Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.102 no.8 Pretoria ago. 2012
RESEARCH
Osteosarcoma presentation stages at a tumour unit in South Africa
N FerreiraI; L C MaraisII
IBSc, MB ChB, HDip Orth (SA), FC Orth (SA), MMed (Orth). Tumour, Sepsis and Reconstruction Unit, Department of Orthopaedic Surgery, Greys Hospital, University of KwaZulu-Natal, Pietermaritzburg
IIMB ChB, FCS (Orth) (SA), MMed (Orth), CIME. Tumour, Sepsis and Reconstruction Unit, Department of Orthopaedic Surgery, Greys Hospital, University of KwaZulu-Natal, Pietermaritzburg
ABSTRACT
BACKGROUND: Osteosarcoma is the most common malignant bone tumour found in children and adolescents. Changed treatment protocols have resulted in improved survival and the opportunity for limb salvage surgery. Despite these advances, the outcome is mainly determined by the stage of disease at presentation, making early referral to a tumour unit essential.
METHODS: Between July 2009 and October 2011, 25 consecutive patients were diagnosed with biopsy-confirmed osteosarcoma. Their records were reviewed and information extracted regarding clinical presentation, histological subtype and stage of disease.
RESULTS: Twenty-four patients met the inclusion and exclusion criteria. Conventional osteosarcoma was the most common histological diagnosis encountered; 16 out of 24 (66.7%) patients had metastases at presentation; 6 of the remaining had advanced local disease with very large tumours or pathological fractures that precluded limb salvage surgery.
CONCLUSION: The great majority of patients referred to our tumour unit present with locally advanced or metastatic disease, which limits treatment options and adversely affects survival. Increased awareness, a high index of suspicion and appropriate early referral is crucial to enable limb salvage surgery and increase disease-free survival rates.
Osteosarcoma is the most common malignant primary bone tumour in children and adolescents, and the second most common primary bone tumour overall, after multiple myeloma.1-6 With an estimated incidence of approximately 3 - 5 cases/million population per year, osteosarcoma has been classified as an orphan disease by the WHO.7
Prior to 1970, the overall survival rate of localised osteosarcoma was 10 - 20%.2,8 This survival rate has dramatically improved over the last 30 years, to 60 - 70% , as a result of improved chemotherapy regimens and surgical techniques.2,4,6,8 To benefit from these advances in treatment, the diagnosis must be made prior to progression beyond localised disease. Non-metastatic disease is currently curable in 60 - 70% of cases.5,6 However, osteosarcoma associated with systemic spread carries a much graver prognosis, with cure expected in less than 30% of cases.2,6
This study evaluated the clinical stage of osteosarcoma at presentation to our tumour unit. Particular emphasis was placed on the early signs of disease and radiological findings, to raise awareness among doctors who might be the first point of call for these patients and their families.
Methods
Between July 2009 and October 2011, 25 patients with suspected osteosarcoma were managed at our orthopaedic tumour unit. After complete workup and radiological staging, the diagnosis of osteosarcoma was confirmed with formal open incisional biopsy. Inclusion criteria were patients with histological diagnosis of osteosarcoma. Patients were excluded if their records were insufficient in terms of the required data. Patients' charts were reviewed and information extracted regarding clinical presentation, histological diagnosis and stage of disease.
Results
The records of 25 patients were reviewed; 24 (10 males and 14 females) met the inclusion and exclusion criteria (Table 1). One patient was excluded owing to insufficient data. The median age was 16 years (range 11 - 53 years).
Patients presented to our unit a median of 4 months after symptom onset. The most common presenting complaint was a swelling or mass (n=22) followed by pain (n=12) and constitutional symptoms (n=2). Pathological fracture at presentation was found in 3 (12.5%) patients.
Metaphyseal location around the knee was the most common anatomic site, with the distal femur being involved in 13 cases and the proximal tibia being involved in 10 (Fig. 1). The remaining case was located in the metaphyseal region of the proximal ulna.

Conventional osteosarcoma was the most common histological diagnosis and found in 22 out of 24 patients (91.6%); these were histologically subdivided into 20 osteoblastic and 2 chondroblastic osteosarcomas. The remaining 2 patients had histological diagnoses of periosteal osteosarcoma and dedifferentiated parosteal osteosarcoma respectively.
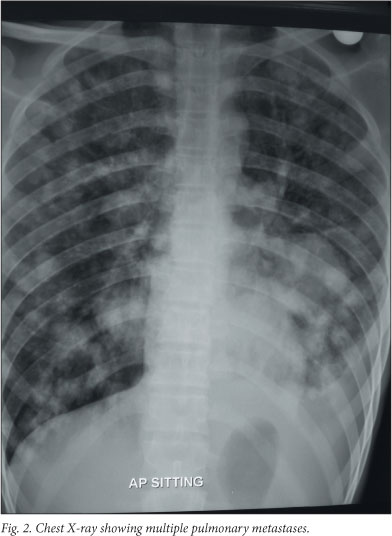
At presentation, 16/24 (66.7%) patients had metastatic disease (Table 1); metastasis to the lung was the most common site in 12/16 (75%) patients (Fig. 2); 5 had concurrent bony metastases; and 4 had bony metastases without radiological evidence of lung metastases.
Eight patients presented without any evidence of metastatic disease; 4 of them had advanced local disease, including large tumour mass with soft-tissue compromise, neurovascular encasement and pathological fracture. Limb salvage was performed in 2/8 patients who presented without metastatic disease, both of whom had a proximal tibial tumour, and underwent wide resection and megaprosthesis total knee replacement.
Three of the patients were older than expected for primary osteosarcoma, aged 40, 51 and 53 years, respectively. Two of these patients were HIV-1 infected; further research is being conducted to determine the causality, if any, between osteosarcoma and HIV-1 infection.
Discussion
Osteosarcoma is a primary malignant bone tumour that is characterised by the proliferation of malignant mesenchymal cells capable of the direct production of osteoid.3,4,6,9 The World Health Organization's histological classification further divides osteosarcoma into medullary and surface tumours, which are each divided into several subtypes. Conventional osteosarcoma (the high-grade medullary variant) is the most common subtype, making up about 90% of all cases,4,6 and was found in 91.5% of our cases.
Patients usually present during the second and third decades of life, 70 - 75% of patients being between the ages of 15 and 25 years.3,4,6,10 Our patients had a slightly wider age variance, with 70% being between the ages of 11 and 28 years. Lesions are typically located in the metaphyseal region of long bones, with the distal femur and proximal tibia making up approximately 50% of all cases.3-6,10,11 The tumour location in our patients was almost exclusively in the distal femur and proximal tibia.
Patients usually present with localised pain and swelling.2,6,10 The onset of symptoms is insidious, generally being present for several weeks before presentation. Most patients cite incidental trauma as the cause of their symptoms. Pain may be activity-related but typically also occurs during rest or at night. Constitutional symptoms include weight loss, pallor, fever and anorexia.6 At presentation, a limp, loss of function or decreased range of motion may be detected.3 The most common clinical finding is a mass that is invariably firm and tender. Erythema and venous distention are also frequently noted.3 A high index of suspicion must be maintained in every child or adolescent who complains of pain around the knee, irrespective of a trauma history.
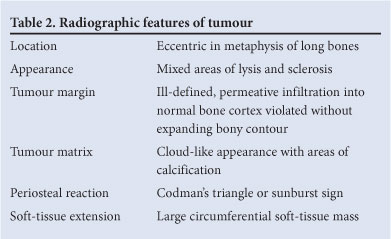
Plain X-rays are indispensable for diagnosis, and the clinical suspicion of osteosarcoma is often confirmed by plain radiographs.5 Typical radiographic findings of an aggressive bone-forming tumour with a periosteal reaction and extraskeletal soft tissue extension are present in 80 - 90% of cases (Table 2) (Fig. 3).2-4,6,11 Early osteosarcoma, however, can often be overlooked or mistaken for benign lesions.12

Therefore, computed tomography (CT) or magnetic resonance imaging (MRI) should be used when there is doubt as to the nature of a bony lesion in a child or adolescent. These modalities can show subtle aggressive features not apparent on plain radiographs.11 Most of our patients presented with locally advanced disease and classic radiographic findings.
Along with plain radiographs, CT, MRI, bone scintigraphy and occasionally angiography are used for diagnosis and staging purposes.6 MRI is used to delineate the extent of the tumour, plan biopsy and definitive surgery, and identify any possible skip lesions. CT scan of the chest and abdomen is performed to identify any visceral metastases, while bone scintigraphy should be done to rule out bony metastases.6,13 Where available, positron emission tomography fluorine-18-fluorodeoxyglucose (PET 18-FDG) may be used as an alternative staging modality.13
To confirm the diagnosis of osteosarcoma, a biopsy is always required.6 As with all suspected malignant bone tumours, the biopsy should be done in a specialised unit by the surgeon who will also perform the definitive surgery.5,6,14 Biopsy is preferably done open, through a longitudinal incision, without jeopardising possible future limb salvage surgery.2 The biopsy incision must be placed in an area where it can be totally excised at the time of eventual resection, to allow successful limb salvage surgery.5,6,14 All biopsies done at our institution are open incisional biopsies, and no postoperative wound complications were observed.
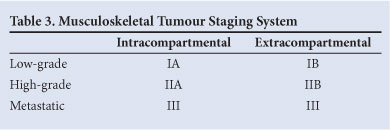
Once confirmed histologically, the definitive treatment decision is based on the stage of disease and prognosis. Staging is performed using the Musculoskeletal Tumour Staging System (Table 3),15,16 that is based on the histological grade, local extent, and presence of metastases. Multiple prognostic factors have been proposed including detectable metastases, advanced age, non-extremity location, large tumour volume, elevated LDH and ALP, and poor histological response to neo-adjuvant chemotherapy.6,8,17 Of these, only metastatic disease, tumour size >10 cm, and poor response to neo-adjuvant chemotherapy have consistently been associated with poor outcome.2,4,6,8,18
The primary surgical objective is complete resection of tumour tissue.1 Therefore, limb salvage and prosthetic replacement can only be considered if a viable, functional limb remains after resection. If limb salvage is considered, pre-operative neo-adjuvant chemotherapeutic treatment is instituted to facilitate the surgical dissection. If limb salvage is not possible, ablation of the limb may be performed.4 The literature reports limb salvage rates in excess of 80%,1,6,17 which was not possible in our patients as 20/24 (83.3%) patients presented with advanced disease precluding limb salvage surgery. Following surgical tumour excision, either through limb salvage or ablation, all patients are considered for postoperative systemic chemotherapy.
Conclusion
Owing to its relative rarity, osteosarcoma is unfortunately often missed on the initial visit to a local hospital. To improve the early recognition of osteosarcoma, a high index of suspicion, liberal use of radiographs and a sound knowledge of the subtle X-ray changes are needed. When faced with a suspected osteosarcoma, consultation with a referral unit that specialises in these diseases is advisable, as missed or late diagnoses could have catastrophic consequences.
The content of this article is the sole work of the authors. No benefits of any form were or will be received from a commercial party related directly or indirectly to the subject of this article. This research was approved by an ethics committee.
References
1. Ayerza MA, Farfalli GL, Aponte-Tinao L, Muscolo L. Does increased rate of limb-sparing surgery affect survival in osteosarcoma? Clin Orthop Relat Res 2010;468:2854-2859. [http://dx.doi.org/10.1007%2Fs11999-010-1423-4] [ Links ]
2. Federman N, Bernthal N, Eilber FC, Tap WD. The multidisciplinary management of osteosarcoma. Curr Treat Options Oncol 2009;10:82-93. [http://dx.doi.org/10.1007%2Fs11864-009-0087-3] [ Links ]
3. Klein MJ, Siegal GP. Osteosarcoma: anatomic and histologic variants. Am J Clin Pathol 2006;125:555-581. [http://dx.doi.org/10.1309%2FUC6KQHLD9LV2KENN] [ Links ]
4. Murphey MD, Robbin MR, McRae GA, Flemming DJ, Temple HT, Kransdorf MJ. The many faces of osteosarcoma. RadioGraphics 1997;17:1205-1231. [ Links ]
5. Phillip T, Brunat-Mentigny M, Carrie C, et al. Osteosarcoma. Br J Cancer 2001;84(2):78-80. [http://dx.crossref.org/10.1054%2Fbjoc.2001.1770] [ Links ]
6. Picci P. Osteosarcoma (Osteogenic sarcoma). Orphanet Journal of Rare Diseases 2007;2(6):1-4. [http://dx.doi.org/10.1186%2F1750-1172-2-6] [ Links ]
7. Ferrari S, Palmerini E. Adjuvant and neoadjuvant combination chemotherapy for osteogenic sarcoma. Curr Opin Oncol 2007;19(4):341-346. [http://dx.doi.org/10.1097%2FCCO.0b013e328122d73f] [ Links ]
8. Romeo S, Cleton-Jansen AM, Bovee JVMG, Hogendoorn PCW. Advances in bone and cartilage tumours. Applied Cancer Research 2005;25(3):108-115. [ Links ]
9. Huvos A. Bone Tumors: Diagnosis, Treatment, Prognosis. 2nd ed. Philadelphia: WB Saunders, 1991. [ Links ]
10. Chaudhary S, Singh D, Sen R, Deviraju C, Bhagwat K. Osteosarcoma of calcaneum. A case series of rare tumour presenting a diagnostic dilemma. WebmedCentral Orthopaedics 2010;1(12):WMC001273. [ Links ]
11. Rosenberg ZS, Lev S, Schmahmann S, Steiner GC, Beltran J, Present D. Osteosarcoma: subtle, rare, and misleading plain film features. AJR 1995;165:1209-1214. [ Links ]
12. DeSantos LA, Edeiken BS. Subtle early osteosarcoma. Skeletal Radiol 1985;13:44-48. [ Links ]
13. Meyer JS, Nadel HR, Marina N, et al. Imaging guidelines for children with Ewing sarcoma and osteosarcoma: a report from the Children's Oncology Group Bone Tumor Committee. Pediatr Blood Cancer 2008;51(2):163-170. [ Links ]
14. Geller DS, Gorlick R. Osteosarcoma - A review of diagnosis, management and treatment strategies. Clinical Advances in Hematology and Oncology 2010;8(10):705-718. [ Links ]
15. Wolf RE, Enneking WF. The staging and surgery of musculoskeletal neoplasms. Orthop Clin North Am 1996;27(3):473-481. [ Links ]
16. Enneking WF. A system of staging musculoskeletal neoplasms. Clin Orthop Relat Res 1986;204:9-24. [http://dx.doi.org/10.1097%2F00003086-198603000-00003] [ Links ]
17. ESMO Minimum clinical recommendations for diagnosis, treatment and follow-up of osteosarcoma. Ann Oncol 2005;16(1):i71-i72. [ Links ]
18. Bielack SS, Kempf-Bielack B, Delling G, et al. Prognostic factors in high-grade osteosarcoma of the extremities or trunk: an analysis of 1,702 patients treated on neoadjuvant cooperative osteosarcoma study group protocols. J Clin Oncol 2002;20(3):776-790. [http://dx.doi.org/10.1200%2FJCO.20.3.776] [ Links ]
Accepted 9 May 2012.
 Correspondence to:
Correspondence to:
NFerreira
(drferreiran@gmail.com)














