6%). The relationship between stroke subtype and death was not statistically significant (p>0.05). Table 4 summarises the mortality according to BI range at baseline.
Discussion
Of patients who met the inclusion criteria, 56.5% were female and 43.5% were male, consistent with other studies.8,10 Mean patient age (53.2±11.4 years) was much younger than that of a previous study performed in Cape Town.8 Reported mean stroke patient age is 67.3 years in Belgium10 and >70 years in most high-income countries7. This supports the hypothesis that stroke occurs at much earlier ages in sub-Saharan Africa.11
In agreement with previous studies, hypertension (95%), smoking (76%) and obesity (36%) were the most common risk factors for stroke in SA.5,12 This supports the view that the country is in danger of a 'stroke explosion' as the adoption of Western lifestyles by the population takes its toll.5 All 3 risk factors are modifiable, highlighting the importance of pertinent health education.11
The 3-month (25.5%) and 6-month (35.5%) cumulative mortality rates were higher than in the aforementioned Cape Town study (18% and 23%, respectively).8 However, the case mix differed between the 2 studies; only ischaemic stroke patients were included in the present analysis.
The mortality rate of 38% within 12 months post discharge was consistent with that reported by Wolfe (34 - 41%).13 The latter study, however, encompassed all forms of stroke, while the present study included only those from infarctions. Furthermore, the mortality rate was in agreement with the previously reported 12-month stroke case fatality in Zimbabwe (30%),14 but much lower than that of
The Gambia (62%).15 The high mortality rate substantiates that the majority of the 5.7 million deaths attributed to stroke annually occur in low- and middle-income countries.16 The short hospital stay and few physiotherapy treatment sessions received during hospitalisation could have contributed to the poor patient functional ability and high case fatality.
Of the infarction types, patients with posterior circulation infarction (POCI) demonstrated the lowest mortality rate (19%) and TACI patients the highest (70.6%) (Table 3). TACI patients suffer the most grave physical and neurological deficits,17 are more dependent on caregivers, and more susceptible to diseases such as chest infections (due to reduced mobility); hence the higher death rate. In agreement with this, patients who died had, on average, lower
BI, RMI and EQ-5D VAS scores than those who survived (Table 4). This could have been attributed to the high prevalence of bed-rest complications resulting from immobility during the acute period of stroke.17
Lacunar circulation infarction (LACI) stroke patients had a low mortality rate in this study, in agreement with findings from the Netherlands.18 LACI strokes result in the least severe neurological deficits of the infarction subtypes, with no cortical higher function involvement. Consequently, fewer deaths and better functional outcomes are reported among LACI patients.
The high death rate in this study population could be attributed to the low socioeconomic status of the participants, previously shown to be consistent with a higher stroke mortality.19
Conclusion
The cumulative mortality was high at 12 months, but highest at 3 months post discharge. TACI patients demonstrated the poorest survival rate. The short hospital stay and poor functional ability of the patients post stroke possibly left them vulnerable to bed-rest complications such as chest infections and pressure sores. This could explain the high 3-month case fatality. Mechanisms need to be investigated to ensure a reasonable length of hospital stay and concurrent provision of adequate rehabilitation to improve overall functional ability and quality of life. Notably, these findings are limited to patients with infarction stroke who have a short hospital stay and little inpatient rehabilitation.
References
1. Connor MD, Thorogood M, Casserly B, Dobson C, Warlow CP. Prevalence of stroke survivors in rural South Africa: results from the Southern African Stroke Prevention Initiative (SASPI) Agincourt Field Site. Stroke 2004;35(3):627-632. [http://dx.doi.org/10.1161/01.STR.0000117096.61838.C7] [ Links ]
2. Bradshaw D, Nannan N, Laubscher R, et al. South African National Burden of Disease Study 2000: Estimates of provincial mortality. Burden of Disease Research Unit Report. Pretoria: Medical Research Council, 2002. http://www.mrc.ac.za/bod/profile.pdf (accessed 10 January 2012). [ Links ]
3. Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL (eds). Global Burden of Disease and Risk Factors. Oxford, UK: Oxford University and The World Bank, 2006. [http://dx.doi.org/10.1596/978-0-8213-6262-4] [ Links ]
4. Walker R. Hypertension and stroke sub-Saharan Africa. Trans R Soc Trop Med Hyg 1994;88(6):609- 611. [ Links ]
5. Thorogood M, Connor M, Tollman S, Hundt GL, Fowkes G, Marsh J. A cross-sectional study of vascular risk factors in a rural South African population: data from the Southern African Stroke Prevention Initiative (SASPI). BMC Public Health 2007;7:326. [http://dx.doi.org/10.1186/1471-2458-7-326] [ Links ]
6. Connor MD, Walker R, Modi G, Warlow CP. Burden of stroke in black populations in sub-Saharan Africa. Lancet Neurol 2007;6:269-278. [http://dx.doi.org/10.1016/S1474-4422(07)70002-9] [ Links ]
7. Feigin VL, Lawes CMM, Bennet DA, Anderson CS. Stroke Epidemiology: a review of population based studies of incidence, prevalence and case fatality in the late 20th century. Lancet 2003;2:43-53. [http:// dx.doi.org/10.1016/S1474-4422(03)00266-7] [ Links ]
8. De Villiers L, Badri M, Ferreira M, Bryer A. Stroke outcomes in a socio-economically disadvantaged urban community. S Afr Med J 2011;101(5):345-348. [ Links ]
9. Bamford J, Sanderock P, Dennis M, Burn J, Warlow C Classification and natural history of clinically identifiable subtypes of cerebral infarction. Lancet 1991;337:1521-1526. [ Links ]
10. Correia M, Silva MR, Matos I, Magalha'es R, Lopes JC, Ferro JM, Silva MC. Prospective community-based study of stroke in Northern Portugal: incidence and case fatality in rural and urban populations. Stroke 2004;35:2048-2053. [http://dx.doi.org/10.1161/01.STR.0000195209.26543.8f] [ Links ]
11. Lemogoum D, Degaute JP, Bovet P. Stroke prevention, treatment and rehabilitation in sub-Saharan Africa. Am J Prev Med 2005;29:95-101. [http:/dx/doi.org/10.1016/j.amepre.2005.07.025] [ Links ]
12. Thorogood M, Connor M, Tollman S, Hundt GL, Fowkes G, Marsh J. A cross-sectional study of vascular risk factors in a rural South African population: data from the Southern African Stroke Prevention Initiative (SASPI). BMC Public Health 2007;7:326. [http://dx.doi.org/10.1186/1471-2458-7-326] [ Links ]
13. Wolfe CDA. The effectiveness of public health and individual measures in reducing the incidence of stroke. In: Wolfe CDA, Rudd A, Beech R (eds). Stroke Services and Research. London: Stroke Association, 1996;40-87. [ Links ]
14. Matenga J. Stroke incidence rates among black residents of Harare - a prospective community-based study. S Afr Med J 1997;87:1389-1391. [ Links ]
15. Garbusinski JM, van der Sande MA, Bartholome EJ, et al. Stroke presentation and outcome in developing countries. A prospective study in The Gambia. Stroke 2005;36:1388-1393. [http://dx.doi.org/10.1161/01.str.0000170717.91591.7d] [ Links ]
16. Strong K, Mathers C, Bonita R. Preventing stroke: saving lives around the world. Lancet Neurology 2007;6:182-187. [http://dx.doi.org/10.1016/s1474-4422(07)70031-5] [ Links ]
17. Lawrence ES, Coshall C, Dundas R, et al. Estimates of the prevalence of acute stroke impairments and disability in a multiethnic population. Stroke 2001;32:1279-1284. s [http://dx.doi.org/10.1161/01.str.32.6.1279] [ Links ]
18. De Jong G, van Raak L, Kessels F, Lodder J. Stroke subtype and mortality: a follow-up study in 998 patients with a first cerebral infarct. Journal of Clinical Epidemiology 2003;56:262-268. [http:dx.doi.org/10.1016/s0895-4356(02)00572-3] [ Links ]
19. Hart CL, Hole DJ, Smith GD. Influence of socioeconomic circumstances in early and later life on stroke risk among men in a Scottish cohort study. Stroke 2000;31:2093-2097. [http://dx.doi.org/10.1161/01.str.31.9.2093] [ Links ]
Corresponding author: W Mudzi (witness.mudzi@wits.ac.za).














