Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.101 n.12 Pretoria Dec. 2011
ORIGINAL ARTICLES
Assessment of routine laboratory screening of adult psychiatric patients presenting to an emergency centre in Cape Town
Andreas CredeI; Heike GeduldII; Lee WallisIII
IFCEM (SA). Joint Division of Emergency Medicine, University of Cape Town and Stellenbosch University, W Cape
IIFCEM (SA), MMed (EM). Joint Division of Emergency Medicine, University of Cape Town and Stellenbosch University, W Cape
IIIMD, FRCS, FCEM, FCEM (SA). Joint Division of Emergency Medicine, University of Cape Town and Stellenbosch University, W Cape
ABSTRACT
Our study suggests that routine laboratory screening provides no additional information to that obtained from a thorough history and clinical examination in patients at high risk of having an underlying medical cause of presenting psychotic symptoms.
Managing mental health patients forms part of the workload in emergency centres (ECs) throughout the Western Cape (WC), which has an estimated overall lifetime prevalence of mental health disorders of 39.4%.1 The Mental Health Care Act of 2002 requires that patients presenting with a mental health disorder and requiring involuntary or assisted admission be admitted to a designated hospital for 72 hours for assessment and treatment.2 Their entry point in most cases is via the EC, which places additional strain on emergency facilities. The high incidence of mental health disorders in adolescence, when many adult mental health conditions begin, is expected to increase because of increasing social stressors such as poverty, displacement and conflict in low-income areas.3 We can therefore expect an increasing human and financial resources burden on health care facilities.
Diagnosing mental health disorders in the EC is made more difficult because they can co-exist with medical conditions including HIV/AIDS, which itself can present with mental health disturbances. The prevalence of HIV/AIDS in the WC is estimated to be 5.3% in persons aged 15 - 49 years.4 Mental health disorders, specifically psychosis, can also be precipitated by recreational drugs. In the WC mental health (including substance abuse) is one of the top five contributors to the burden of disease, placing significant strain on local health care resources.5 Methamphetamine as the primary drug of abuse has increased from 0.3% in 2002 to 37.2% in 2006.6 This is likely to have increased the number of presentations of psychosis to ECs.
At the EC, patients with a mental health disorder are assessed by emergency medical personnel to exclude underlying medical causes that would explain their presentation, before being referred to mental health practitioners. The WC guidelines for investigation of psychiatric patients state that patients with a first presentation of a psychotic disorder must have a serological test for syphilis and an HIV test, with consent, if clinically indicated.7 Other tests should be done only if clinically indicated.7
This guideline has been expanded to recommend that patients with a psychiatric illness and low clinical suspicion of a general medical condition need only a clinical examination with basic observations and a random blood glucose level measurement in the EC before referral to the mental health services (patients >60 years also require urinalysis to exclude urinary tract infection).8 However, if there is high clinical suspicion of an underlying general medical condition, the following additional investigations are required:8 white cell count (WCC), serum sodium and renal function, haemoglobin (point of care test sufficient unless Hb <10 g/dl), chest radiograph, and additional testing as indicated by clinical examination.
Despite these guidelines, routine testing carried out in ECs in Cape Town includes WCC, serum sodium and electrolytes, syphilis serology, HIV testing and thyroid function testing. Such 'blanket screening' of patients who present with mental health disorders is unnecessary9-14 and places additional strain on hospital financial and personnel resources.
The justification for 'blanket screening' is to exclude medical diagnoses that may not be detected in a mental health institution14 and to detect treatable co-morbid medical conditions early. However, most missed medical cases are due to an inadequate history and clinical examination rather than failing to perform blanket laboratory and radiological investigations.14 The overall yield of routine blanket screening in the EC is very low.9 -14 There must be a clear rationale for performing tests, rather than ordering predetermined routine testing on all patients.11
Furthermore, some patients re-present frequently to the EC with acute psychosis, often resulting in multiple re-testing within a short period of time. This further increases cost to the health care facility and increases the risks (such as needle-stick injuries) to health care workers. Routine screening is warranted in 'high-risk' populations,12 including those at high risk of having a concomitant or primary medical illness that causes or exacerbates the psychiatric presentation (e.g. the immunocompromised, elderly, recreational drug users or persons from a poor socio-economic background).
High levels of substance abuse, a high HIV prevalence and the poor socio-economic background of much of Cape Town's population make the EC population a 'high-risk' one, and suggest that routine screening is necessary. A causal or contributory medical diagnosis in 24.3% of aggressive patients presenting to the EC was found in KwaZulu-Natal. However, their causes of aggression include diagnoses that could be detected on history and physical examination alone.15
We aimed to assess the utility of laboratory testing in acute psychotic presentations in the EC in Cape Town.
Materials and methods
We retrospectively reviewed records of all patients presenting to the EC of G F Jooste Hospital, Cape Town, with acute-onset psychotic symptoms from 1 January to 30 June 2009. Patients were identified through the EC register. A standardised data capture form documented date of presentation, sex, age, whether blood tests were conducted, which tests these were, and the results of these tests.
The results of the following laboratory investigations were extracted: syphilis serology, thyroid-stimulating hormone (TSH), WCC, serum sodium and creatinine, HIV status and lumbar puncture results. Additional tests performed on some patients that were not part of the routine screening tests were excluded. Only laboratory investigations performed in the EC were included.
Blood tests were regarded as being either normal or significantly abnormal (above the threshold for what the local psychiatric services considered as requiring further investigation).8 For sodium, creatinine, lumbar puncture and TSH results no threshold levels were available in the hospital mental health guidelines, so internationally accepted values considered abnormal and likely to contribute towards psychotic symptoms were used. Values for lumbar punctures, HIV rapid test, syphilis serology and thyroid-stimulating hormone were obtained as unpublished data from the National Health Laboratory Service at time of data collection. Table I presents reference ranges for determining significantly abnormal individual laboratory results in this study.
The case notes of all patients with significantly abnormal blood results were reviewed by the principal investigator to assess whether the abnormal blood test could have been predicted on clinical examination alone. Predictability was determined by the presence of a relevant history, abnormal vital signs or clinical examination relevant to the abnormal laboratory result. If the patient's medical history and the clinical examination led to suspicion of an underlying medical condition documented in the patient's notes, this was considered a result that could have been predicted without blood tests.
In EC case notes in which no final diagnosis or disposition plan was documented, admission notes from the relevant specialty were reviewed to determine the patient's diagnosis and management plan. This diagnosis was then accepted as the EC diagnosis with regard to determining whether the laboratory result was relevant in making this diagnosis. In case notes with multiple differential diagnoses, the admitting specialty's notes were reviewed to determine the discharge diagnosis. If this was within the differential diagnosis in the EC notes, it was accepted as the EC diagnosis on which relevance and predictability were assessed.
Patients who presented to the EC with psychotic symptoms but whose results were not found on the hospital laboratory computer system were considered not to have had laboratory investigations performed.
Laboratory results were entered into a Microsoft Excel spreadsheet and data were analysed using Stata 10.19
Ethics approval for the study was obtained from Stellenbosch University.
Results
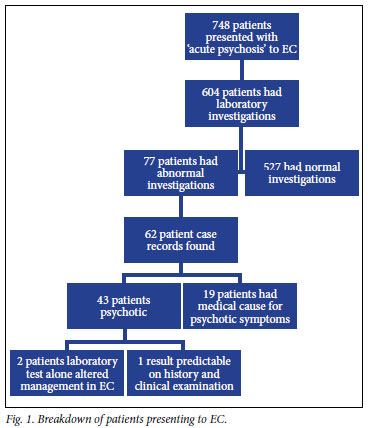
Seven hundred and forty-eight patients with psychotic symptoms were identified from the EC register of G F Jooste Hospital; 604 (80.7%) had laboratory investigations performed in the EC, and the median age was 29 years (interquartile range 23 - 38 years). In total 2 287 tests were conducted. Of the patients who had laboratory investigations, 67.4% were male.
The number of abnormal test results as a fraction of the total number performed was as follows: sodium 7/562 (1.2%), creatinine 2/590 (0.3%), WCC 53/584 (9.1%), HIV 7/58 (12.1%), lumbar puncture 20/68 (29.4%), rapid plasma reagin (RPR) 14/333 (4.2%), and TSH 0/92 (0%) (Table II).
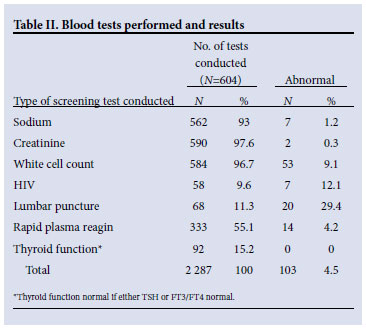
Patients with abnormal TSH values all subsequently had normal FT3 or FT4 values, so no patient had abnormal thyroid function. Of the 14 patients with reactive RPR tests, 4 had lumbar punctures performed in the EC, of which 1 was abnormal.
Almost one-third of lumbar punctures performed were abnormal according to the criteria in Table I. However, no lumbar puncture on its own changed the management and disposition of the patient.
Of the patients 132 had had one or more of the same laboratory tests performed in the previous 6 months. One patient had had laboratory tests performed five times in the period studied.
Of all patients with abnormal laboratory results (N=77), 62 case records were found; 43 had a final diagnosis of a mental health disorder, while 19 had a medical cause for their presentation of acute psychosis. Table III describes the number of patients whose final diagnosis could have been predicted through medical history, clinical examination or abnormal vital signs. Fig. 1 describes the number of patients for whom clinical management in the EC was altered directly as a result of these abnormal blood tests.
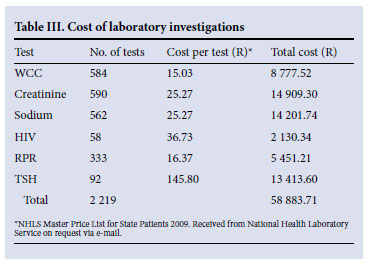
Although not designed to estimate the costs of these routine tests, some exploratory extrapolation was done to estimate their full financial burden on the health care system.
Table III summarises the estimated cost of tests performed, excluding lumbar punctures.
Discussion
Consistent with previous studies,9-14 our results suggest that 'blanket screening' of all psychiatric patients is unnecessary and wasteful of scarce resources in the WC public health care setting. Of patients who presented to the EC at G F Jooste Hospital with 'acute psychosis', 80.7% had blood tests taken to screen for underlying medical causes for their acute psychosis.
The rationale behind using laboratory investigations is to corroborate the findings of the patient's history and clinical examination, and a high yield of abnormal results is expected. However, of our 2 287 blood tests only 103 (4.5%) were abnormal. In only 2 (0.33%) of 604 cases did the abnormal result change the management of the psychotic patient. This suggests that these tests are conducted on most acutely psychotic patients without a clinical indication and not to corroborate evidence. This is consistent with findings that 61% of abnormal results discovered in screening tests for mental health patients resulted in no further action.12 Others have shown that that few (0.4 - 0.8%) screening tests were clinically significant.13
Of the abnormal laboratory results, 21% were considered to have been predictable from the patient's medical history and examination. The higher yield of positive lumbar punctures could be expected, as the decision to perform them was derived from the history and clinical examination and not routinely on patients presenting with psychosis.
Our findings clearly show that in most cases routine screening tests provide no information additional to that obtained on history and clinical examination. To limit the burden on public health care resources, clinicians should have confidence in their clinical expertise and use blood tests only to corroborate the clinical suspicion of an underlying medical disorder. The minimal information that screening tests add to the clinical examination alone cannot justify the large amount of money spent on them.
The diagnosis of neurosyphilis can be challenging in HIVpositive patients because of its rapid progression, even in the young population. However, its symptoms should be detected on a thorough history and clinical examination and asymptomatic patients should not be tested routinely.20 This would reduce the high number of false-positive syphilis tests21 and improve the unacceptably low yield (4.2%) of positive results even in this at-risk population.
High levels of recreational drug use in the population have been described as an indication for routine screening on 'acutely psychotic patients'.12 However, a quarter of metamphetamine users are under 20 years old (mean 24 years)6,22 and this age group is less likely than older patients to suffer from co-morbid medical illness and to have abnormal screening laboratory investigations.
This study was in a 'high-risk population' with a high HIV prevalence, high incidence of recreational drug use and low socioeconomic background,4,6,23 and provides unique information about a previously unstudied population.
Screening tests performed on acutely psychotic patients should also only be used when an underlying medical cause for the patient's condition is suspected. Our results suggest that even in a population regarded as at high risk of undiagnosed medical illness, in the acutely psychotic patient routine blanket screening is not indicated and does not aid in patient management in the EC.
Limitations
This study is a retrospective record review including only patients identified from the EC register, and a small proportion of patients with acute psychosis may have been missed due to not being recorded. However, this is unlikely to change the findings significantly. A single reviewer examined the folders of patients with abnormal results and decided which results were significant and clinically predictable. This may have added bias regarding which abnormal results were considered clinically significant. The study may not reflect practices at other health care facilities, as it was performed at a single health care facility.
References
1. Stein DJ, Seedat S, Herman AA, et al. Findings from the First South African Stress and Health Study. Policy Brief, October 2007. Tygerberg: South African Medical Research Council, 2007. [ Links ]
2. South Africa, Mental Health Care Act [online]. Government Gazette, 2002. http://www.info.gov.za (accessed May 2010). [ Links ]
3. Patel V, Flisher AJ, Nikapota A, Malhotra S. Promoting child and adolescent mental health in low and middle income countries. J Child Psychol Psychiatry 2008;49(3):313-334. [ Links ]
4. Shisana O, Rehle T, Simbayi LC, et al. South African National HIV Prevalence, Incidence, Behaviour and Communication Survey 2008: A Turning Tide among Teenagers? Cape Town: HSRC Press, 2009. [ Links ]
5. Corrigal J, Ward C, Stinson K, et al. Decreasing the Burden of Mental Illness. Western Cape Burden of Disease Reduction Project. 2007;4(7). http://www.hsrc.ac.za/research/output/outputDocuments/4599_ Corrigal_Deceasingtheburdenofmentalillness.pdf (accessed May 2010). [ Links ]
6. Pluddemann A, Myers B, Parry C. Fact Sheet - Methamphetamine, Alcohol and Drug Abuse Unit, Medical Research Council. http://www.mrc.ac.za//mrcnews/methamphetamine.pdf (accessed May 2010). [ Links ]
7. Baumann S, Pienaar W, Winkler G. Guidelines for Routine Screening Investigations of First Presentations to Psychiatric Services for Organic, Psychotic and Mood Disorders. Provincial Administration: Western Cape. Circular H 142/ 2002. Protocols for the Management of Mental Health Problems at District and Regional Hospitals: Protocol 4. [ Links ]
8. Sellar C. Appropriate special investigations for mental disorders in primary care. CME 2006;24(8):453-454. [ Links ]
9. Korn CS, Currier GW, Henderson SO. 'Medical clearance' of psychiatric patients without medical complaints in the emergency department. J Emerg Med 2000;18(2):173-176. [ Links ]
10. Lukens TW, Wolf SJ, Edlow JA, et al. Clinical policy: Critical issues in the diagnosis and management of the adult psychiatric patient in the emergency department. Ann Emerg Med 2006;47(1):79-99. [ Links ]
11. Vergare MJ, Binder RL, Cook IA, Galanter M, Lu FG. Practice Guideline for the Psychiatric Evaluation of Adults. 2nd ed. Arlington: American Psychiatric Association, 2006. [ Links ]
12. Thomas CJ. The use of screening investigations in psychiatry. Br J Psychiatry 1979;135:67-72. [ Links ]
13. Anfinson TJ, Kathol RG. Screening laboratory evaluation in psychiatric patients: a review. Gen Hosp Psychiatry 1992;14:248-257. [ Links ]
14. Reeves RR, Pendarvis EJ, Kimble R. Unrecognised medical emergencies admitted to psychiatric institutions. Am J Emerg Med 2000;18:390-393. [ Links ]
15. Saloojee S. Routine pre-admission screening for a medical illness in aggressive patients who required sedation in the emergency department - necessary or not? South African Journal of Psychiatry 2009;15(3):67-71. [ Links ]
16. Reddy P, Mooradian AD. Diagnosis and management of hyponatremia in hospitalised patients. Int J Clin Pract 2009;63(10):1494-1508. [ Links ]
17. Androgue HJ, Madias NE. Hypernatremia. N Engl J Med 2000;342(20):1493-1499. [ Links ]
18. Kwon KT, Tsai VW. Metabolic emergencies. Emerg Med Clin North Am 2007;25:1041-1060. [ Links ]
19. Stata Statistical Software: Release 10. College Station, TX: StataCorp LP, 2007. [ Links ]
20. Lee JP, Koo SH, Jin SY, Kim TH. Experience of meningovascular syphilis in human immunodeficiency virus infected patient. J Korean Neurosurg Soc 2009;46(4):413-416. [ Links ]
21. Goh BT. Syphilis in adults. Sex Transm Infect 2005;81:448-452. [ Links ]
22. Plüddemann A, Dada S, Parry C, et al. South African Community Epidemiology Network on Drug Use Monitoring Alcohol and Drug Abuse Trends in South Africa (July 1996 - June 2009). SACENDU Research Brief 2009; 12(2):3. [ Links ]
23. Bourne D, Matzopoulos R, Bradshaw D, et al. Institutionalising a mortality surveillance system in the Western Cape province to measure the burden of disease and the impact of preventive interventions. Final Report 2007. Western Cape Burden of Disease Reduction Project; 2(7). https://vula.uct.ac.za/access/content/group/91e9e9d8-39b6-4654-00ae-f4d74cba085f/CD%20Volume%202%20Mortality%20Surveillance.pdf (accessed May 2010). [ Links ]
Accepted 27 July 2011.
Corresponding author: A Crede (acrede@hotmail.com)














